Telehealth in ear (or tele-otology/tele-audiology) and hearing care has steadily increased as an area of both research and clinical interest over the past 15 years [1]. Driven by rapid advances in connected technologies and wide-ranging potential use cases, telehealth had a surprisingly slow and selective uptake into clinical practices. Barriers to clinical use of telehealth have included restrictive regulatory allowances and an inability to reimburse for services. As a result, despite technological advances, telehealth had not had widespread clinical uptake in ear and hearing care until the COVID-19 global pandemic. Telehealth was mostly reserved as an optional convenience available for some patients and mostly as part of rehabilitation support and remote fine-tuning of hearing aids. This article on telehealth in ear and hearing care by Professor De Wet Swanepoel expands on this field which is familiar territory for him. He was awarded the 2018 Olusegun Obasanjo Prize for Scientific Breakthrough and Technological innovation.
Hearing access in low- and middle-income countries
In low- and middle-income countries our work has advocated for telehealth-enabled services for more than a decade [2]. Estimates indicate more than 400 million people globally require hearing aids and, on a continent like Africa, up to 90% of affected persons are unable to access care [3].
With less than one hearing health professional for every million persons in Africa, existing models are vastly inadequate to address the required ear and hearing care and require innovative solutions. In response, my research interests have focused on developing new low-cost technologies and innovative telehealth-integrated service delivery models that are key to reduce the global burden of hearing loss [3].

Figure 1. Example of a lay health worker conducting hearing screening in Africa.
Over the years we have developed, implemented, and evaluated mHealth technologies within community-based service-delivery models in low-income communities [1]. Smartphone apps with calibrated headphones are enabling minimally trained persons (Figure 1) to offer accurate hearing tests using digitally inclusive user-interfaces and rigorous quality control (e.g., environmental noise monitoring). This type of technology allows for on-site quality control measures such as environmental noise monitoring and tracking the quality of test operators. Cloud-based data management further enables asynchronous remote support, referral, and follow-up [1].
“With less than one hearing health professional for every million persons in Africa, existing models are vastly inadequate to address the required ear and hearing care and require innovative solutions”
Smartphone otoscopy combined with validated AI-assisted classification of ear disease (hearScope, hearX group) can further support decentralised assessment for appropriate referrals. Lay health workers, for example, are able to deliver childhood screening in communities with integrated cloud-based data management, directing referrals through text messages based on geolocation. Evaluations have demonstrated that these lay and community health workers are able to deliver testing on par with school health nurses and other health professionals using these technologies [4].
No- and low-touch hearing care
In higher income countries, alternative telehealth-based services have been slower in the uptake pre-COVID-19. The pandemic, which shut down regular hearing health services during lockdowns and required rapid changes in subsequent service-delivery models has, however, escalated telehealth as a matter of safety first and foremost. As a result, telehealth has seen unprecedented growth with rapid evolution of technology options to support no- and low-touch services and widespread regulatory and reimbursement allowances increasing adoption [5].
During COVID-19 we focused on several ways to reduce contact, using validated digital approaches, including online hearing screening and self-test assessment kits that can be incorporated by audiologists and hearing clinics. Online hearing screening, using a digits-in-noise test paradigm, allows for a rapid two-minute screening that can refer patients for further care. This technology, available from the digital health company founded on these technologies, hearX Group (www.hearxgroup.com), has also been deployed for the World Health Organisation (WHO) screening app (hearWHO). We are currently exploring how to further differentiate failed screening tests into sensorineural and potential ear disease cases for direct referrals to medical or audiological care to minimise contact and optimise efficiency.
“Lay health workers are able to deliver childhood screening in communities with integrated cloud-based data management, directing referrals through text messages based on geolocation.”
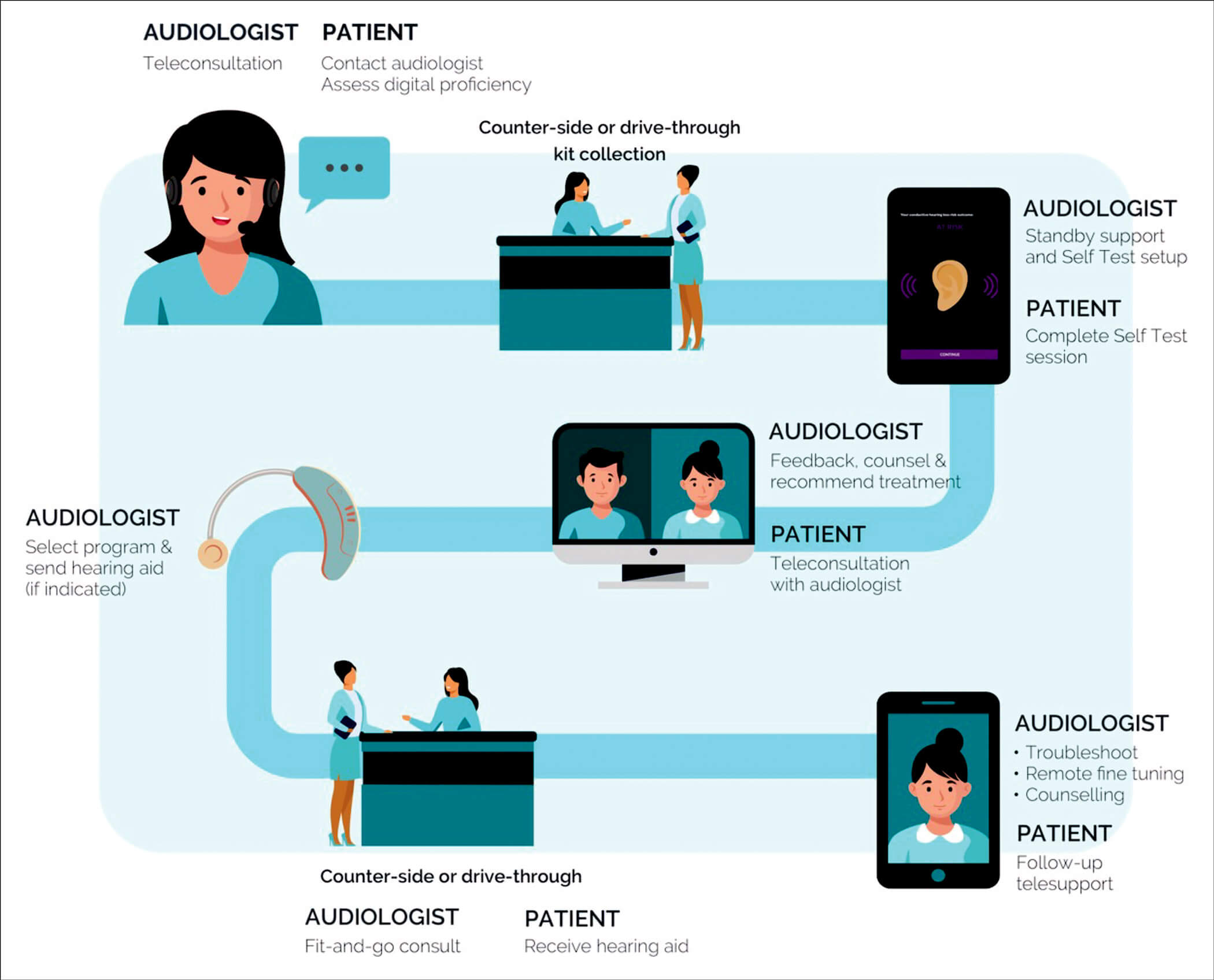
Facilitating hearing assessments for hearing aid fittings has been a particular challenge for the typical audiology patients who are mostly elderly and at highest risk of COVID-19 mortality and morbidity [5]. Traditional clinic settings have confined spaces (i.e., sound booths) with a variety of equipment used on patients during long appointments, all contributing to the risk of COVID-19 infection. We proposed alternative care pathways based on risk profile and patient preference that are no- or low-touch hearing assessments, using an innovative self-test kit supported by telehealth [5]. The self-test kit includes a tablet with calibrated headphones, facilitating a comprehensive hearing assessment that can be conducted at home or be incorporated into curb- or counter-side services (hearX group). Using self-testing to determine air conduction pure tone audiometry and speech-in-noise (digits-in-noise) thresholds informs a newly-developed algorithm to classify type of hearing loss with 94% accuracy [6]. This allows patients with sensorineural hearing loss to be treated using no- or low-touch services and those at risk of conductive hearing loss or ear disease escalated for advanced care (Figure 2).
Conclusion
During this rapidly changing landscape, hearing care professionals have an opportunity to rethink and reinvent the way they provide care. There are increasingly advanced and validated digital resources at our disposal to enable hearing professionals to continue serving patients supported through telehealth.
References
1. Swanepoel D. eHealth technologies enable more accessible hearing care. Seminars in Hearing 2020;41(2):133-40.
2. Swanepeol DW, Clark JL, Koekemoer, et al.Telehealth in audiology – the need and potential to reach underserved communities. International Journal of Audiology 2010;49(3):195-202.
3. Orji A, Kamenov K, Dirac M, et al. Global and regional needs, unmet needs and access to hearing aids. International Journal of Audiology 2020;59(3):166-72.
4. Dawood N, Mahomed-Asmail F, Louw C, Swanepoel D. mHealth hearing screening for children by non-specialist health workers in communities. International Journal of Audiology 2021; in press.
5. Swanepoel D, Hall J. Making audiology work during COVID-19 and beyond. The Hearing Journal 2020;73(6):20-4.
6. De Sousa KC, Smits C, Moore D, et al. Pure-tone audiometry without bone-conduction thresholds: using the digits-in-noise test to detect conductive hearing loss. International Journal of Audiology 2020;59(10):801‑8.




