In this article, the authors describe the importance of identifying aspirin-exacerbated respiratory disease in patients with chronic rhinosinusitis refractory to standard medical treatment. This can then open the door to considering aspirin desensitisation treatment which, in their hands, has proven successful in reducing both disease severity and the need for surgical intervention.
Aspirin-exacerbated respiratory disease (AERD, also known as Samter’s triad, is a chronic condition defined by asthma, sinus inflammation with recurring nasal polyps, and aspirin sensitivity.
It is estimated that up to 9% of adults with asthma and 30% of adults with both asthma and nasal polyps have Samter’s triad. Aspirin intolerance is underdiagnosed. When people with Samter’s triad are exposed to aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), they have an adverse reaction. The reaction includes both upper and lower respiratory symptoms.
“Studies have shown that up to 87% of AERD patients who undergo desensitisation and continue daily aspirin therapy show improvement in their sinusitis/asthma symptoms and need fewer polyp surgeries”
People with Samter’s triad will generally need to take medications daily to control their symptoms. They frequently have nasal polyp surgeries with early recurrences. Aspirin desensitisation, followed by long-term aspirin therapy is considered the gold standard treatment for AERD. The mechanism for aspirin desensitisation is not yet fully understood, but it is thought that small incremental dosages decrease leukotriene production, downregulate cysteinyl leukotriene receptors and decrease histamine and tryptase release from mast cells. Studies have shown that up to 87% of patients with AERD who undergo desensitisation and continue daily aspirin therapy show improvement in their sinusitis/asthma symptoms and need fewer polyp surgeries. Though varied protocols for aspirin desensitisation have been described, they all involve taking gradually increasing doses of aspirin until the patient can tolerate regular high aspirin strength without a reaction. Our protocol is as follows.
“The most common reactions that occurred in our patients during the challenge were rhinitis, asthma, GI symptoms and urticaria”
Diagnosis
Our diagnosis of AERD is based on history and oral aspirin challenge (OAC) test. Patients may give a history of an adverse reaction on the ingestion of NSAIDs, usually in the form of exacerbation of their asthma attack. In the absence of history, the oral aspirin challenge test remains the gold standard test.
OAC test Indications
Indications:
- Refractory Samter’s triad patients with a history of aspirin intolerance or a positive aspirin challenge test.
- Patients requiring COX-1 inhibitors for cardiovascular protection.
Contraindications:
- Uncontrolled bronchial asthma.
- Gastric ulcers.
- Pregnancy.
- Liver dysfunction.
- Bleeding disorders.
- Anticoagulation therapy.
Patients who have had previous systemic reactions to aspirin should not generally undergo aspirin desensitisation because of the risk of a fatal reaction.
Pre-challenge requisites
- Patients must undergo a full house FESS six-to-eight weeks prior.
- Patients must have lung function tests done prior and FEV1 should ideally be above 60%.
- Oral antihistamines are discontinued 48 hours prior.
- Patients may continue with their asthma medications
- Informed consent, explaining adverse reactions including asthma, urticaria, angioedema, angioedema, and status asthmaticus must be obtained.
Setting
We perform the OAC test under the supervision of one of our author consultants in an HDU hospital setting where adequate resuscitation facilities are available.
Hospital setting
Patients are admitted and an intravenous line secured before the challenge. Hourly peak flow measurements are recorded.
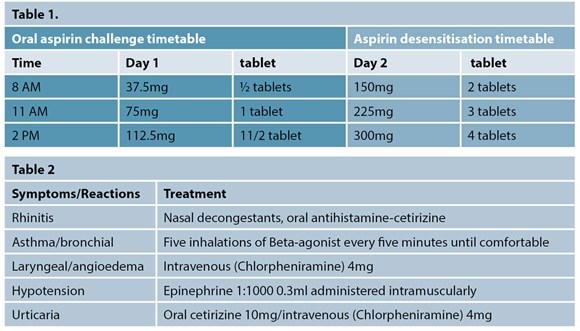
Patients are prescribed incremental escalating doses of aspirin as per the protocol in Table 1.
All patients were closely monitored for any adverse reactions and treated immediately and appropriately. The most common reactions that occurred in our patients during the challenge were rhinitis, asthma, GI symptoms and urticaria. Adverse reactions are treated as shown in Table 2.
Clinical parameters for positive aspirin challenge test
- Naso-ocular symptoms alone.
- A decline in peak flow (classic reaction).
- Lower respiratory reaction only with decline in peak flow.
- Laryngospasm with or without any of the first three reactions.
- Systemic reactions: hives, flushing, gastric pain, hypotension.
Our recommended continuation of daily aspirin therapy to maintain a desensitised state following a positive OAC test is as follows:
- Patients are advised to take 600mg of aspirin every day for two months and then taper down to 300mg/day.
- They are advised to take the 300mg aspirin medication every day for rest of their life.
- They are advised to take Omeprazole 20mg to reduce gastric irritation while on treatment.
- If they forget or fail to take aspirin, they are advised to recommence their medication within two-to-five days.
- If patients require any surgery in the future, they are advised to reduce their aspirin dose to a minimum dose of 100mg.
- Patients/GPS are advised to contact and take advice from the specialist before altering the aspirin dosage.
- Patients are followed up at three, six and 12 months thereafter. They are monitored for any adverse reactions such as gastric irritation or asthma symptoms, and for recurrence of nasal polyps
- Once desensitised, it is extremely important that the patients be maintained on regular aspirin therapy, because a break in therapy of one–to-five days can result in the patient returning to a sensitised condition.
So far in our institute, a total of 79 patients with a mean age of 46 years (male, 41; female, 38) and a diagnosis of AERD have undergone aspirin desensitisation. During the OAC, we did not have any patients developing severe reactions such as angioedema or anaphylaxis.
“Among our desensitised patients, aspirin desensitisation has shown a statistically significant beneficial impact on the number of surgical interventions, and medication requirements”
Among our desensitised patients, aspirin desensitisation has shown a statistically significant beneficial impact on the number of surgical interventions, and medication requirements. The degree of improvement varies in individuals, but most patients do experience significant benefit. Patients are usually compliant and those benefitting have found the treatment to be “life changing”. We plan to publish our more detailed experience in the near future.
Conclusion
Following excellent patient feedback, we as a team would encourage more suitable centres to offer this treatment to patients who would otherwise need to resort to further operations and perhaps future expensive biological treatments.
Further reading
1. Castells M. Desensitisation for drug allergy. Curr Opin Allergy Clin Immunol 2006;6(6):476-81.
2. Gollapudi RR, Terstein PS, Stevenson DD, Simon RA. ASA sensitivity implications for patients with coronary artery disease. J Am Med Assoc 2004;292(24):3017-23.
3. Stevenson DD, Simon RA. Selection of patients for ASA desensitisation treatment. J Allergy Clin Immunol 2006;118(4):801-4.
4. Slavin RG, Spector SL, Bernstein IL, et al. The diagnosis and management of sinusitis: a practice parameter update. J Allergy Clin Immunol 2005;116(6 Suppl):S13-47.
5. Stevenson DD, Simon RA. Selection of patients for aspirin desensitization treatment. J Allergy Clin Immunol 2006;118(4):801-4.









