In an attempt to improve the efficiency and flow of patients through a busy ENT clinic, technology now allows the ENT surgeon to consider biopsies in the outpatient setting on a more regular and controlled basis. This can avoid the need for an ‘examination under anaesthetic’ and can lead to a quicker diagnosis. The authors here describe how they do this in their unit for head and neck cases.
Advances in transnasal endoscopy, including the development of channelled nasendoscopes with distal chip optics, have allowed the development of awake, in-clinic procedures of the upper aerodigestive tract. Laryngeal biopsies have traditionally been done under general anaesthetic in an operating theatre environment. However, these procedures are increasingly being performed in the clinic environment in the awake, unsedated patient with use of topical anaesthesia and flexible nasendoscope technology.
In October 2018, Health Improvement Scotland published an advice statement stating that “outpatient biopsy offers the possibility of a more rapid diagnosis and allows selected patients to avoid biopsy under general anaesthetic in the operating theatre. The provision of outpatient biopsies is also likely to reduce laryngoscopy costs to the NHS…” [1]
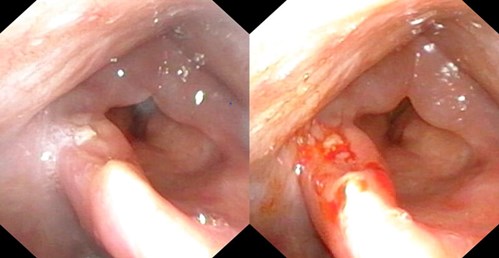
Pre and post biopsy.

Nasal anaesthesia.
Whilst some surgeons have reservations with regards to this technique, due to the reduced sensitivity and specificity of 71% and 97% respectively when comparing in-clinic biopsy with biopsy under general anaesthetic in the operating theatre, we feel this is a valuable technique which can expedite diagnosis and treatment in patients and is proven to be safe and cost effective. In our patients, the procedure is well tolerated and, in many cases, preferred to general anaesthetic biopsy. We utilise this technique for selected patients in the biopsy of suspected malignancy, suspected benign pathology of the larynx and in the surveillance of dysplastic lesions with the aid of narrow band imaging.
“This is a valuable technique which can expedite diagnosis and treatment in patients and is proven to be safe and cost effective”
Pre-procedure preparations
Patients are counselled with regards to the procedure and possible complications, including discomfort, epistaxis, failure of procedure and need for further treatment. A consent form is signed and filed in the patients’ case notes.
Materials
- Cotton wool soaked in lidocaine hydrochloride 5% and phenylephrine hydrochloride 0.5% topical solution
- Epidural catheter (Portex 18G Epidural, System 1 Clear Catheter, Smiths Medical, UK) and 5ml 1% lignocaine
- Channelled flexible naso-laryngoscope (ENF-VT3 Rhino-Laryngoscope, Olympus, Japan)
- Biopsy forceps (EndoJawTM Alligator jaw-step fenestrated 1.9mm FB-211D, Olympus Medical Systems Corp, Japan)
- Pathology specimen container and preservative

Transnasal equipment.
Procedure
The procedure is performed in either the outpatient clinic or the ward treatment room with the patient sat in an examination chair. The nose is examined and the most appropriate side is then packed using cotton wool soaked in lignocaine and phenylephrine topical solution. This is left in-situ for 10 minutes. The packing is removed and the ported scope is introduced. Further topical anaesthesia is administered via an epidural catheter placed down the endoscope channel. This allows further administration of 1-2% lignocaine under endoscopic guidance to the nasopharyngeal surface of the soft palate and the larynx.
The patient is instructed to make a prolonged ‘e’ sound to allow laryngeal gargling of the topical anaesthetic if the vocal folds are to be biopsied. After visualisation of the lesion, biopsies are performed using the flexible biopsy forceps (EndoJawTM Alligator jaw-step fenestrated 1.9mm FB-211D, Olympus Medical Systems Corp, Japan) which are passed down the endoscope channel. The biopsies are taken under endoscopic guidance by pushing the open jaws into the lesion, closing the jaws and pulling back swiftly on the forceps whilst holding the endoscope steady.
The specimen is then transferred into the pathology specimen container. Multiple biopsies can be taken using this method. Images were displayed using a video processor (CV-170, Olympus, Japan) which, in our case, allows both white light and narrow band imaging modalities. Photographs are taken pre and post biopsy and these are stored in the patient’s notes. There is also the facility to video record the procedure.
Postoperative procedure
The patient is observed for 15 minutes post procedure before being discharged home if well. The patient is instructed to remain nil by mouth for one hour from the administration of topical anaesthesia and to take care when first consuming liquids to ensure they do not aspirate.
“The patient is instructed to make a prolonged ‘e’ sound to allow laryngeal gargling of the topical anaesthetic if the vocal folds are to be biopsied”
Complications
A number of studies have reported on the complications from awake transnasal laryngeal biopsy. Complications are rare with published rates of 0-2.6%, the vast majority of which were self-limiting and include epistaxis, aspiration event and haematoma. There has been one reported case of supraglottic oedema resulting in the need for tracheostomy [2].

Transnasal biopsy.
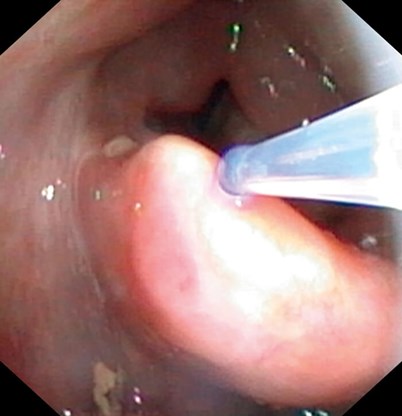
Drip catheter.
Conclusion
Awake transnasal biopsy of the larynx and pharynx is being performed by an increasing number of centres and practitioners. It is a well-established procedure in many countries and has been shown to be safe and effective. We believe the use of this technique will increase in the future which could lead to cost savings and a reduction in time to diagnosis/time to treatment for patients with lesions of the larynx and pharynx.
Patients do need to be counselled that the rate of non-diagnostic/unsatisfactory biopsy is greater than the traditional in-theatre general anaesthetic biopsy and that some patients may require a general anaesthetic procedure to obtain adequate tissue for diagnosis.
We have performed in excess of 50 of these procedures and have not encountered any major complications. Patient feedback has been positive, with patients especially pleased with the limited disruption to their day to day life in relation to avoiding the need for admission, preoperative assessment and general anaesthetic. We have found that adequate nasal anaesthesia is the key step to minimising discomfort for the patient.
References
1. Outpatient biopsy for the diagnosis of suspicious lesions of the larynx, pharynx and tongue base? Health Improvement Scotland, Evidence Note Number 84; August 2018.
2. Wellenstein DJ, de Witt JK, Schutte HW, et al. Safety of flexible endoscopic biopsy of the pharynx and larynx under topical anaesthesia. Eur Arch Otorhinolaryngol 2017;274(9):3471-6.






