In this article, the authors describe their ingenious technique to produce affordable yet realistic simulation models for some common ENT procedures.
The use of surgical simulation in otolaryngology training has significantly increased in recent years. This is most likely due to combination of factors, including increasing pressures on efficiency in the operating room, reduced trainee working hours, and an emphasis on patient safety [1].
Traditionally, surgical simulation has primarily depended on the use of human and animal cadavers, but there is increasing use of alternative technologies such as virtual and augmented reality (VR/AR) [2]. Whilst these modes all offer an effective learning environment, their use may be somewhat limited by cost. Ideally simulation opportunities should be accessible locally, and the use of low-cost models provides an opportunity for this to become a reality. In practice, a low-cost simulation model can be posted to training surgeons at their local trust and used alongside simple training kits.
In recent years we have designed and tested several low-cost, high-fidelity otolaryngology simulation models for the simulation of anterior ethmoidal artery ligation, periorbital abscess drainage, and quinsy drainage [3].

Figure 1. Construction of periorbital abscess models.
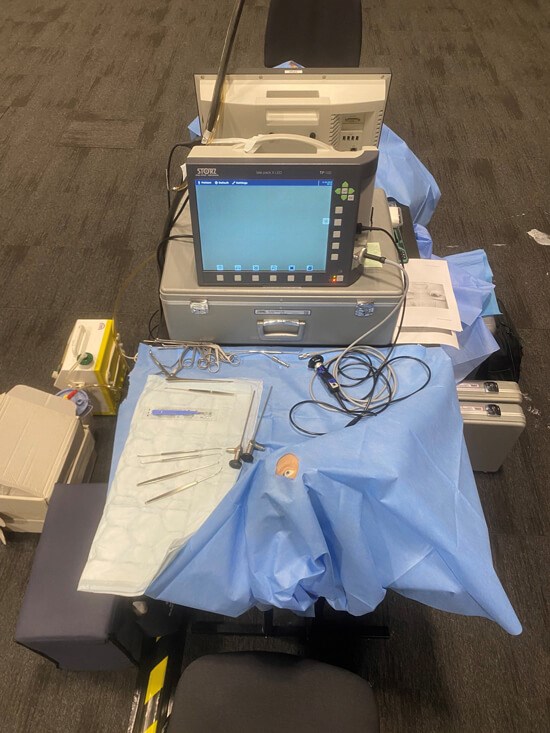
Figure 2. Periorbital abscess drainage model in situ for teaching at ESPO 2023.
Building the models
For the rhinology models, each was comprised of half a skull cast from plaster combined with rubber soft tissue components: skin, orbit, rectus muscles, periorbita and periorbital fat (Figures 1-2). A custard-filled water balloon was used to replicate the abscess, and electrical wire used for the ethmoidal arteries, inserted at their often-cited distances 24mm then 12mm posterior to the lacrimal crest (24-12-6 rule). The estimated cost of each model was £10 in materials, though this does not account for the labour of construction. The estimated cost of each model was £25 accounting for cost of materials and the labour of construction.
For the quinsy model, the base was sculpted from clay, the tongue from a simple dish sponge to allow depression, the soft tissue over the abscess from latex, and the abscess again from a custard-filled water balloon (Figures 3-4).
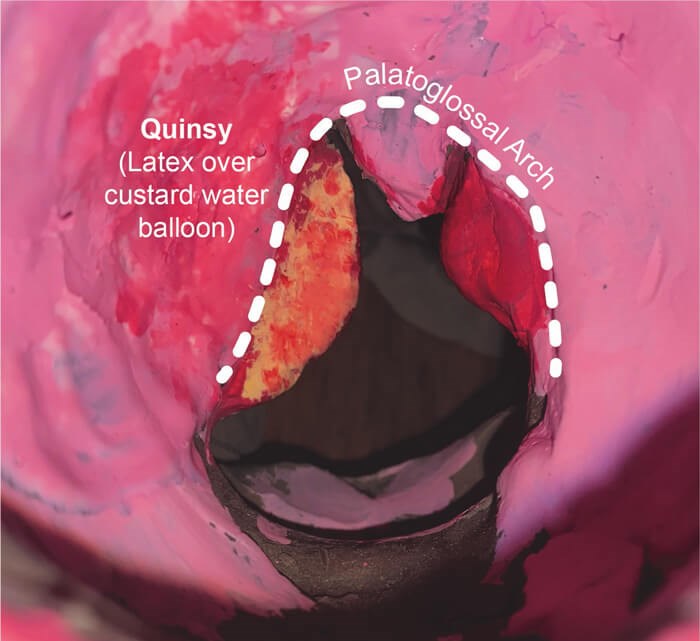
Figure 3. View of quinsy for drainage.
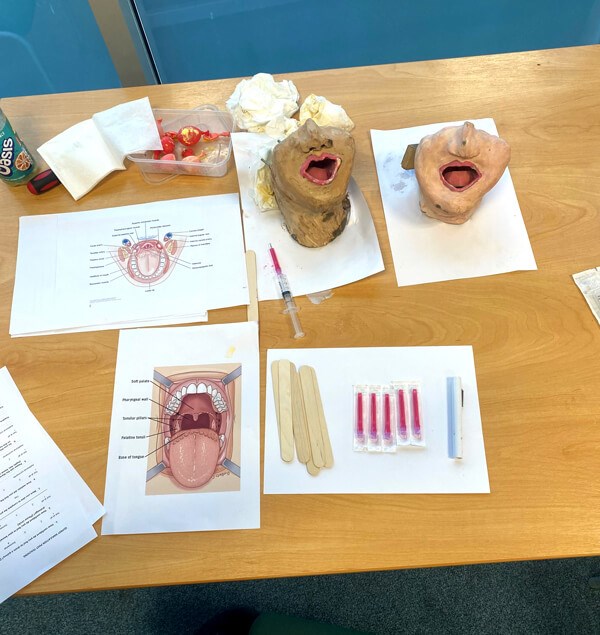
Figure 4. Quinsy model drainage station.
Feedback
The models have been implemented at a range of teaching environments for otolaryngology trainees. Each rhinology model was first trialled as an OSCE station for the North-West otolaryngology trainees’ (ST3-ST8) formative exam. Of those that used the SPOA model, 80% liked the anatomy of the model, 60% felt more confident to drain a SPOA on patients, and 60% thought the model increased their anatomical knowledge.
Most of the surgeons using the anterior ethmoidal artery ligation model were carrying out the procedure for their first time, highlighting its rarity in practice. Similarly to the SPOA model, the accuracy of the anatomy and likeness to human tissue were both ranked highly (means of 5 and 4.93 respectively on a Likert scale of 1-7), and most surgeons supported the hypothesis that the model would provide a benefit to their ability to carry out the procedure (5.53 on a Likert scale of 1-7).
The quinsy drainage model was trialled as a station for a training day for second-year core surgical trainees (CT2) in the North-West. Feedback was again provided from a questionnaire with ratings on Likert scales of 1-7. Each of the trainees had performed the procedure several times. The confidence in their anatomical knowledge, and ability to carry out the procedure were assessed prior to and following the teaching, and both increased (means of 5 to 7, and 5 to 7 respectively). The realism of the anatomy and ability of the model to improve their confidence were also both scored highly with means of 6.3 and 6.2 respectively.
Discussion and future work
The highly positive feedback that our models have received suggested a high benefit to the training of otolaryngology surgeons. These models are not only low-cost but are also mostly re-usable, aiming to reduce the waste of resources in the field of surgical training. Whilst impressive technologies exist for many surgical simulations, there may be an argument for further exploring the cost benefit of simple anatomical models such as these.
The periorbital abscess models have since been repeated and were recently used at ESPO 2023 to teach this procedure. In the future we would like to continue to develop low-cost simulation models and strive for the adoption of consistent surgical simulation opportunities nationwide.
Click the image belowto view a short clip of the endoscopic view of the abscess model in use.
References
1. Alwani M, Bandali E, Larsen M, et al. Current state of surgical simulation training in otolaryngology: systematic review of simulation training models. Arch Otorhinolaryngol-Head Neck Surg (AOHNS) 2019.
2. Arora A, Lau LY, Awad Z, et al. Virtual reality simulation training in otolaryngology. Int J Surg 2014;12(2):87-94.
3. Yapp J, Sebastien R, Khwaja S. A Low-Cost Prosthetic Orbital Simulation model for Endoscopic Anterior Ethmoid Artery Ligation. J Laryngol Otol 2023;1-6.
Declaration of competing interests:
1C Fees for use the of the construction and use of the periorbital abscess model have been paid for education at several conferences.