Background
The commonest active management of a pharyngeal pouch is the division of the “interparty” wall using a stapling device [1, 2]. The technique is relatively straight forward to perform and theoretically should have less complications than other techniques such as an “external approach”. Unfortunately the success of the technique is not universal as in a proportion of patients the stapling device cannot be deployed or it may fail to resolve symptoms. In these circumstances revision surgery is contemplated. This could be repeat stapling, an external approach or CO2 laser division of the interparty wall.
An external approach has fallen from favour due to a significant level of complications and morbidity. The CO2 laser is still used in some centres as an alternative to stapling. It has the advantage of being able to be used in cases with difficult access, using the ‘ultraslim’ endoscope and in revision cases where division of residual cricopharyngeal fibres can be confirmed.
The Cases
Case 1
Seventy-three male, of good general health presented to another centre two years previously with a history of regurgitation of foodstuffs and dysphagia. A pharyngeal pouch was confirmed on barium swallow. He underwent stapling of a large pharyngeal pouch without adverse effects. Initially he had a good result but deteriorated gradually over the next few weeks. A further stapling was performed. Again he made a good initial response but then deteriorated over several weeks. On presentation to our team he was maintaining his weight but concerned about the recurrence of his symptoms. In view of his previous unsuccessful repeat stapling it was decided to proceed to a CO2 laser Dohlmans procedure. At surgery the interparty wall fibres of cricopharyngeus muscle were seen with staples around them forming the persistent interparty wall. This was successfully divided using the CO2 laser. He subsequently had complete resolution of his symptoms with no recurrence at his discharge 12 months later.
Case 2
Fifty-seven male, overweight, with gastro-oesophageal reflux disease. He had undergone two previous stapling procedures in another hospital. Following the second procedure a pharyngeal leak was noted and treated conservatively. Unfortunately this left him with a ‘neuralgic’ throat and neck pain in the distribution of the cervical plexus and glossopharyngeal nerves. He presented to our care with a recurrence of his original swallowing problems in addition to the new symptoms of neuralgic pain. He underwent an endoscopic examination that revealed a persistent cricopharyngeal bar. At surgery the persistent cricopharyngeal fibres with staples in the mucosa were seen. These fibres were successfully divided using the CO2 laser. Postoperatively he did well and was discharged on a normal diet at 48 hours. No further swallowing problems were encountered and in addition to his swallowing improvement he had a reduction in his neck pain. Unfortunately his glossopharyngeal nerve pain is unchanged for which he attends the “chronic pain clinic”.
Case 3(BD)
Fifty-seven male, generally fit and well. Presented with a known diagnosis of pharyngeal pouch, confirmed by barium swallow. He was very symptomatic and had been seen previously in another institution for a pouch stapling which had to be abandoned. This was as a result of difficulty in access due to his long thin neck and a full dentition, which prevented access to the postcricoid region with either the endoscope or the stapler. Using the “Ultraslim” diverticuloscope it was possible to divide the interparty wall using the CO2 Laser. After nine months he is now swallowing normally.
Discussion
Although stapling techniques are successful in the vast majority of patients with Zenkers diverticulum there is a significant group of patients in whom there are access difficulties or need revision surgery.
The Weerda diverticuloscope used in stapling, is a fairly bulky instrument (Figure 1) and can be difficult to deploy satisfactorily when demonstrating the pouch or the full extent of the “inter-party” wall. This can be due to a combination of the patient’s dentition, neck stiffness or tongue base anatomy. In comparison the “ultraslim” CO2 diverticuloscope (Figure 2) is narrower, and as such it is often possible to demonstrate the surgical anatomy even in those patients in whom oesophagoscopy is difficult.
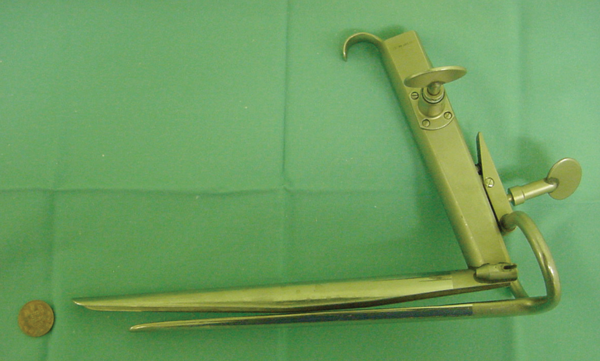
Figure 1: The Weerda Laryngoscope.

Figure 2: The “Ultraslim” CO2 Diverticuloscope.
In those patients in whom revision surgery is contemplated the issue is frequently the persistence of fibres of the cricopharyngeus muscle. As these can be displayed clearly during the CO2 Dohlmans procedure complete division can be achieved and confirmed visually (figure 3). In these cases a further advantage of using the CO2 laser is that it is possible to avoid previous staples by aiming between them.
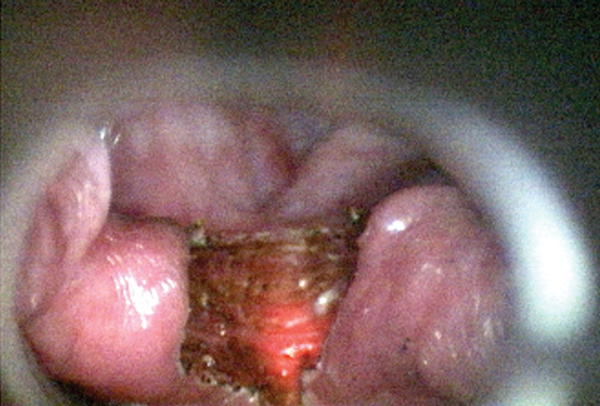
Figure 3: The Appearance of Cricopharngeus muscle during a Laser Dohlmans.
The main concern about the Dohlmans procedure is the risk of a pharyngeal leak and subsequent sepsis. This is overcome with a sealed row of staples in the endoscopic stapling procedure, this can also be obtained by augmenting the coagulum seal at the end of a CO2 laser Dohlmans procedure by applying one of the tissue glues such as TISEAL™.
Since its introduction, the technique of endoscopic stapling has revolutionised the management of pharyngeal pouches. Despite its success, however, there is still a cohort of patients where it is not an appropriate procedure and it is for this select group we would recommend consideration of the CO2 Laser Dohlman technique.
References
1. Siddiq MA. Sood S. Current management in pharyngeal pouch surgery by UK otorhinolaryngologists. Ann R Coll Surg Engl 2004:86(4):247-52.
2. Collard JM. Otte JB. Kestens PJ. Endoscopic stapling technique of esophagodiverticulostomy for Zenker’s diverticulum. Annals of Thoracic Surgery. 1993:56(3):573-6.






