The effectiveness of surgical technique and satisfactory outcome is greatly dependent on good surgical exposure. Retraction requires adequate traction and counter-traction of tissues in order to expose the tissue or organ under scrutiny for the surgeon. This is a universal component of surgical technique that spans across all surgical specialties. Rohit Gohil and Rodney Mountain tell us more.
In order to gain satisfactory retraction, a number of factors must be taken into account. Firstly, the degree of retraction should be such that no untoward damage is caused to the structures under tension. Secondly, the line of sight must be optimised for the operating surgeon, taking into account adequate illumination from theatre lighting.
The location of the retractor, and its method of retraction, along with the force applied to tissues and direction of tension will optimise exposure. The degree of surgical exposure achieved improves with greater application of force, but this should be balanced to minimise tissue damage and resultant unacceptable scarring.
The responsibility of retraction is usually that of the surgeon’s assistant. The current use of handheld metal retractors has its limitations in terms of ergonomics and access to the surgical field. This can limit the assistant’s view and their ability to perform effectively. The assistant can also become fatigued by periods of static retraction.
This has resulted in the development of a variety of retraction devices best tailored for their respective specialties: with regards to the structures being retracted and the nature of access required. These can be broadly divided into: handheld metal retractors; self-retraining retractors; compliant retraction and laparoscopic retraction (see Table 1) [1].
The training of a junior surgeon in their craft depends upon them being guided though the operation in question by their trainer – usually a consultant or senior trainee. Most procedures are usually taught in a stepwise manner where the trainee firstly observes a stage or procedure, before moving onto performing this at reducing degrees of supervision until they can be deemed as proficient. Progress can be evidenced by the trainee through platforms such as the Intercollegiate Surgical Curriculum Programme workplace-based assessments throughout their training [2,3].
Unfortunately, there are ever-growing problems with this mode of teaching with demands placed upon the trainee and trainer’s time by the European Working Time Directive (EWTD) [4,5,6]. This limits the total exposure that a trainee will get to operative practice prior to their completion of training. Exposure is also dependent upon patient load with particular conditions, which can be limited based on their trainer’s practice. This means that the trainee must be deemed to be safe at performing key procedures in a reduced timeframe. Alternatives can include training courses and cadaveric dissection, for example, but this is of limited value unless implemented thereafter in a live clinical setting.
Therefore, it is important that the trainee gains as much in-theatre training with their trainer and progresses efficiently. We have found that the use of elasticated retractors in open head and neck surgery may confer an advantage for the training of junior surgeons, especially with regards to the nature of this retraction method and the exposure achieved. We also describe how this improves the trainee / trainer dynamic, allowing efficient development of the trainee’s skills, complementing their educational needs and the theatre dynamic.
Elasticated retraction
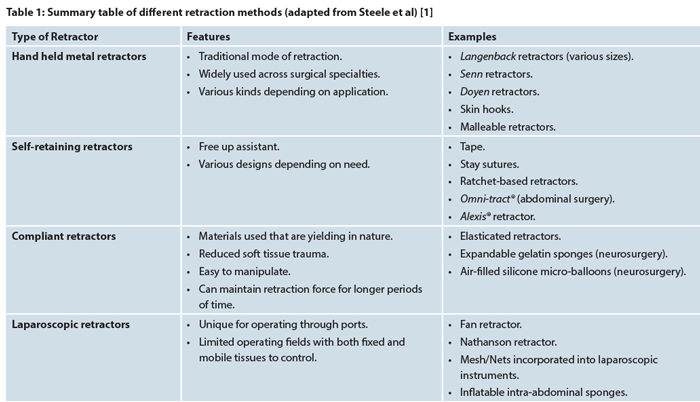
Elasticated surgical retractors are grouped into the class of compliant surgical retraction. They are composed of a metal hook embedded in a body of elastic. This elastic continues as a free length that can be stretched and attached to drapes or other application systems (see Figure 1) [7].
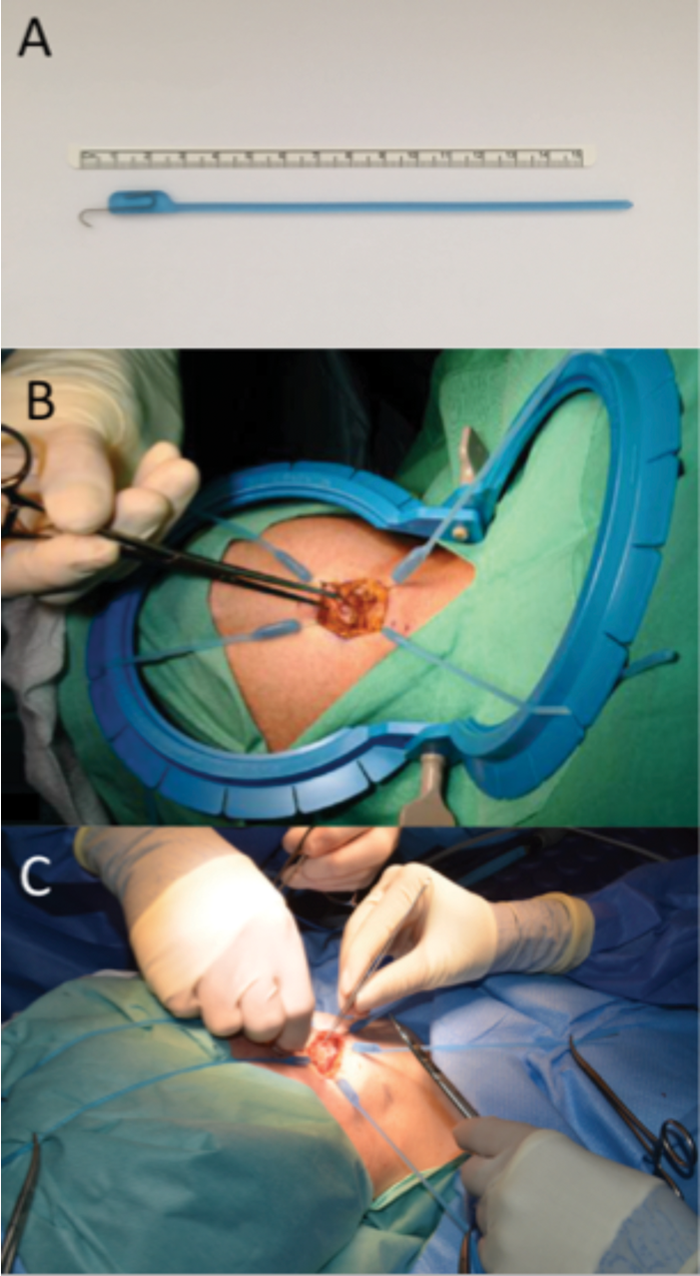
Figure 1: (A) Photograph of an elasticated retractor. (B) Photograph showing the use of four elasticated retractors applied to a disposable retractor system. (C) Photograph illustrating the application of elasticated retractors directly onto the surgical drapes.
Elastic as a material confers several benefits for retraction. When stretched and secured, it can maintain its elastic force in the desired direction without fatigue for long periods of time. As the procedure progresses, the force can be manipulated and directed elsewhere as needed. The constant static retraction force means that an assistant may not be required, or can be free to perform other tasks. The constant and efficient, yet dynamic, retraction provides an unimpaired and optimised surgical exposure. The resulting field can even be adequate for solo operating [1].
Elasticated retraction has been adapted for use in a variety of surgical specialties including urology, gynaecology, general and vascular surgery. Head and neck procedures - including neck dissection, parotidectomy, thyroidectomy and tracheostomy - have also been performed using this retraction method by ENT, maxillofacial and plastic surgeons alike. [8,9,10,11,12]
The use of elasticated retraction has vastly improved surgical exposure through a limited incision compared to the established use of handheld retractors (e.g. Langenbacks retractor). Once elasticated retractors are applied to the wound and secured peripherally, a circumferential force is applied to the edge. The resultant exposure is wider than the oblong field created with Langenbecks. As these retractors are smaller, more can be added without obscuring the surgical field (see Figure 2). Circumferential retraction also divides the force applied to tissues, preventing localised damage to skin and deeper structures.
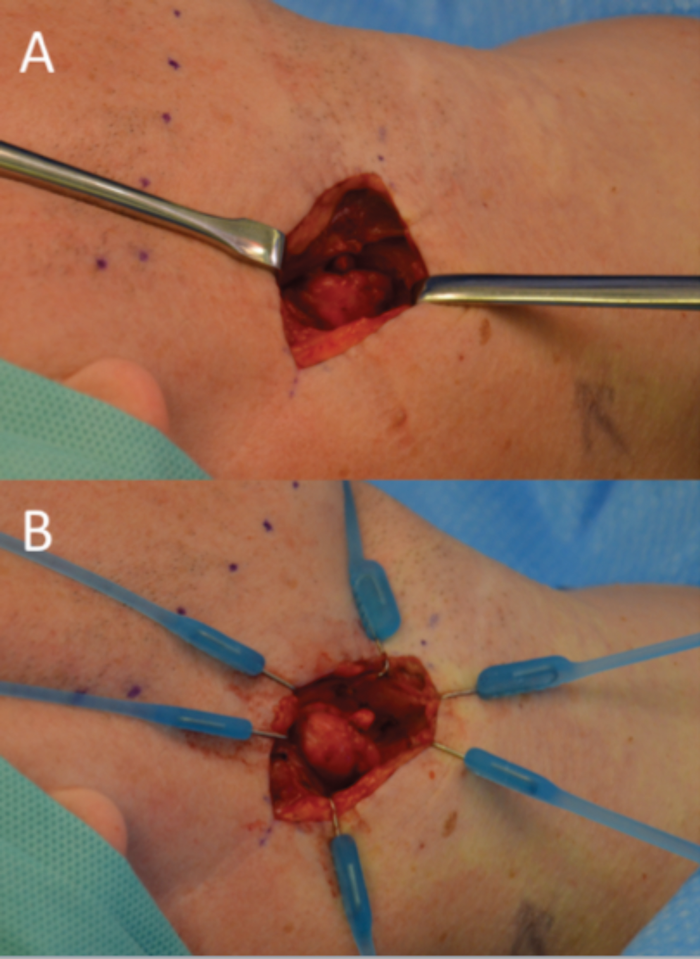
Figure 2: (A) Through the same incision traditional Langenbecks handheld retractors have been placed to expose a lesion. (B) However, the application of six smaller elasticated retractors applies a circumferential force with greater resultant exposure with a fraction of the force applied to the retracted skin.
As the procedure progresses and deeper tissues are encountered, the retractor hooks can be applied to them. Through a manoeuvre of eversion and lateral retraction, these structures are brought closer to the surface for better exposure, illumination and visualisation (see Figure 3). In this respect, deeper and more difficult stages in procedures such as tracheostomy can be made more manageable for the surgeon. The smaller size of elasticated retractors means they can also be easily removed from the wound once the tracheostomy is in place [13].
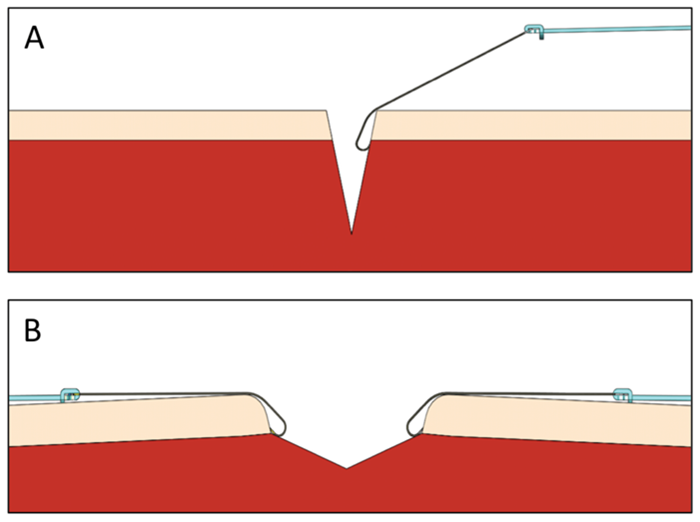
Figure 3: (A) In order to access deeper structures through an incision, elasticated retractors are applied to deeper planes / structures. (B) With effective traction and counter-traction, an eversion / lateral retraction force is applied, bringing deeper structures superficially for greater access.
Elasticated surgical retractors can be considered to be more versatile than other methods of retraction - for example, when in use they can retract a variety of soft tissues with equal efficacy. Other methods would require the assistant to handle a range of different retractors dependant on stage and tissue (i.e. Senn ‘cats paw’ retractors and large or small Langenbecks).
There are limitations associated with elasticated retraction. Haptic feedback is lost, but is essential in handheld retraction. Therefore it is possible to unwittingly apply a downward pressure to the skin surface for prolonged amounts of time with a potential for skin ischaemia – however we have not experienced this in practice. The introduction of a number of sharp instruments into the field also requires the surgeons’ vigilance in order to avoid needlestick injuries. In unique cases, the retractors may not provide complete exposure due to the limited properties of elastic and may need to be complimented with other retraction methods [14]. These retractors are also disposable and, therefore, additional cost is incurred in their one-off use.
The trainee / trainer dynamic
The process of becoming competent in operative surgery requires guidance from a trainer. This is a long process, usually beginning with an introduction to the basic stages of a procedure, progressing to being able to perform the procedure independently - i.e. competence. This theatre-based training forms a backbone to all surgical training, which is complemented by additional exposure in the form of craft courses and other educational activities. Unfortunately, total in-theatre exposure has been limited by the constraints of the EWTD [5].
The role of a trainer is therefore an important one and it is readily accepted that in order to provide first-class training, the trainer must be able to adapt to a changing profession and clinical landscape [15].
We have found that the use of elasticated retractors can make real-time training more efficient for both trainee and trainer - thus allowing the trainee to progress at a faster rate, but safely under the full guidance of their trainer.
The dynamic, stable retraction provided for a longer period of time allows for solo operating, leaving the assistant free to observe or perform additional tasks. If the trainer was guiding the trainee through an operation, they would now be able to stand on the same side as the operating trainee. Both would have the same view of the operative field and the same intensity of illumination. Therefore, the trainer would be better positioned to give efficient guidance and feedback (see Figures 4 and 5). The more efficient position of the trainer also allows them to assist in more difficult stages if necessary, whilst also being able to actively guide the trainee with very little obstruction of either’s view.

Figure 4: The use of elasticated retractors allows the trainee to become the solo operator, with the trainer free to supervise and assist from the same side. The trainee can therefore develop their operative skills more efficiently in a supervised environment.
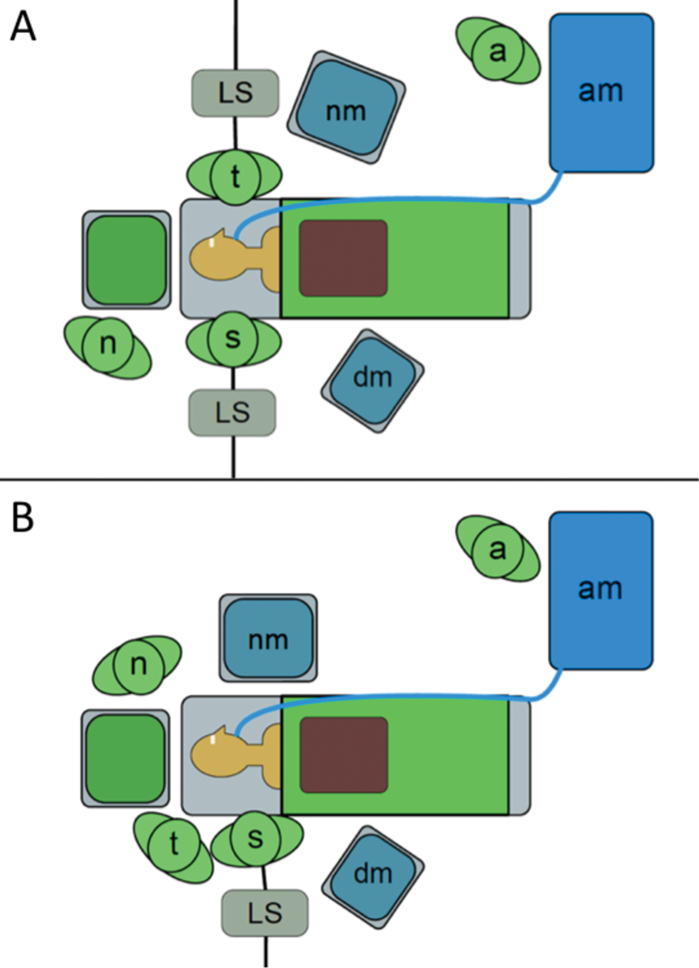
Figure 5: Plan view of an operating theatre. (A) Illustrates the traditional layout with opposite side operating and need for additional equipment. (B) Illustrates the layout with a solo operating surgeon and their trainer. Additional equipment is close to the surgeons, with a reduced need for extra equipment. The scrub nurse is positioned closer to the surgical field. [surgeon (s), trainer (t), scrub nurse (n), anaesthetist (a), light source (LS), nerve monitor (nm), diathermy machine (dm), anaesthetic machine (am)]
The previous dynamic of a primary surgeon and their assistant has now been shifted to that of a single operating surgeon - the trainee - and their trainer. This new arrangement allows the trainee to acquire their surgical skills at a more efficient rate, especially where many training programmes require a minimum number of key procedures as ‘primary surgeon’ before acquiring the Certificate of Completion of Training (CCT) [16]. The trainee’s confidence is also preserved as their trainer can be on hand to provide extra assistance if necessary, whilst they operate with greater independence. The trainer’s confidence in their trainee can also be improved in this respect, whilst improving their competence in providing training.
Impact on the theatre environment
It is widely accepted that the training of a surgeon in theatre must be balanced with the efficient flow of an operating list such that it finishes within the time allocated. This is, however, a multidisciplinary process requiring the concerted efforts of surgeons, anaesthetists, the scrub team and other theatre and ward staff [17,18]. Any delay in this process means that these teams become pressured - in order to make up time, training opportunities may be compromised.
We have found that the surgeries performed by the trainee using elasticated retractors are shorter in duration than those performed using traditional means. We feel that this will help in making the time for training more efficient and the culture of training to become universally acceptable in more time-pressured surgical lists.
Given the topographical rearrangement of the trainee and trainer in theatre, the opportunity is given for the scrub nurse to place themselves closer to the patient (see Figure 5). This makes their job easier as they have a better view of the operation and can easily anticipate requests for instruments from the surgeon. Additionally, same side operating also creates a workplace that is safer for circulating staff as there are fewer trailing cables: for example, only one headlight may need to be used in solo operating. The task of monitoring and passing sharp instruments is made easier for the scrub nurse as they are closer to the operative field.
References
1. Steele PRC, Curran JF, Mountain RE. Current and future practices in surgical retraction. The Surgeon 2013;11:330-7.
2. Beard J, Rowley D, Bussey M, Pitts D. Workplace-based assessment: assessing technical skill throughout the continuum of surgical training. ANZ J Surg 2009;79:148-53.
3. Intercollegiate Surgical Curriculum Programme. www.iscp.ac.uk Last accessed April 2017.
4. Anwar M, Irfan S, Daly N, Amen F. EWTD has negative impact on training for surgeons. BMJ 2005;331:1476.
5. Benes V. The European Working Time Directive and the effects on training of surgical specialists (doctors in training): a position paper of the surgical disciplines of the countries of the EU. Acta Neurochir (Wien) 2006;148:1227-33.
6. Cresswell B, Marron C, Hawkins W, et al. Optimising Working Hours to Provide Quality in Training and Patient Safety. A Position Statement by the Association of Surgeons in Training, London. January 2009.
7. Rogers SN, Davies ES. An alternative method of intraoperative skin retraction: the Walton fish hook. Br J Oral Maxillofac Surg 1995;33:323.
8. Arullendran P, Robson AK. The fish hook retractor. J Laryngol Otol 2001;115:212-3.
9. Ellul D, Sheikh S. Retraction technique in open-approach rhinoplasty. J Laryngol Otol 2011;125:1270-1.
10. Chan AC, Chung SC, Li AK. Liver retraction using elastic bands. Aust N Z J Surg 1990;60:217.
11. Skillman JJ, Kent KC. Elastic retraction for exposure of the femoral artery. Surg Gynecol Obstet 1990;170:71.
12. Carriero A, Dal Borgo P, Pucciani F. Stapled mucosal prolapsectomy for haemorrhoidal prolapse with lone star retractor system. Tech Coloproctol 2001;5:41-6.
13. Steele PRC, Mountain RE. Elasticated retractors in tracheostomy. J Laryngol Otol 2013;127:1141-2.
14. Mountain R, et al. Lone Star Retractor System – Head and Neck Procedure Guide. 2014 CooperSurgical, Inc. ver.82402 Rev. 03/2012.
15. McIlhenny C, Pitts D. Standards for Surgical Trainers. The Faculty of Surgical Trainers, The Royal College of Surgeons of Edinburgh. April 2014.
16. Guidelines for the award of a CCT in Otolaryngology. Last accessed April 2017.
17. Delaney CL, Davis N, Tamblyn P. Audit of the utilization of time in an orthopaedic trauma theatre. ANZ J Surg 2010;80:217-22.
18. Travis E, Woodhouse S, Tan R, et al. Operating theatre time, where does it all go? A prospective observational study. BMJ 2014;349:g7182.
Key Points
-
Elasticated retractors are able to provide effective retraction of tissues intra-operatively. They remain static for long periods time, but can be manipulated easily.
-
They allow for a shift in operative training, from the surgeon and trainee-assistant to the solo-operating trainee and supervising trainer.
-
They allow the trainee to progress quickly, efficiently and safely in acquiring operative skills.
-
Elasticated retraction can also promote better flow and safety in the theatre environment.
Declaration of competing interests: None declared.
Funding Statement: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.