Epiphora, or abnormal tearing, occurs because of blockage in the lacrimal drainage system, which impairs normal tear channeling into the nose. Dacryocystorhinostomy (DCR) is used to treat patients diagnosed with lacrimal sac or nasolacrimal duct obstruction (NLDO).
External DCR was the Gold standard treatment for NLDO for more than 100 years and had a high success rate of 90% and above. With the introduction of endoscopes and DCR burrs, the endonasal approach is being used more and more by ENT surgeons for management.
The endoscopic approach has several advantages, including the following:
- It provides a better aesthetic result with no external scar.
- It allows a one-stage procedure to also correct associated nasal pathology that may be causative.
- It avoids injury to the medial canthus and / or pathologic scar formation.
- It preserves the pumping mechanism of the orbicularis oculi muscle.
- Active infection of the lacrimal system is not a contraindication to surgery.
- It is especially superior to the external approach in revision surgery.
- It is much less bloody than the external approach.
- Because of the facility of the approach, the perioperative time is shorter.
The success rate is comparable to external approach but the outcome can be improved even further. The senior author has performed many endoscopic DCR surgeries with successful outcome and good long-term results. The article is written with a view to identifying and overcoming the pitfalls and improving the success rates.
Clinical diagnosis
The diagnosis of NLD outflow obstruction is made following documentation of symptoms, examination and appropriate investigation.
- History should include history of patient’s symptoms, ocular or nasal disease, trauma, ocular medication and history of systemic diseases.
- Ocular examination – to look for a cause of hypersecretion of tears, to examine lid apposition to globe, conjunctiva, puncta, cornea and tear film on the slit-lamp.
- Intranasal examination to exclude nasal pathology and identify anatomical variations.
- Fluorescein dye retention tests – test of obstructed tear flow. A drop of 2% fluorescein is instilled in the conjunctival sac. The amount of residual colour 3-5 minutes after the dye is instilled is noted. The test is positive if residual fluorescein is present. The intensity of colour is graded on a scale of 0-4. False negative finding may occur due to a large lacrimal sac, mucocele or a distant NLD obstruction.
- Diagnostic probing and syringing of the lacrimal system – it can detect both the presence and site of partial or complete lacrimal outflow obstruction.
- Jones 1 and 11 tests for functional epiphora – the Jones tests are dye tests for functional epiphora where it is known from syringing that the lacrimal drainage system is patent. In conjunction with the fluorescein dye retention test, probing and irrigation can help differentiate hypersecretion and epiphora.
- Dacryocystography – injection of contrast material into the duct system followed by X-Ray views or CT scanning to identify the site of obstruction.
- Dacryoscintigraphy
- Computed tomography or magnetic resonance imaging of the lacrimal system and sinuses.
Not all the investigations are required with each case. The cause may be apparent following the more simple tests. Dacryoscintigragphy is recommended for diagnosis of functional lacrimal drainage obstruction, CT / MRI are useful in secondary obstructions such as those associated with nasal polyposis, nasal tumours.
Surgical technique
The procedure is generally done under general anaesthesia although it can be done under local anaesthesia. A combined team approach with ophthalmologist is recommended.
Position:
Patient is placed in the supine position with 30 degree head elevation. Ipsilateral eye is kept open and the contralateral eye is lubricated with lacrilube ointment and taped. Corneal shields may also be used. General anaesthesia with TIVA-Remifentanyl and Sevoflurane is routinely used and blood pressure is kept optimal around 100 systolic blood pressure.
Nasal preparation:
5% cocaine solution is prepared and the nasal cavity sprayed using the atomiser jet insufflation 15 minutes prior to the procedure in the anaesthetic room. Once the patient is placed on the operating table, the middle turbinate and the lateral nasal wall just anterior to the middle turbinate is infiltrated with 2% lignocaine and 1:80,000 adrenaline. Middle meatus is packed with medium sized neurosurgical patties soaked in 1:1000 adrenaline.
Procedure
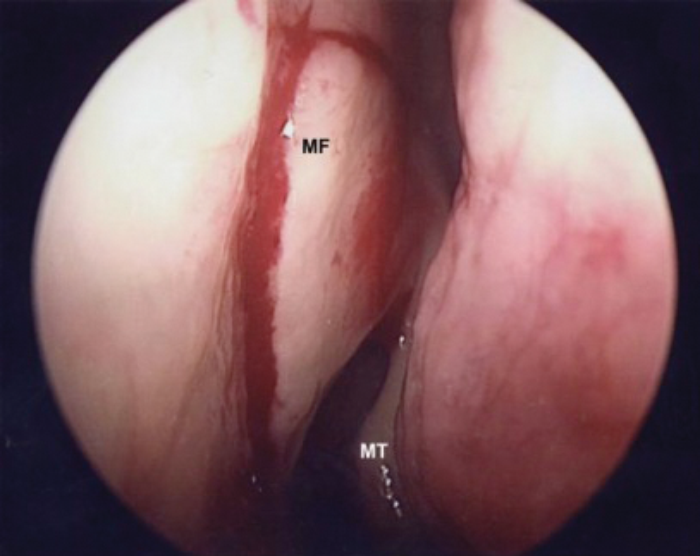
A vertical incision is made at the level of the anterior maxillary crest 8mm above, 8mm anterior and 10mm down to the level of the midportion of the middle turbinate (Figure 1). Horizontal incision is next placed extending from the vertical incision to the uncinate process. Mucoperiosteum is elevated using a suction Freer elevator / dissector and folded away from the lateral wall.
MT – Middle Turbinate MF – Mucosal Flap Marking
Figure 1. Mucosal incision in the lateral wall 8mm above, 8mm anterior to middle turbinate.
Bone removal
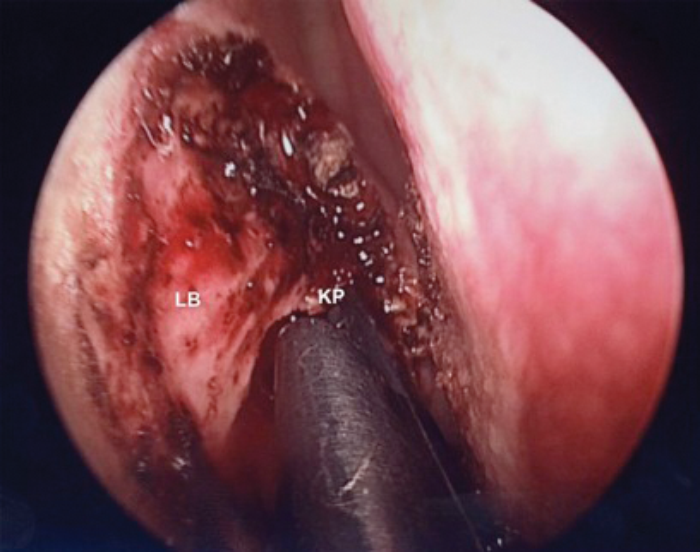
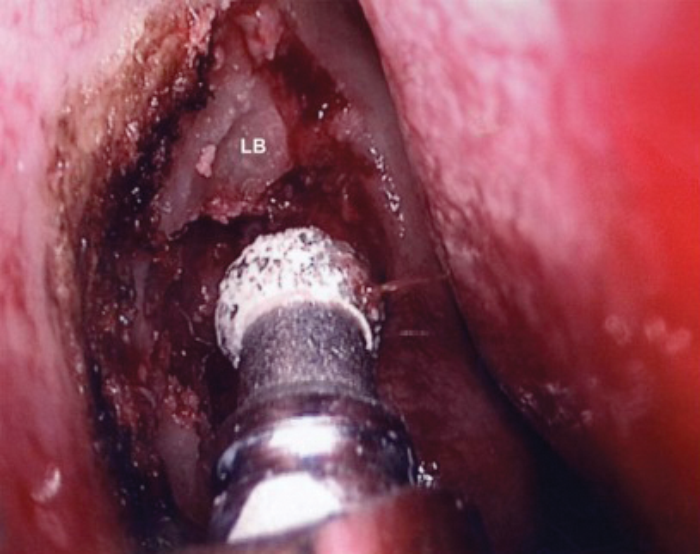
The nasolacrimal bone is divided into two parts, anterior hard bone forming the anterior lacrimal crest and posterior thin bone in front of the uncinate process. The thin posterior bone is removed using the 2mm Kerrison punch (Figures 2a & b) starting superiorly from the axilla of the middle turbinate down inferiorly to the level of middle portion of the middle turbinate. The tip of the punch should be used to push the sac away where the lacrimal bone needs to be removed. Care should be taken not to inadvertently grasp the sac while closing the punch. Thin lacrimal bone is then gently flaked away with the sharp end of the Freer elevator. Superiorly and anteriorly where the bone becomes thick, a 15 degree curved 2.9mm endonasal microdebrider DCR coarse diamond burr (Medtronic, Jacksonwill, Florida) (Figure 3) is used for removing the hard bone anteriorly over the maxillary crest and above the axilla. The sac including the fundus should be completely exposed for successful outcome.
LB – Lacrimal bone KP – Kerrison Punch
Figure 2a. Removal of Lacrimal bone with Kerrison punch.
Figure 2b. Kerrison Punch.
LB – Lacrimal bone
Figure 3. Removal of upper part of lacrimal bone with diamond drill.
Dacryocystorhinostomy
Once wide bone removal has been achieved, the sac should stand proud and exposed from just above the axilla of the middle turbinate down to the mid portion of the middle turbinate (Figure 4). The lacrimal puncta is dilated with a lacrimal punctum dilator (Figure 5) and the lower canaliculus cannulated with a 0 Bowman canalicular lacrimal probe. The sac is thus made to tent medially. A vertical incision is made along the lacrimal sac using a sickle knife (Figure 6). Lacrimal sac is opened like a book with an anterior and posterior flap. Horizontal incisions are then placed superiorly and inferiorly in the posterior flap and the midportion of the posterior flap removed with Bellucci scissors (Storz, Germany).
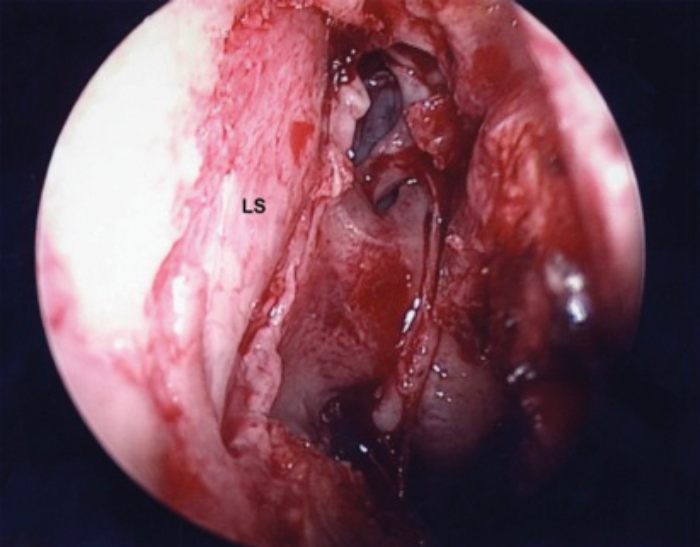
LS – Lacrimal sac
Figure 4. Complete exposure of lacrimal sac.
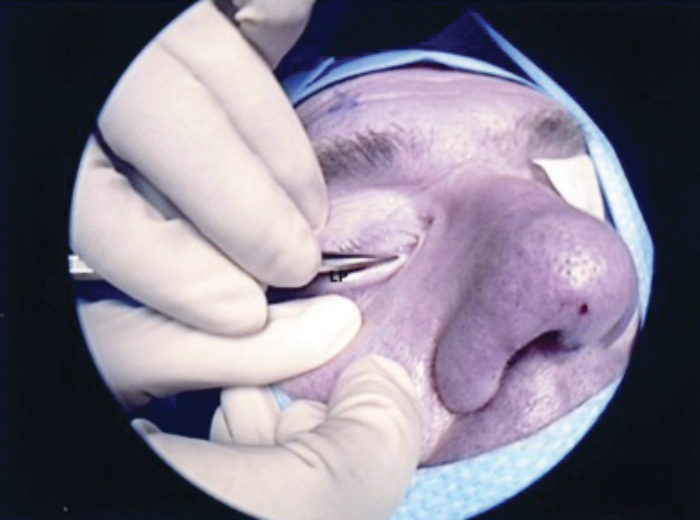
LP – Lacrimal probe
Figure 5. Probing of lower canaliculi with lacrimal punctum dilator.
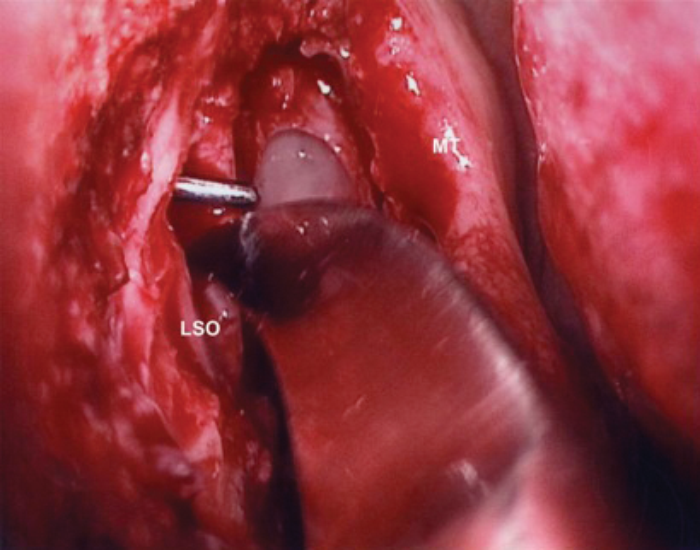
LSO – Lacrimal sac opening
Figure 6. Lacrimal sac opening with sickle knife.
A wide nasolacrimal window is created. Silastic lacrimal stents are then placed via both upper and lower canaliculi, retrieved endonasally (Figures 7a & b) and tightened over a 18 gauge venflon sheath / silastic tubing (Figure 8) to prevent upward migration of the stent knot. The stent loop is ensured not to be too tight as it may cheese wire through the puncta. We prefer using ligaclips to stabilise the stents (Figures 9a & b) in place of knots to avoid any risk of slippage of the knot leading to stent laxity. The nasal mucosa is trimmed and folded back to cover the exposed bone and haemostasis achieved with suction diathermy.
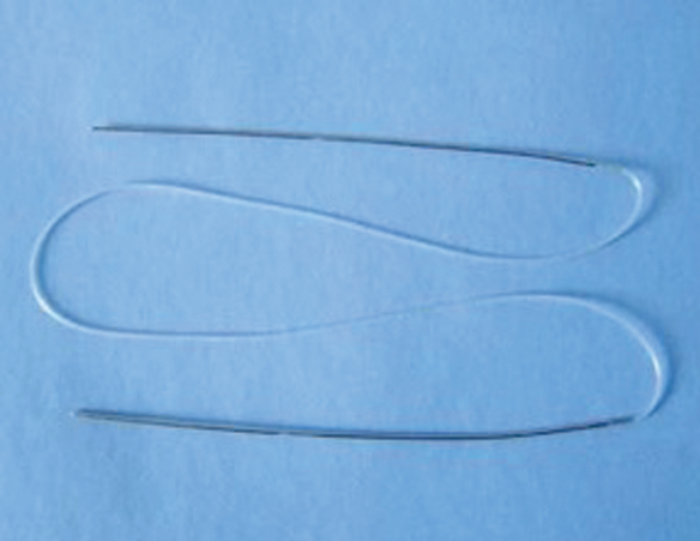
Figure 7a. Silicone bicanalicular tube with double metallic loader.
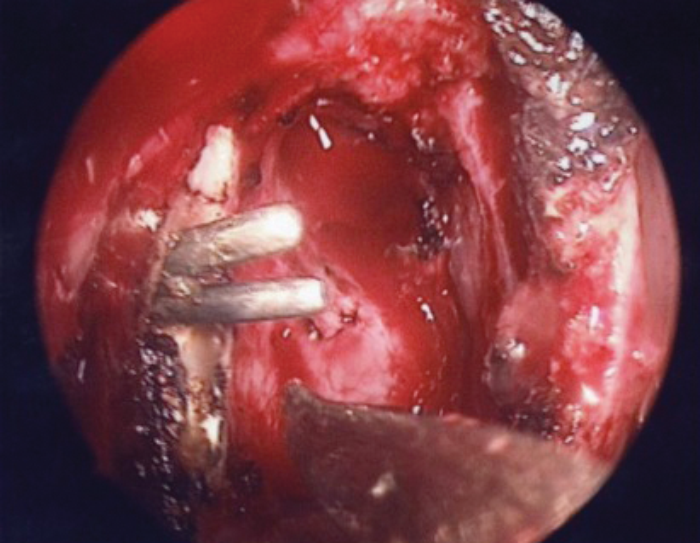
Figure 7b. Silastic stenting of both upper and lower canaliculi and
retrieval of the tips through the dacryocystostomy.
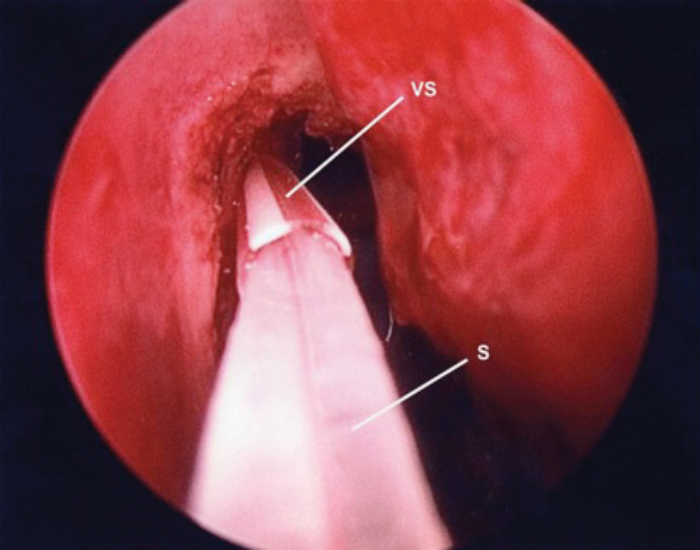
VS – Venflon Sheath S – Stent
Figure 8. Silastic stents guided through trimmed venflon sheath.
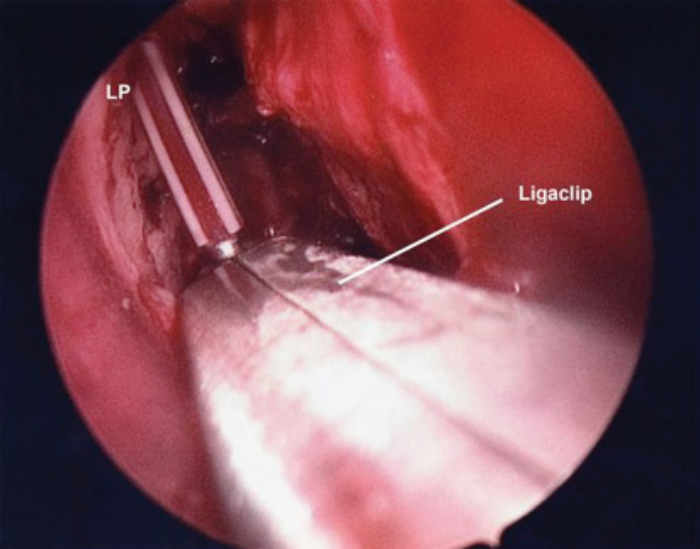
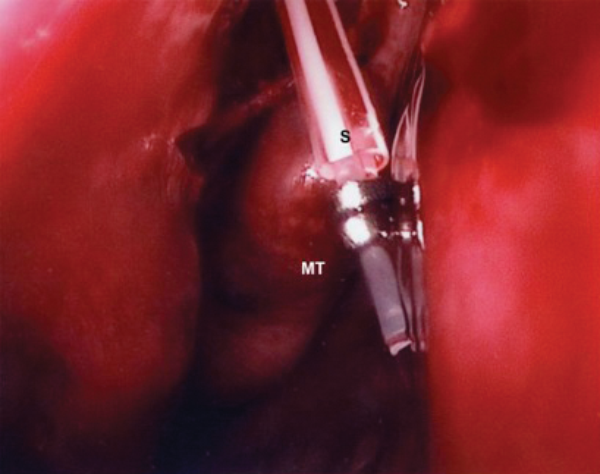
MT – Middle Turbinate S – Stents
Figure 9a (top) & 9b (above). Stent stabilisation with Ligaclips.
The eye is lubricated with chloramphenicol drops and nasal cavity packed loosely with small nasopore dressings soaked in topical steroid drops. Patient is advised not to blow their nose in the immediate post-operative period. Topical nasal saline douching and topical chloramphenicol eye drops are advised for two weeks.
Follow-up
Patients are seen at three weeks and at three months. Any granulation tissue seen around the stents is removed and the stents are kept in-situ for three months and removed in the outpatient clinic. Patency is checked with fluorescein dye test. Patients are discharged after one year.
Success rates
Success is defined as complete resolution of patient’s symptoms and patency of the nasolacrimal window. In our series success was achieved in 95% of cases using the above technique.
Conclusion
Endoscopic Dacryocystorhinostomy is a minimally invasive endoscopic technique that offers good long-term surgical outcome. The key to success includes exposure of the whole sac including the fundus, creation of wide nasolacrimal window, mucosal preservation and meticulous postoperative care.
Key points:
-
Adequate nasal preparation
-
Meticulous technique
-
Adequate lacrimal bone removal
-
Creation of wide nasolacrimal window
-
Removal of midportion of lacrimal sac posterior flap
-
Stent placement for three months.
References
1. Huang J, Malek J, Chin D, et al. Systematic Review and Meta-Analysis on Outcomes for Endoscopic Versus External Dacryocystorhinostomy. Orbit 2014;33(2):81-90.
2. Hartikainen J, Antila J, Varpula M, et al. Prospective randomized comparison of endonasal endoscopic dacryocystorhinostomy and external dacryocystorhinostomy. Laryngoscope 1998;108(12):1861-66.
3. Maini S, Agave N, Youngs R. Endoscopic endonasal laser versus endonasal surgical dacryocystorhinostomy for epiphora due to nasolacrimal duct obstruction: prospective, randomised, controlled trial. J Laryngol Otol 2007;121(12):1170–76.
Declaration of competing interests: None declared.