In this interesting article, our experienced colleagues describe their favoured technique for performing endoscopic DCR and share with us the key steps for a successful outcome.
Dacrocystorhinostomy (DCR) was historically performed by ophthalmologists for nasolacrimal obstruction using external techniques. The modern endoscopic approach was introduced by McDounagh and Meiring in 1989 [1]. Tsirbas and Wormald in 2003 [2] described mechanical endonasal DCR, a technique that involves the creation of a large rhinostomy and mucosal flaps.
Their adaption involves the preservation, rather than sacrifice, of nasal mucosa and the fashioning of anterior and posterior flaps of the lacrimal sac to achieve marsupialisation. To achieve this, full exposure of the sac is required and, as the upper half of the lacrimal sac lies above the insertion of the middle turbinate, removal of the hard bone of the lacrimal crest of the maxilla in this area is necessary.
We describe our endoscopic posterior flap technique similar to that popularised by Tsirbas and Wormald and used by the senior authors (PW and GS) in this institution since 1995.
Preoperatively
Primary assessment is made by our ophthalmology colleagues, and indications for surgery include primary acquired canalicular obstruction, primary acquired nasolacrimal duct obstruction with secondary chronic dacrocystitis, acute dacrocystitis, functional block and revision surgery. Management options, including medical treatments, are discussed with the patient and surgical management is often adopted if obstructive symptoms are significant to the patient. Risks and complications are discussed, including failure of procedure and silastic tube problems.
“Bone removal is continued superiorly up to the level of the axilla of the middle turbinate, where the bone invariably becomes too thick to punch.”
Intraoperatively
The procedure is usually performed under general anaesthetic. The steps involved include:
- Pre-injection of the agger mucosa, middle turbinate and uncinate. (Note- this may also include a trans caruncle block if the procedure is under local anaesthetic.)
- Raising mucosal flap
- Exposing the lacrimal sac
- Lacrimal sac intubation
- Sac incision and sac flap creation
- Stenting/marsupilisation
Tissue preparation
The nasal mucosa is decongested with 0.1% xylometazoline nasal spray, pledgets soaked in 1:1,000 adrenaline and the lateral nasal wall, middle turbinate and uncinate are injected with lidocaine hydrochloride 2% with adrenaline 1:80,000. Limited septoplasty can be performed for access endonasally, if required. A combination of 0° and 30° rigid endoscopes attached to an endocamera system are used for imaging the procedure.
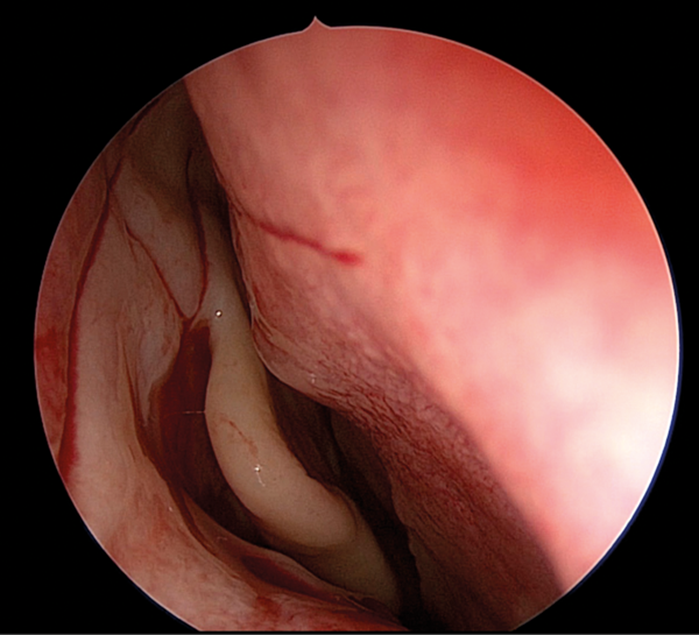
Figure 1. ‘H’ shaped incision of agger mucosa.
Raising mucosal flap
A mucosal flap is fashioned with a crescent knife, by creating an ‘H’ shaped incision in the agger mucosa (see Figure 1). The incision starts 8mm above the insertion of the middle turbinate and brought down vertically to the level of the insertion of inferior turbinate; this constitutes the first limb of the ‘H’. The second vertical limb is approximately 8mm anterior of this; the ‘cross bar’ of the H is made horizontally between the two vertical limbs just above the halfway point. This ensures a larger inferior flap, which allows for a better mucosal preservation. The two flaps (superior and inferior) are elevated with a Cottle elevator, exposing the junction of the hard frontal process of the maxilla and the thin lacrimal bone, i.e. the lacrimal crest of the maxilla.
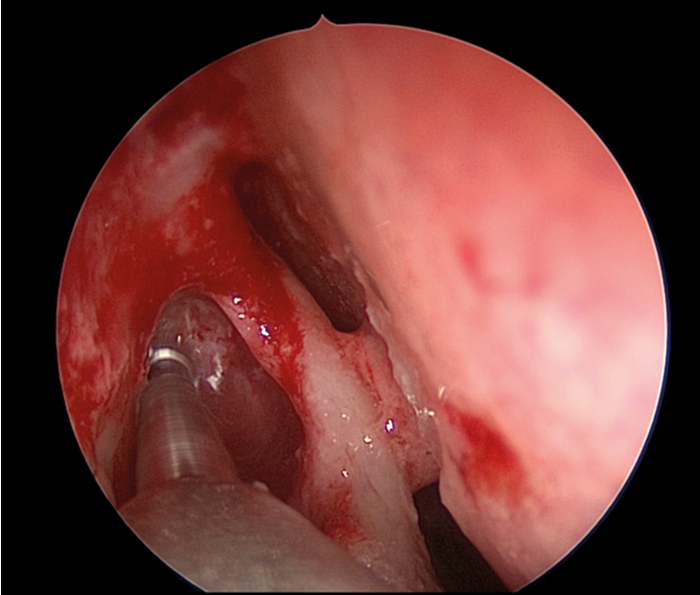
Figure 2. 3mm high-speed endonasal drill removing frontal process above axilla.
Exposing the lacrimal sac
A frontal sinus probe is used to develop a plane between the lacrimal sac and the lateral aspect of the lacrimal crest of the maxilla. The inferior aspect of frontal process of the maxilla is removed with Hajek-Koeffler retrograde and straight biting punches, and additional bone can be removed with a Kerrison Rongeur. Bone removal is continued superiorly up to the level of the axilla of the middle turbinate, where the bone invariably becomes too thick to punch. At this point, a 3mm high-speed endonasal drill is used to remove the remaining frontal process of the maxilla up to a level of 8mm above the axilla of the middle turbinate (see Figure 2). This will frequently give rise to exposure of any agger cells when present, and should ensure complete exposure of the sac up to the level of the fundus.
Lacrimal sac intubation
When lacrimal sac exposure seems adequate, an O’Donaghue probe and stent is passed down the inferior canaliculi to tent the medial wall of the sac. This will allow assessment to determine whether sufficient bone over the common canalicular opening has been removed. This is important as sufficient bone needs to be removed to allow the sac flaps to sit flat against the lateral nasal wall.
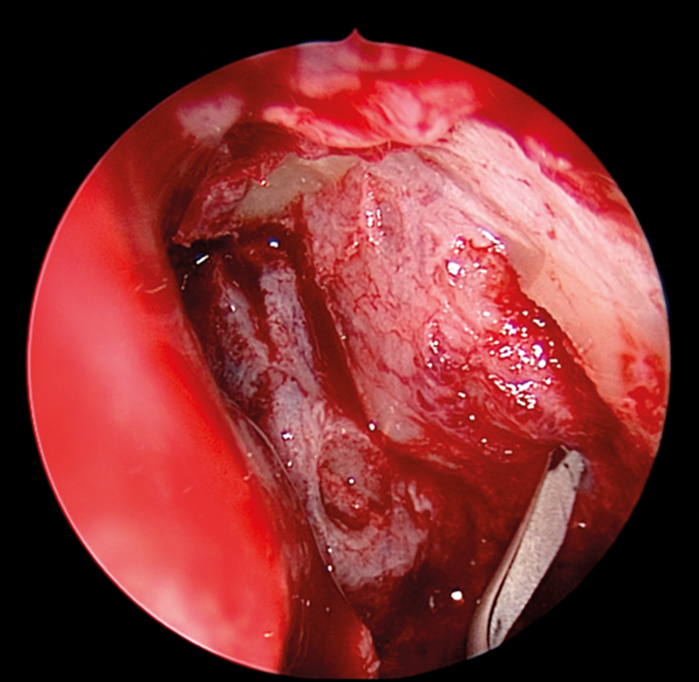
Figure 3. Initiating anterior lacrimal sac incison.
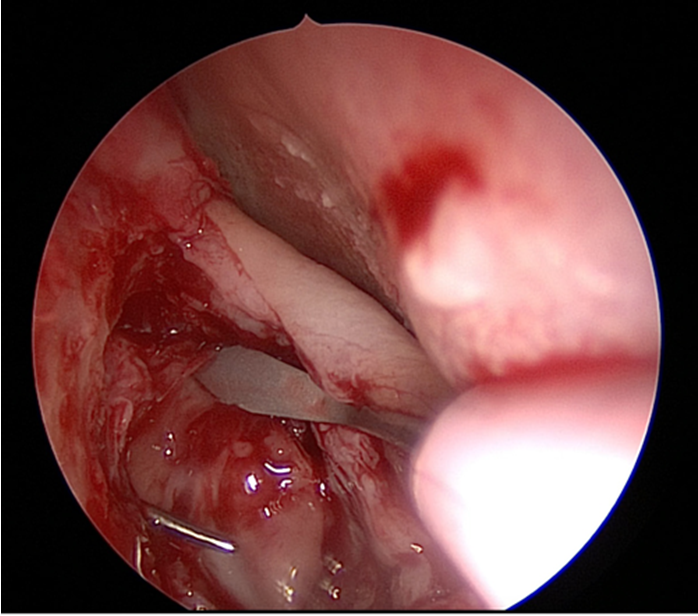
Figure 4. Superior release of lacrimal sac.
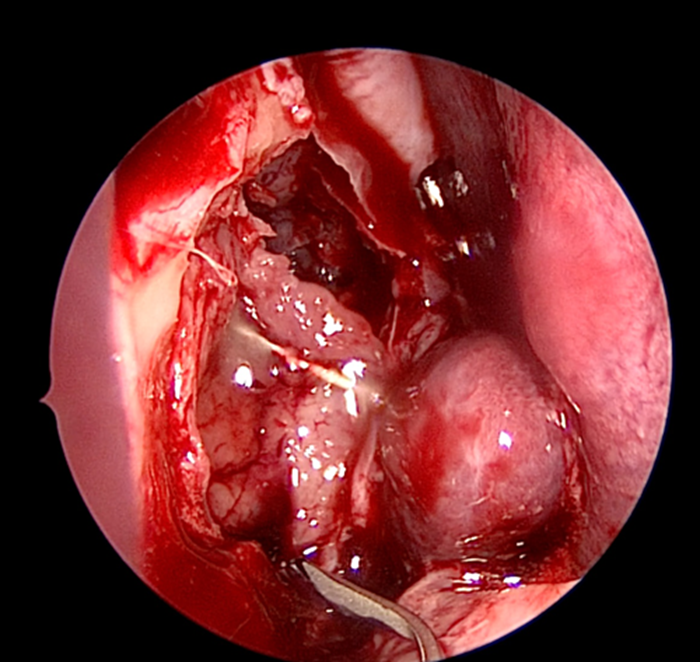
Figure 5. Inferior release of lacrimal sac.
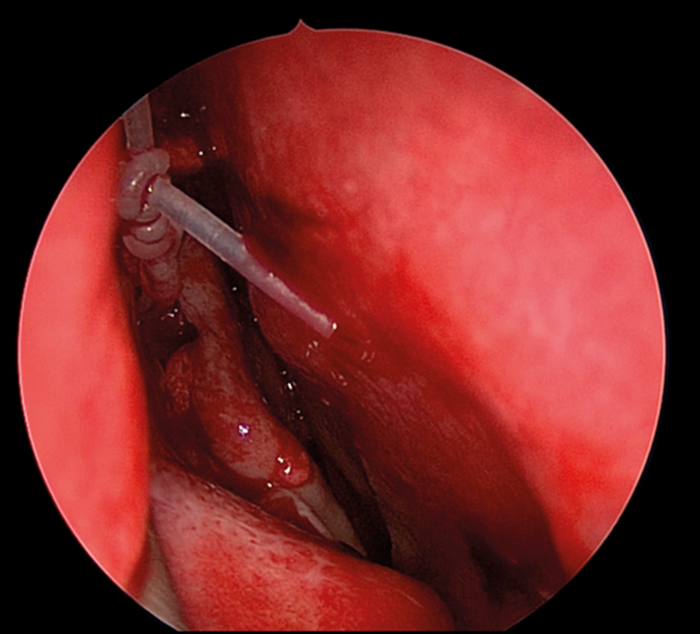
Figure 6. O’Donaghue tube in place with mucosal flaps laid back.
Stenting/marsupialisation and creation of the sac wall flap
The medial wall of the sac is tented medially using the end of the O’Donaghue probe and incised vertically using a sharp pointed Phaco knife at its most anterior aspect (see Figure 3). The aim is to create a large posterior based sac flap, which can later be folded back towards the uncinate process, facilitating full sac marsupialisation. Relieving incisions are then placed horizontally, both superiorly (see Figure 4) and inferiorly (see Figure 5) to complete the sac incision into a ‘C’ shape. The remaining posterior edge is left intact but the completed sac wall flap can now be folded posteriorly, exposing the entire sac lumen. The lacrimal probe should be visible and is pulled through with Mosquito artery forceps. The process is repeated with the probe and stent through the superior canaliculus. Upon delivery of the stents a Watzke sleeve is placed and the stents are tied. The lacrimal sac flaps remain folded backwards but the nasal mucosal flaps are repositioned to overlap each sac flap to encourage healing and ensure there is no exposed bone (see Figure 6).
Postoperatively and expected outcome
Patients are advised to use nasal irrigation twice daily with saline for six weeks. Most procedures are performed as day-cases. Patients are routinely reviewed at four-to-six weeks in a nurse-led clinic by a nurse practitioner trained in endoscopic stent removal and fluorescence appearance testing. Most cases would have stent removal at this stage. Audit of patient satisfaction following surgery has consistently been reflected by high Glasgow Benefit Inventory Scores (average 32.7) and patency rates of 90-95% for distal obstruction [3].
“Audit of patient satisfaction following surgery has consistently been reflected by high Glasgow Benefit Inventory Scores.”
Discussion
Systematic review and meta-analysis in 2010 [4] and 2014 [5] on outcomes of endoscopic versus external DCR found comparable results between the two groups with success rates of 65 to 100%, and noted that endoscopic technique avoids the risk of cosmetically unacceptable scars. In addition, they found that revision rates were comparable between the two groups. The technique we describe is based on total sac exposure and preservation of mucosa through a larger rhinostomy to try and prevent reclosure of the nasolacrimal stoma. We have found this technique to reliably produce good results with very few complications. Green et al [6] performed a systematic review of mucosal and lacrimal flaps in DCR and found level 1B evidence (two randomised controlled trials) showing a trend towards improved outcomes and reduced granulation tissue in groups with preserved mucosa. Complications attributed to the larger rhinostomy include skin/dermal exposure but, in the limited instances this has occurred, healing has been good with no lasting consequences. There is additional equipment and theatre time required to allow for the further anatomical resection.
References
1. McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol 1989;103:585-7.
2. Tsirbas A, Wormald PJ. Mechanical endonasal dacryocystorhinostomy with mucosal flaps. British Journal of Ophthalmology 2003;87:43-7.
3. Spielmann PM, Hathorn I, Ahsan F, et al. The impact of endonasal DCR on patient health status as assessed by the GBI. Rhinology 2009;47:48-50.
4. Leong SC, MacEwen CJ, White PS. A systemic review of outcomes after dacryocystorhinostomy in adults. Am J Rhinol Allergy 2010;24:81-90.
5. Huang J, Malek J, Chin D et al. Systematic review and meta-analysis on outcomes for endoscopic versus external dacryocystorhinostomy. Orbit 2014;33:81-90.
6. Green R, Gohil R, Ross P. Mucosal and lacrimal flaps for endonasal dacryocystorhinostomy: a systematic review. Clin Otolaryngol 2017;42:514-20.






