In this article Vikranth Visvanathan describes an exciting development on the use of endoscopic technology in complex otological practice.
Transcanal endoscopic ear surgery (TEES) is rapidly evolving as a recognised method of addressing middle ear and mastoid pathology. Since its introduction over two decades ago, otolaryngologists have employed this technique as an adjunct to conventional microscopic ear surgery or exclusive TEES. At this point in time surgeons are pushing the boundaries of TEES to manage disorders of the inner ear and lateral skull base as well. The evolution of TEES has also been made possible by advances in technology and surgical instrumentation.
In this article we describe our technique of surgical excision of middle ear cholesteatoma using the endoscope. The article, in particular, describes primary acquired attic cholesteatoma with limited mastoid extension. The extent of disease that can be managed exclusively with the transcanal approach is debatable but as a general rule, any pathology extending beyond an imaginary line drawn along the axis of the lateral semicircular canal may not be suitable for an exclusive endoscopic approach.
“Any pathology extending beyond an imaginary line drawn along the axis of the lateral semicircular canal may not be suitable for an exclusive endoscopic approach”
Theatre set-up
The patient is in the operating room under general anaesthetic, head turned to the contralateral side of the operating ear. The endoscope used is a 0 degree Hopkins rod telescope (Storz), 3mm diameter and 14cms in length. The endoscope is connected to a 3-chip video camera system with the monitor stationed opposite the operating surgeon. The scrub team position their table at the head end of the patient with the scrub nurse standing adjacent to the surgeon, therefore having a clear view of the monitor stationed across. The anaesthetic team is at the bottom end of the table with the circuit away from the operating field. Facial nerve monitor is used as a standard.
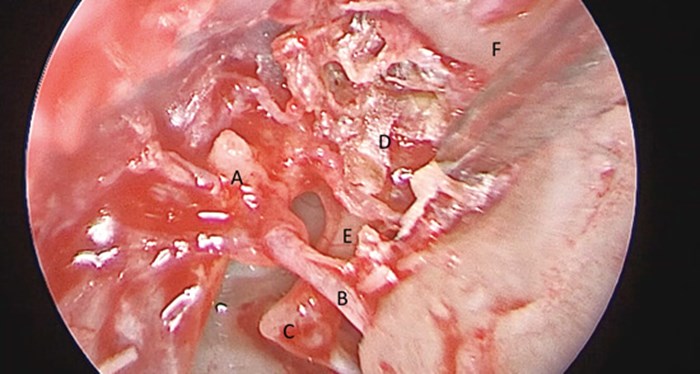
Figure 1. Left ear transcanal endoscopic view. A) Lateral process of malleus; B) Chorda Tympani; C) Incudostapedial joint; D) Cholesteatoma sac; E) Long process of Incus; F) Outer attic wall.
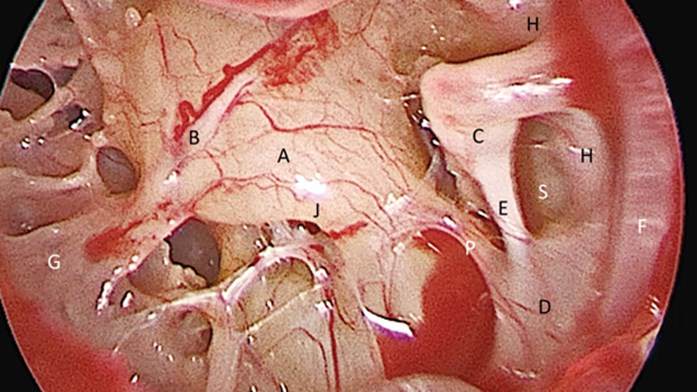
Figure 2. Left ear endoscopic middle ear view. A) Promontory; B) Jacobsons’s nerve; C) Incudostapedial joint; D) Pyramid; E) Stapedius tendon; F) Chorda tympani; G) Hypotympanic air cells; H) Facial nerve (tympanic segment); S) Sinus tympani; P) Ponitculus; J) Superior lip of round window niche.
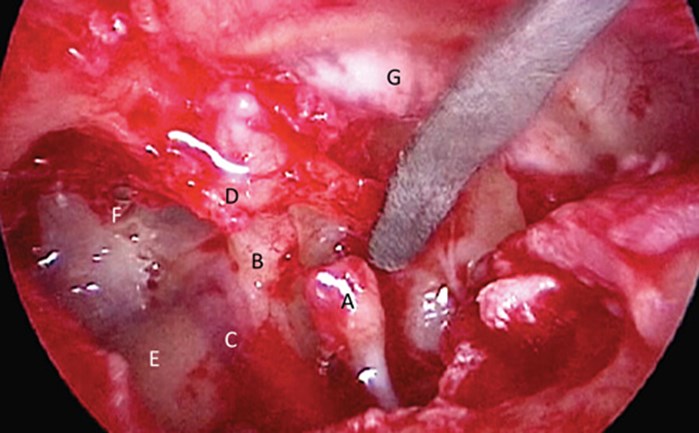
Figure 3. Right ear endoscopic view after removal of incus and head of malleus. A) Head of stapes; B) Cochleariform process; C) Tympanic facial nerve; D) Lateral process of malleus; E) Lateral semicircular canal; G) Tympanic membrane; F) Anterior epitympanic space.
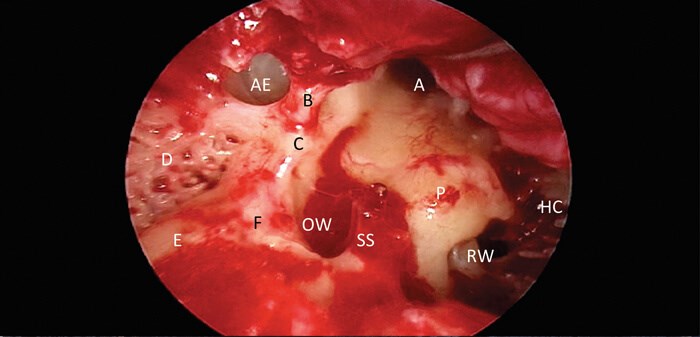
Figure 4. Right ear endoscopic view. A) Eustachian tube orifice; B) Tensor tympani tendon; C) Cochlearform process; D) Posterior epitympanic air cells; E) Lateral semicircular canal; F) Facial nerve; SS) stapes suprastructure; OW) Oval window; RW) round window; HC) Hypotympanic air cells; AE) Anterior epitympanic space.
Step 1
An examination under anaesthetic is performed under the microscope and the ear canal is slowly infiltrated with 2% lignocaine with 1:80000 adrenaline. The tragus is infiltrated (for cartilage harvest). Depending on the size of the tympanic membrane (TM) defect to be reconstructed the authors prefer infiltrating a small region (2cms) postaurally for temporalis fascia harvest. The ear canal is then packed with cottonoids soaked in adrenaline (1:10000) to aid haemostatic dissection.
Step 2
Following sterile preparation and draping, we begin by harvesting tragal cartilage with perichondrium and temporalis fascia (if required) at the start of the procedure. These wounds are closed primarily with absorbable sutures. Our reasons for performing this at the start are to allow the local anaesthetic with adrenaline to have maximum effect in the ear canal and also harvesting fascia early allows it to dry and ready for later use.
The endoscope is now used for the procedure. Surgery begins by raising a tympanomeatal flap. Standard ear canal incisions at six o’clock and 12 o’clock will suit most cases but this may need to be altered depending on the site of pathology and extent of TM that needs reconstructing. A tympanomeatal flap is raised with the aid of adrenaline soaked cottonoids to maintain an avascular plane until the annulus is identified and middle ear entered. The middle ear and attic are inspected to evaluate the pattern of disease and ossicular chain involvement.
Step 3
Initial dissection commences by curetting the outer attic wall and following the cholesteatoma sac to its lateral extent akin to a front to back mastoidectomy (atticoantrostomy). We prefer the use of curettes for this step, although fine diamond burrs (2 or 3mm) can also be used. The challenge with using high-powered drills is that the vibrations are transmitted to the endoscope, which affects image clarity. Use of drills also means there needs to be an assistant to provide irrigation/suction (three-handed technique) to clear bone dust and provide a clear view.
Once the back of the sac is identified, all disease is cleared. Similar to traditional mastoid approaches, if the disease is lateral to the ossicular chain, the ossicles can be preserved and disease cleared. Disease extending medial to the ossicular chain would require disarticulation of the incudo-stapedial joint and possible removal of the head of the malleus to achieve a clear view of the anterior epitympanic space and aid complete disease clearance. Complete removal of disease is possible with the use of angled instruments that are standard in all endoscopic ear surgery trays (Spiggle & Theis or Karl Storz).
Step 4
Once complete excision is achieved with the 0 degree endoscope, we recommend inspection of all middle ear recesses (sinus tympani, facial recess, supratubal recess) with a 30 degree endoscope for the presence of residual disease. These are addressed before planning reconstruction.
The final stage comprises of three elements:
- Reconstruction of the attic/mastoid defect
- Ossicular chain reconstruction
- Tympanic membrane repair
Reconstructing the attic defect is usually done with tragal cartilage with perichondrium as an island graft type fashion. Depending on the defect size, more than one piece of cartilage may be used. The ossicular chain reconstruction depends on the surgeon’s preference. Autologous incus is a reliable method to use with an intact stapes. Alternatively, partial or total ossicular replacement prosthesis may be used in the presence or absence of stapes suprastructure respectively. In the case of prosthesis a separate sheet of cartilage over the implant is required to minimise extrusion.
If temporalis fascia has been harvested, this can be used as a second layer of reconstruction and the TM flap replaced. Alternatively, for tympanic membrane reconstruction, biomaterial-based grafts (Biodesign®) can be used to good effect. The ear canal is packed with absorbable material (Gelfoam®) soaked in antibiotic solution and cotton wool placed in the ear canal. No other dressings are required. All procedures are performed as day surgery.
SUMMARY
-
Transcanal endoscopic ear surgery is a feasible and safe method of addressing middle ear cholesteatoma.
-
It is minimally invasive, provides excellent visualisation of the middle ear and its complex recesses and can be performed as day surgery in most centres.
-
The use of angled endoscopes and instruments provide the added advantage of examining hidden recesses such as the sinus tympani, facial recess and anterior epitympanic space.
Declaration of Competing Interests: None declared.





