
Traditionally middle ear surgery, including stapes surgery, has been performed using the operating microscope. In this article the authors describe their experience with endoscopic middle surgery and share some of its advantages.
Trans-canal endoscopic ear surgery (TEES) is now a very well-recognised technique for the management of middle ear and mastoid pathology. Early published literature on TEES was focused on its applications in chronic otitis media. Key advantages of TEES are its minimal invasiveness and excellent visualisation of difficult-to-access areas within the middle ear (facial recess and sinus tympani). The disadvantages are that of being a one-handed technique and lack of stereoscopic vision.
Once the early hurdles were crossed in TEES, the natural evolution was to capitalise on its advantages for other finer otological procedures, such as stapes surgery. It has been two decades since the endoscopic approach was first described for stapedectomy and recent case series have highlighted its advantages over the traditional microscopic technique. The main advantage of the endoscope in stapes surgery over the microscope is the better preservation rates of the chorda tympani nerve (CTN). Since the endoscope offers a panoramic view of the middle ear, there is less curetting of the outer attic wall, hence minimising iatrogenic injury to the CTN. The audiometric outcomes between the endoscopic and microscopic surgery are comparable, with no clear advantage with the endoscopic technique.
“The main advantage of the endoscope in stapes surgery over the microscope is the better preservation rates of the chorda tympani nerve”
In this article, we describe our technique of endoscopic stapes surgery. The steps of stapedotomy with the endoscope are practically similar to the microscopic technique. It is highly recommended that otologists keen to adapt the endoscope in stapedotomy acquire adequate experience in all aspects of TEES for middle ear disorders before embarking on stapes surgery.
Step 1 - Ear canal preparation
With the patient in a supine position and head turned towards the contralateral side, examination under anaesthetic is performed using the endoscope or microscope, and the ear canal is slowly infiltrated using lignocaine with 1:80000 adrenaline. Slow infiltration is key to minimise blistering of the ear canal skin. After infiltration, the ear canal is packed with cottonoids soaked in 1:1000 adrenaline to reduce bleeding. Some surgeons pack the ear with a pope wick soaked in adrenaline even before the patient is anaesthetised as a preoperative preparation.
Step 2 - Tympano-meatal flap elevation
Following sterile preparation and draping, the endoscope (0 degree) is used to examine the ear and trim ear canal hair. The procedure starts with ear canal incisions at six and 12 o'clock. These two incisions are joined and a tympanomeatal (TM) flap is raised. Once the annulus is identified, the middle ear is entered, making sure that the chorda tympani is preserved.
Step 3 Exposure
Once the middle ear is entered, the landmarks that have to be clearly visualised are the facial nerve, pyramid, stapedius tendon, incudostapedial joint and stapes footplate. As mentioned before, conventional microscopic surgery almost always requires curetting the outer attic wall to visualise the above structures. However, with the endoscope, this may not be needed due to the wide-angle view. Nevertheless, if access is limited, the bony overhang of the scutum must be curetted.
Step 4 - Confirmation of diagnosis and delivery of stapes
Following successful identification of the above structures, the incudostapedial joint is disarticulated and the mobility of the incudomalleolar joint is assessed first (to rule out malleus head fixation) followed by stapes mobility.
Once the diagnosis is confirmed, the stapedius is divided, posterior crurotomy is performed and stapes suprastructure removed by down fracturing the stapes. These steps can be performed with cold steel instrumentation or with fibre laser assistance. If using a laser, care should be taken to use appropriate settings and also to use either a filter for the endoscope or to switch off the aiming beam to reduce the image being distorted.
“Some surgeons pack the ear with a pope wick soaked in adrenaline even before the patient is anaesthetised as a preoperative preparation”
The laser settings used in our practice are (532nm fibre laser) 2W 200ms pulse for crurotomy, 1W, 200ms pulse for stapedotomy and 1W, 100ms pulse for crimping the prosthesis. Using a stapes measuring rod, the piston length is determined from the footplate to the medial surface of the long process of the incus and 0.25 -0.5mm added to this distance.
Step 5 - Fenestration and piston placement
Footplate fenestration can be performed either with a series of micro perforators or a skeeter diamond drill (with/without laser assistance). If the laser is used, this is done by creating a rosette pattern first (to weaken the footplate) followed by fenestration with a 0.7/0.8 mm diamond drill. A right-angle hook may also be used to ensure that the fenestration is adequate.
“It is highly recommended that otologists keen to adapt the endoscope in stapedotomy acquire adequate experience in all aspects of TEES for middle ear disorders before embarking on stapes surgery”
Utmost care is taken to avoid any direct suction over the footplate area. An appropriately sized Nitinol or Teflon piston is placed in the oval window and crimped onto the long process of the incus. The ossicular chain mobility is checked and the TM flap replaced. Absorbable packing material or ointment is placed in the ear canal.
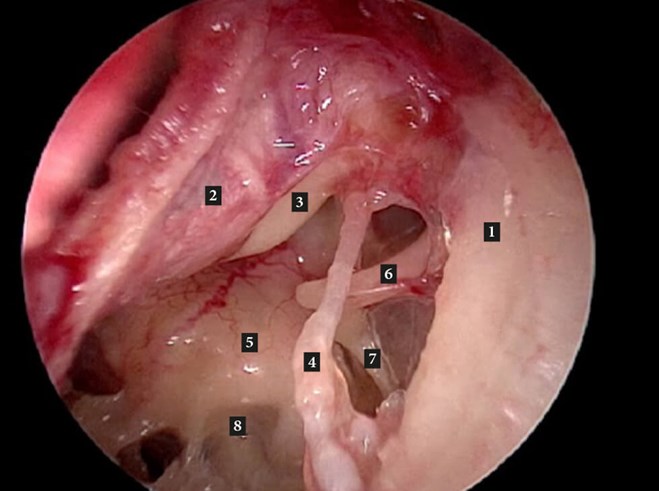
Figure A: Left middle ear. 1. Outer attic wall; 2. Tympanomeatal flap (reflected forwards); 3. Handle of malleus;
4. Chorda tympani; 5. Promontory; 6. Long process of incus; 7. Stapedius tendon.
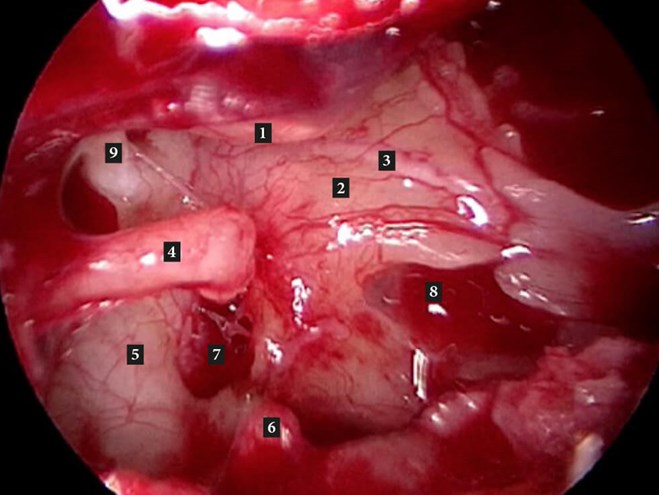
Figure B. Right middle ear (after removal of stapes suprastructure). 1. Handle of malleus; 2. Promontory;
3. Jacobsons nerve; 4. Long process of incus; 5. Tympanic segment of facial nerve; 6. Pyramid;
7. Oval window; 8. Round window niche; 9. Cochleariform process with tensor tympani tendon.
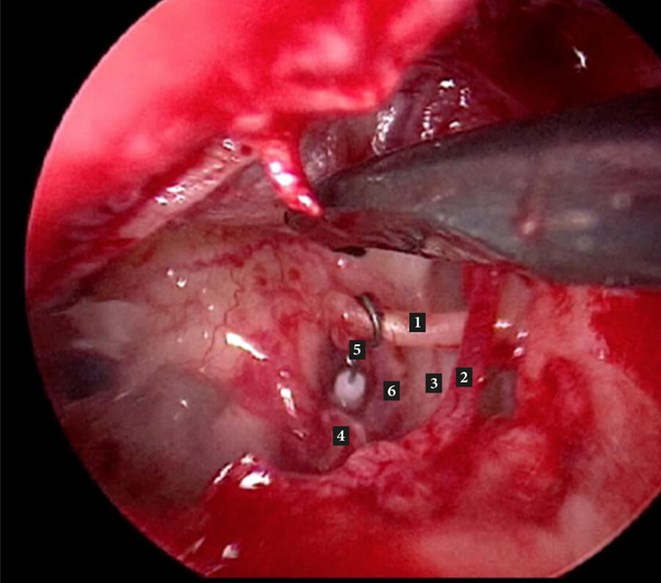
Figure C. Left middle ear with stapes piston in place. 1. Long process of incus; 2. Chorda tympani;
3. Tympanic segment facial nerve; 4. Pyramid 5. SMART Gyrus (self-crimping) stapes piston; 6. Oval window.
Summary
- Endoscopic stapes surgery is a safe and feasible technique for surgical management of hearing loss due to otosclerosis.
- Its key advantages are superior visualisation of the middle ear anatomy, limited need to curette the outer attic wall and better preservation rates of the chorda tympani compared with the microscopic technique.
- Surgeons keen to perform endoscopic stapedotomy should gain adequate experience in all forms of endoscopic middle ear surgery (tympanoplasty, ossiculoplasty, middle ear cholesteatoma excision) before embarking on stapes surgery.
Further reading
1. Sproat R, Yiannakis C, Iyer A. Endoscopic stapes surgery: A comparison with microscopic surgery. Otol Neurotol 2017;38(5):662-6
2. Bhardwaj A, Anant A, Bharadwaj N, et al. Stapedotomy using a 4 mm endoscope: any advantage over a microscope? J Laryngol Otol 2018;132(9):807-11.





