Benign strictures of the upper oesophagus and pharynx, while not very common, can be a challenging condition to successfully manage. The authors of this article provide us with a detailed description of their technique for using the CO2 laser, balloon dilatation and TISSEEL glue to provide a safe and effective way of managing this clinical scenario.
As ENT surgeons, we all encounter cases of dysphagia, of multiple aetiology. One of these causes is benign oesophageal stricture. Once diagnosed, the treatment modalities vary according to the location of the stricture, surgeon experience, availability of equipment and local guidelines.
Our preferred modality is the use of CO2 laser combined with balloon dilatation. In our experience, this releases the tissue tension associated with scar tissue, reduces the risk for inadvertent and uncontrolled mucosal tearing during dilatation, and allows space for atraumatic serial dilatation, achieving symptom improvement with safety and a lower recurrence rate for re-scarring.
Background
We present the case of a 63-year-old woman presenting with ongoing swallowing difficulties to solids, three months post neck radiation. She had chemoradiotherapy for squamous cell carcinoma (SCC) of an unknown primary that presented with metastases to a right level II neck node. Her diet was restricted to pureed food and nutritional supplements orally, supported additionally with gastrostomy feeding tube. She had a history of hiatus hernia and reflux for more than 25 years. We followed her for 14 months post completion of radiotherapy with trials of conservative management for her symptoms, but her dysphagia to solids remained unrelieved.
“If the main point of pressure shifts away from the site of the stricture, the balloon is deflated completely, repositioned and the process started again”
Investigations
A video fluoroscopy swallow test was done initially post treatment revealing normal swallow phases. A barium swallow test showed a high cervical oesophageal scar (luminal web), as well as the previously known sliding hiatus hernia. This explained the patient’s current dysphagia symptoms and supported our plan for surgery.
Procedure
This was performed under general anaesthesia with standard draping and non-sterile but clean technique. A laser endotracheal tube (ETT) was used to minimise the risk of airway fires.
An appropriately sized rigid pharyngoscope is chosen, lubricated with gel and inserted via the oral cavity in a lateral approach. Care is taken to avoid any dental damage. The pharyngoscope is advanced past the arytenoids to visualise the post-cricoid region and oesophageal inlet; the web/stricture is examined and managed through a minimally invasive technique. Pharyngeal suspension is set up with the aid of a Mayo table as per direct laryngoscopy, and findings recorded using a zero-degree Hopkins rod endoscope. A small piece of sterile measuring tape can be inserted to measure the thickness of the web and the remaining lumen diameter for food to pass through.
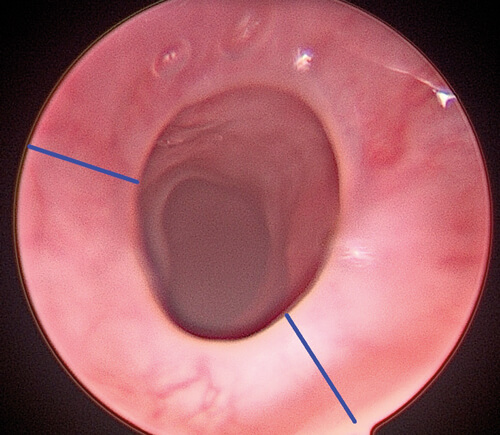
Figure 1. Oesophageal web with markings demonstrating the areas targeted by the CO2 laser.
The microscope with CO2 laser mount is set up, and a laser safety checklist implemented. Using a suction probe, two to three points of maximum web thickness and length are identified (approximately equidistant at two, six and 10 o’clock when concentric scar; in this case at 10 o’clock and five o’clock positions as scarring was slightly eccentric). As demonstrated by the marks on Figure 1, we set the laser to a 1-2mm linear configuration, super-pulse mode, at 10 watts and repeat setting initially, then switched to continuous mode setting once the surgeon’s hands were accustomed (Figure 2).
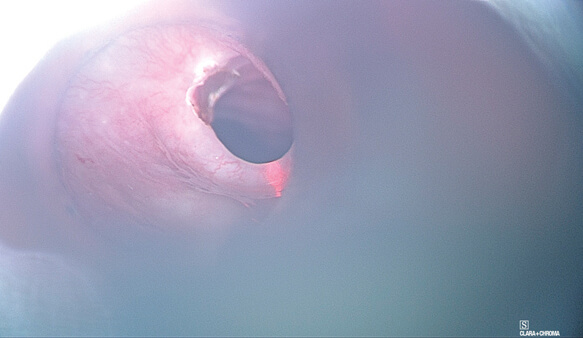
Figure 2. CO2 lasering of areas previously marked.
These settings allow precise transection of the web/ring of scar, while avoiding damage to normal oesophageal tissue, minimising thermal injury and resultant inflammatory response from which repeat scars form. A suction probe is placed on the web to provide counter-traction, as in any form of dissection, until the web is sufficiently released. It also has the added advantage of removing smoke out of the surgical field, clearing the surgeon’s view. The laser is then set to stand-by mode for safety and the balloon dilatation kit is prepared. Depending on the initial stricture diameter (prior to laser), appropriately sized balloons should be used sequentially. In this case, we used a single size 11 balloon and incrementally dilated from 11 to 12 and then 13mm diameter. The scrub nurse or assistant ensures the syringe and catheter are devoid of air in order to ensure the correct measurement of balloon pressure. Once the system is primed and balloon deflated, the surgeon passes the catheter gently through the stricture point until the waist of the balloon is positioned at the central point of the stricture; the balloon is then inflated gradually (Figure 3).
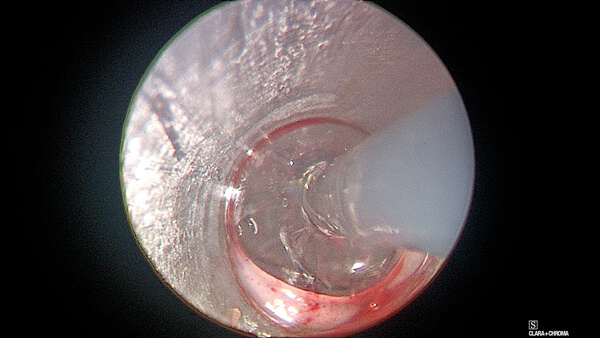
Figure 3. Balloon dilatation.
If the main point of pressure shifts away from the site of the stricture, the balloon is deflated completely, repositioned and the process started again. Pressure is kept constant for about two to three minutes, then deflated and the next atmospheric pressure produced to provide an accurate incremental enlargement in balloon width, until an appropriate dilatation has been achieved (Figure 4).
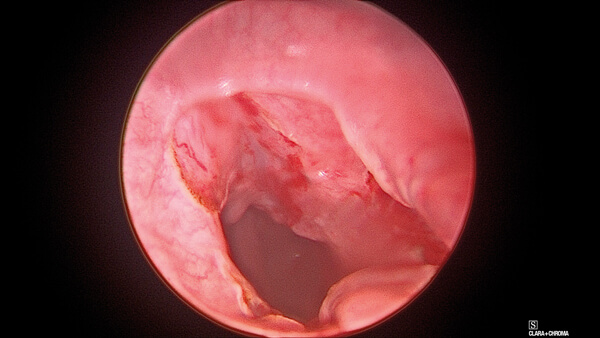
Figure 4. Outcome with dilatation achieved and without complications.
Caution is always advised in this procedure to avoid oesophageal perforation, and the judgement of when to stop is the surgeon’s responsibility. After that, careful inspection is advised for any perforation, and a fibrin sealant (TISSEEL) is applied for improved healing results. Excess TISSEEL should always be suctioned. In case of any doubt for iatrogenic perforation, an NG tube should be inserted under direct vision, through which the patient should be strictly fed until there is radiological confirmation and proof of no-leak. If there is suspicion for perforation, a gastrograffin swallow test at seven days postoperatively may be performed to confirm if healed or residual. Finally, on removal of the pharyngoscope, routine checks are made for any iatrogenic mucosal or dental damage in the oral cavity.
“The reader is reminded that the risk of perforation is around 2.6% and iatrogenic oesophageal injury accounting for the bulk of oesophageal trauma recorded”
Discussion
The use of CO2 laser in the oesophagus is not new. However, it has traditionally been reserved for refractory cases only [1]. With the proper experience, the CO2 laser may be used for a primary procedure, facilitating precise scar division prior to serial dilatation and giving better results than methods for dilatation alone. A novice surgeon is advised to use the ‘rule of three’, stating that no more than three sequential sizes of dilator should be used once medium resistance is felt. However, there is a variation in practice with some centres using sequential dilators up to size 15 Fr, regardless of the resistance on haptic feedback [2]. The surgeon’s judgement and experience is critical: the reader is reminded that the risk of perforation is around 2.6% and iatrogenic oesophageal injury accounts for the bulk of oesophageal trauma recorded [3].
Thereafter comes the role of TISSEEL in this surgery. Fibrin glues have been used for anastomosis in the GI tract, with many studies proving their efficacy and role in lowering the risk of leakage [4]. We utilise TISSEEL at the end of the procedure to minimise perforation risk, with good outcomes in our case series extending over eight years of its use.
Finally, an important additional aspect post stricture surgery is the management of pre-existent laryngopharyngeal refluxate. In our practice, we utilise a proton pump inhibitor and an alginate suspension to optimise patient symptomology and outcome perioperatively, preventing further unwanted sequalae post treatment [5]. This patient may require formal address of the long-standing hiatus hernia additionally; we continue to manage such cases as an integrated care of swallow (ICOS) MDT service linked with speech and language therapy, upper GI surgery, gastroenterology and gastro-intestinal tract dedicated radiologists.
References:
1. van Boeckel PGA, Siersema PD. Refractory Esophageal Strictures: What To Do When Dilation Fails. Current Treatment Options in Gastroenterology 2015;13(1):47-58.
2. Robles-Medranda C, Oleas R, Alvarado-Escobar H, et al. Treating simple benign esophageal strictures with savary-gilliard dilators: is the rule of three still necessary? Arquivos de Gastroenterologia 2019;56(1):95-8.
3. Quine MA, Bell GD, McCloy RF, Matthews HR. Prospective audit of perforation rates following upper gastrointestinal endoscopy in two regions of England. British Journal of Surgery 1995;82(4):530-3.
4. Plat VD, Bootsma BT, van der Wielen N, et al. The role of tissue adhesives in esophageal surgery, a systematic review of literature. International Journal of Surgery 2017;40:163-8.
5. Levin MD, Mendel’son G. Schatzki ring as a symptom of gastroesophageal reflux disease. Vestnik Rentgenologii i Radiologii 2015;1:5-15.
Declaration of Competing Interests: None declared.






