Nasal septal perforation repair has traditionally been a great challenge. Many surgical techniques are described, however the success rate of closure has often been poor. Experience from the use of pedicled vascularised mucosal flaps in skull base surgery has been used to dramatically change the reliability of septal perforation repair. Prof Richard Harvey and Marina Cavada discuss the procedure here.
Nasal septal perforation (NSP) is a defect through the mucosa and cartilage of the nasal septum. The causes of NSP include local trauma, local chondritis, autoimmune aetiologies, cauterisation for epistaxis, substance abuse, and unfortunately iatrogenic from septal surgery [1-3].
“In the past decade, the endoscopic endonasal approach has shown optimal surgical outcomes.”
The symptoms vary in intensity from mild to severe and can affect the quality of life of patients. Septal perforations located anteriorly are more likely to cause discomfort due to turbulent airflow resulting in a variety of symptoms including dryness, crusting, whistling, discharge, epistaxis, nasal obstruction, pain, and structural or cosmetic deformities [1-3].
Treatment consists of symptomatic control, but this is often unacceptable for younger patients to then submit to conservative interventions for life [2]. Several techniques have been described, however, in the past decade, the endoscopic endonasal approach has shown optimal surgical outcomes. Recent studies, utilising pedicled vascular anterior ethmoid artery (AEA) flaps have resulted in robust closure rates between 76.4% and 100% [2].
“Preparing an oversized flap is crucial for a successful outcome, and may feel uncomfortably large for a non-skull base surgeon.”
Operative technique
The procedure is performed under general anaesthesia and by using a 4mm 0° scope. Initially, the perforation size is measured by using a soft ruler (see Figure 1). Cottonoid pledgets embedded in 1% rupivicaine and adrenaline (1:2000) are placed bilaterally in the nasal cavity for topical vasoconstriction. The mucosa around the perforation, the floor of the nasal cavity and the nasal lateral wall, from where the flap is raised, are infiltrated with 1% rupivicaine and adrenaline (1:100.000).
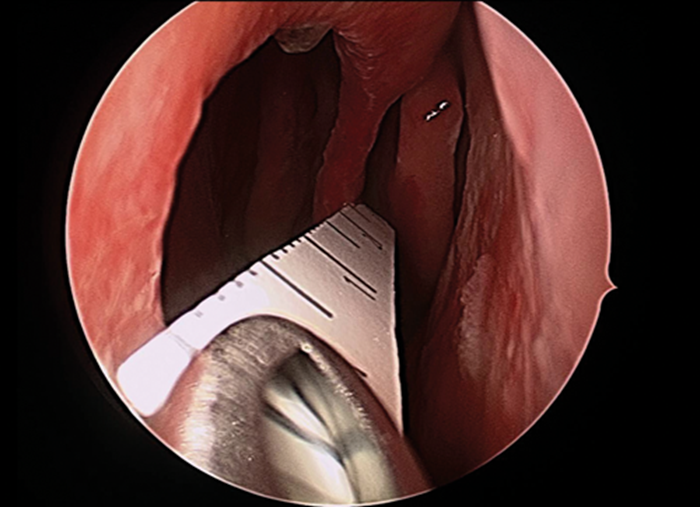
Figure 1. Endoscopic view of a soft ruler measuring the size of the nasal septal perforation.
A pedicled flap based on the anterior ethmoid artery is used to repair the perforation. A monopolar needlepoint tip diathermy (Megadyne 0016AM, Mathi, Italy) is used to mark out the vascular pedicle across the posterior limit, lateral limit on the floor of the nose, extending within the inferior meatus, superior septum margins as well as separating the perforation margins (see Figure 2A). The extension and location of this mark depends on the size and location of the perforation. However, preparing an oversized flap is crucial for a successful outcome, and may feel uncomfortably large for a non-skull base surgeon.
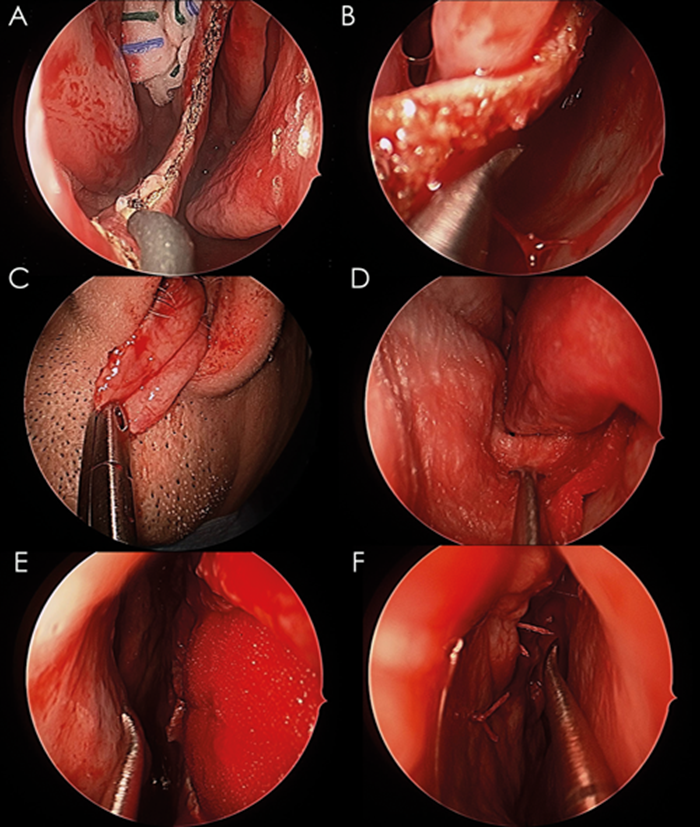
Figure 2. (A) A monopolar needlepoint diathermy is used to separate the margins of the perforation; (B) A pedicled flap is raised from the lateral wall of the nasal cavity; (C) The pedicled flap is mobilised to the upper lip; (D) collagen matrix covers the exposed areas on the floor and lateral wall of the nasal cavity; (E) An endoscopic view of the contralateral septum showing the collagen matrix graft filling the perforation; (F) The final outcome after rotating and suturing the pedicled flap.
The mucoperichondrium/mucoperiosteum around the perforation is separated from the cartilage or bone underneath, exposing as far as the sphenoid rostrum, the superior part of the septum and the nasal floor. A hemitransfixion incision, on the ipsilateral side to the AEA flap is performed to connect the caudal end of the septum with the perforation in order to insert a collagen matrix scaffold (DuraMatrix Stryker, Kalamazoo, USA) in between the cartilage and the mucosa.
The AEA flap is raised (see Figure 2B) and relocated posteriorly in the nasal cavity to avoid trauma and allow adequate space to place the collagen matrix sheet. It is important that the flap has enough mobility to reach the upper lip (see Figure 2C). The collagen matrix graft is inserted ipsilaterally and placed between the cartilage/bone and mucosa (see Figure 2D). Collagen matrix facilitates healing and regeneration of the host tissue, as well as acting as a scaffold for the new mucosa. It also protects exposed bone on the floor of the nasal cavity.
Initially, the flap is sutured in the anterior edge of the perforation with vicryl rapide 5/0 13mm (Ethicon, Johnson & Johnson, Somerville, New Jersey, USA). Several simple sutures are placed in the superior, inferior and posterior edges of the perforation (see Figure 2E). One or two through and through sutures only are used to reduce dead space and stabilise the layers used to repair the defect (see Figure 2F).
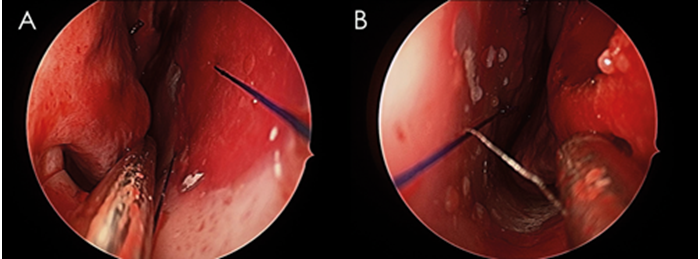
Figure 3. (A) A silastic sheet is used to protect the septum and floor of the contralateral side of the flap; (B) A silastic sheet on the side of the pedicled flap protects and fixes the flap, floor, and lateral wall of the nasal cavity.
Finally, two silastic sheets, which are intentionally oversized to protect exposed areas from crusting, are inserted bilaterally and sutured with prolene 4.0 (see Figure 3). A free mucosal graft can be used on the contralateral side.
A full video of NSP repair can be found at: www.youtube.com/watch?v=mO07in71Dfw&t=1s
Postoperative care
Saline irrigation and emollient ointments are used postoperatively from the first day while the silastic sheet remains in situ. The silastic sheet is left in place from three to six weeks. After removing the silastic sheet, patients are advised to maintain saline irrigation and ointment twice daily. Patients are seen three to six weeks postoperatively and then again at three months (see Figure 4).
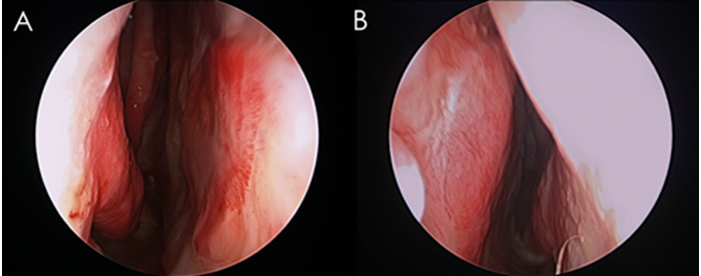
Figure 4. (A) Postoperative outcome after nasal septal perforation repair demonstrating complete closure of the nasal septal perforation three months after surgery; (B) Complete mucosalisation of the septum bilaterally three months after surgery. Figures reproduced with permission by Richard J Harvey.
“Use of a flap with an appropriate blood supply based on branches of the anterior ethmoid artery has resulted in more robust healing.”
Key points
- Use of a flap with an appropriate blood supply based on branches of the anterior ethmoid artery has resulted in more robust healing.
- The flap needs enough mobility to reach as far as the upper lip and is very large (potentially covers the remaining surface of the nasal cavity on that side).
- A collagen matrix facilitates healing allowing a scaffold for the new mucosa to integrate with over time.
- Placement of the silastic sheet bilaterally is essential to prevent crusting as well as enhancing healing of the area.
References
1. Smith DF, Albathi M, Lee A, et al. Upper lateral cartilage composite flap for closure of complicated septal perforations. Laryngoscope 2017;127(8):1767-71.
2. Dayton S, Chhabra N, Houser S. Endonasal septal perforation repair using posterior and inferiorly based mucosal rotation flaps. Am J Otolaryngol 2017;38(2):179-82.
3. Castelnuovo P, Ferreli F, Khodaei I, Palma P. Anterior ethmoidal artery septal flap for the management of septal perforation. Arch Facial Plast Surg 2011;13(6):
411-4.
SUMMARY
-
Experience from the use of pedicled vascularised mucosal flap in skull base surgery has been used to dramatically change the reliability of septal perforation repair.
-
Collagen matrix facilitates healing and regeneration of the host tissue, as well as acting as a scaffold for the new mucosa. It also protects exposed bone on the floor of the nasal cavity.
Declaration of competing interests:
Richard J Harvey is consultant with Medtronic, Olympus and NeilMed pharmaceuticals. He has received research grant funding from Meda Pharmaceuticals and Stallergenes and has been on the speakers’ bureau for BHR, Seqiris, Astra Zeneca, and Glaxo-Smith-Kline and Arthrocare.





