Repair of CSF leaks can be a challenging technical undertaking. In this article, the authors describe their use of a synthetic material to help with the successful repair of these leaks from the middle cranial fossa.
Erosion of the middle cranial fossa dura leading to cerebrospinal fluid (CSF) leak can occur as a result of multiple pathologies and the clinical presentations can be diverse. While it is considered a rare entity, there is evidence to suggest that the incidence may be increasing [1]. Predisposing factors include persistent intracranial hypertension, arachnoid granulations, meningoencephalocoele or possibly as a result of iatrogenic injury.
Recurrent meningitis, middle ear effusion, otorrhoea and retrograde rhinorrhoea via the eustachian tube can herald a possible lateral skull base defect and subsequent CSF leak. Investigation commonly includes computed tomography (CT), magnetic resonance imaging (MRI) and, at times, cisternography [1,2]. These enable characterisation and localisation of the middle fossa defect and subsequent surgical planning.
Approaches for CSF leak repair include a purely middle cranial fossa (MCF) approach, a transmastoid approach, or a mixture of the two [1-3]. The MCF approach can provide excellent exposure to large defects but comes at the expense of requiring temporal lobe retraction. Transmastoid approaches reduce manipulation of the brain and may be associated with reduced hospital stays and requirement for lumbar drains [3]. A combined approach involving a transmastoid approach with mini craniotomy can allow visualisation of the defect through the mastoid, and fashion an appropriately-sized mini craniotomy through which an extradural graft can be placed with minimal retraction.
A variety of materials have been employed to facilitate repair: autologous, allogeneic and synthetic. A robust repair is essential to prevent the spread of meningitis or intracranial infections from the middle ear and mastoid. Traditionally, pericranium, abdominal fat, temporalis and bone grafting have been used to provide multi-layered reconstruction [1-4]. While these tissues may be more biocompatible, there can be donor site morbidity, and when dealing with large defects, there may not be sufficient autologous material. Allogeneic materials like fetal bovine collagen-based dural matrices have also been described to be used for skull base repair which, while obviating many of the disadvantages of autologous material, still carries a risk of immune reactivity and theoretical transmission of Creutzfeldt-Jakob Disease.
Lately, the authors have favoured non-absorbable, synthetic, non-biological material (Neuro-patch® from B Braun Medical Ltd, Sheffield, UK) for middle fossa dura repairs using a combined, transmastoid middle fossa approach. Neuro-patch® is fibred microporous fleece manufactured from a purified polyesterurethane; it is purely synthetic, non-absorbable and can be used in large volumes.
Technical description
We describe our approach for lateral skull base repair; a transmastoid approach with middle fossa mini craniotomy with non-absorbable, non-biological, synthetic dura sheet.
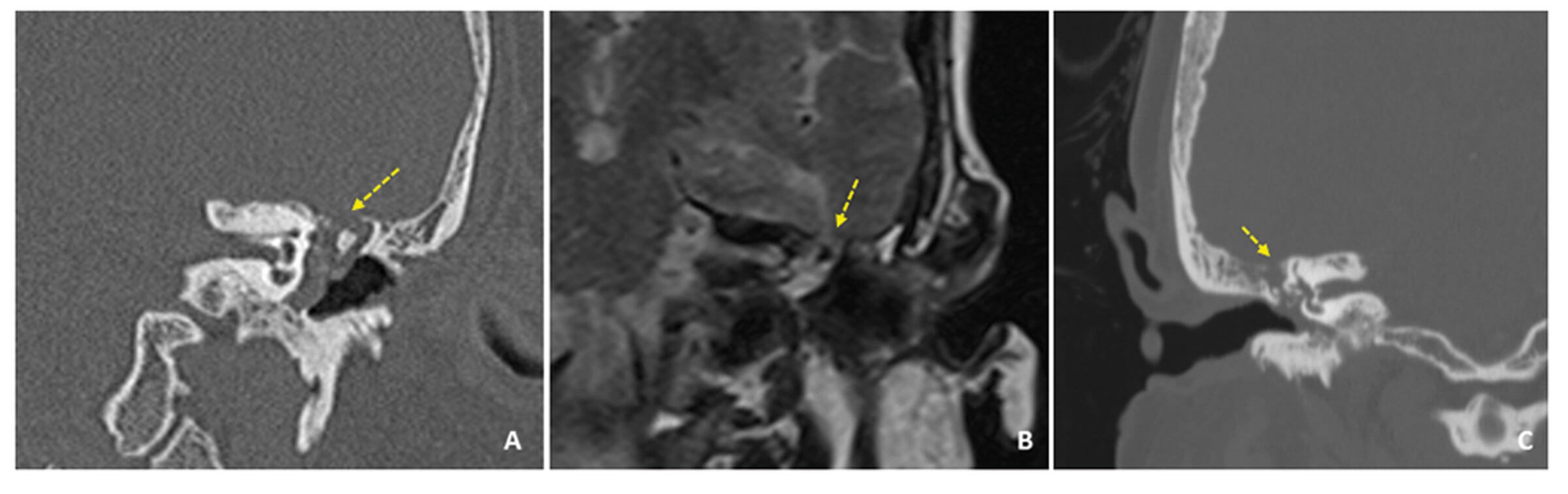
Figure 1. Examples of tegmen defects with meningoceles: left meningocele on coronal plane CT temporal bones (A); and on post-gadolinium T1-weighted coronal plane MRI (B); small defect on the right side in patient with CSF leak and recent meningitis on coronal plane CT temporal bones (C) (highlighted with arrows).
We advocate dual modality imaging of the temporal bone when a middle fossa defect is suspected; CT and MRI are essential in delineating the bony and soft tissue anatomy respectively (Figure 1).
The approach is initially similar to a standard mastoid exploration, with the patient supine, and post-auricular incision. This incision is more superiorly based in order to improve access and visualisation of the middle fossa dura for mini craniotomy. Cortical mastoidectomy is undertaken and the dura is identified, and overlying bone is thinned according to the defect location and size. The defect is identified and skeletonised, any meningo/encephalocoele can be excised or reduced. A mini craniotomy is developed drilling through the cortical bone lateral to the defect so that the middle fossa dura/encephalocoele can be elevated through the craniotomy to facilitate underlay of reparative materials. The site of the craniotomy depends on the precise location of the defect and is usually in continuity with the drilled-out mastoid.
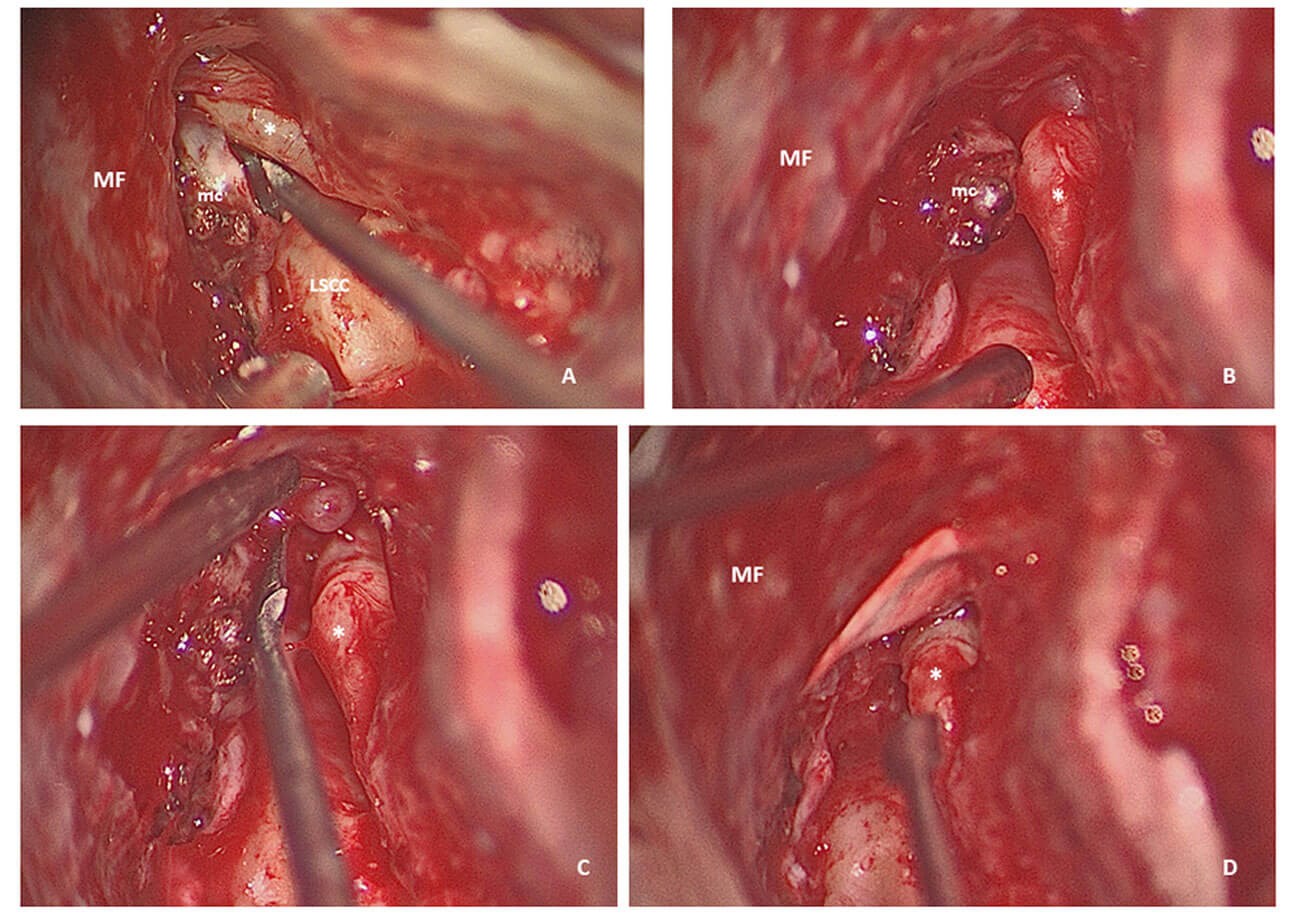
Figure 2. Right meningocele (mc) just over the incus (*); middle fossa (MF) has been exposed to gain better access and allow elevation of the dura for placing the graft (A); the meningocele is being resected (B) and the dura is being elevated off the tegmen (C) to allow the placement of the artificial dura (D) without disrupting the ossicles (LSCC: lateral semicircular canal).
A multi-layered approach is taken using temporalis fascia in underlay technique and the synthetic dura material placed between the remaining dura and the tegmen (Figure 2).
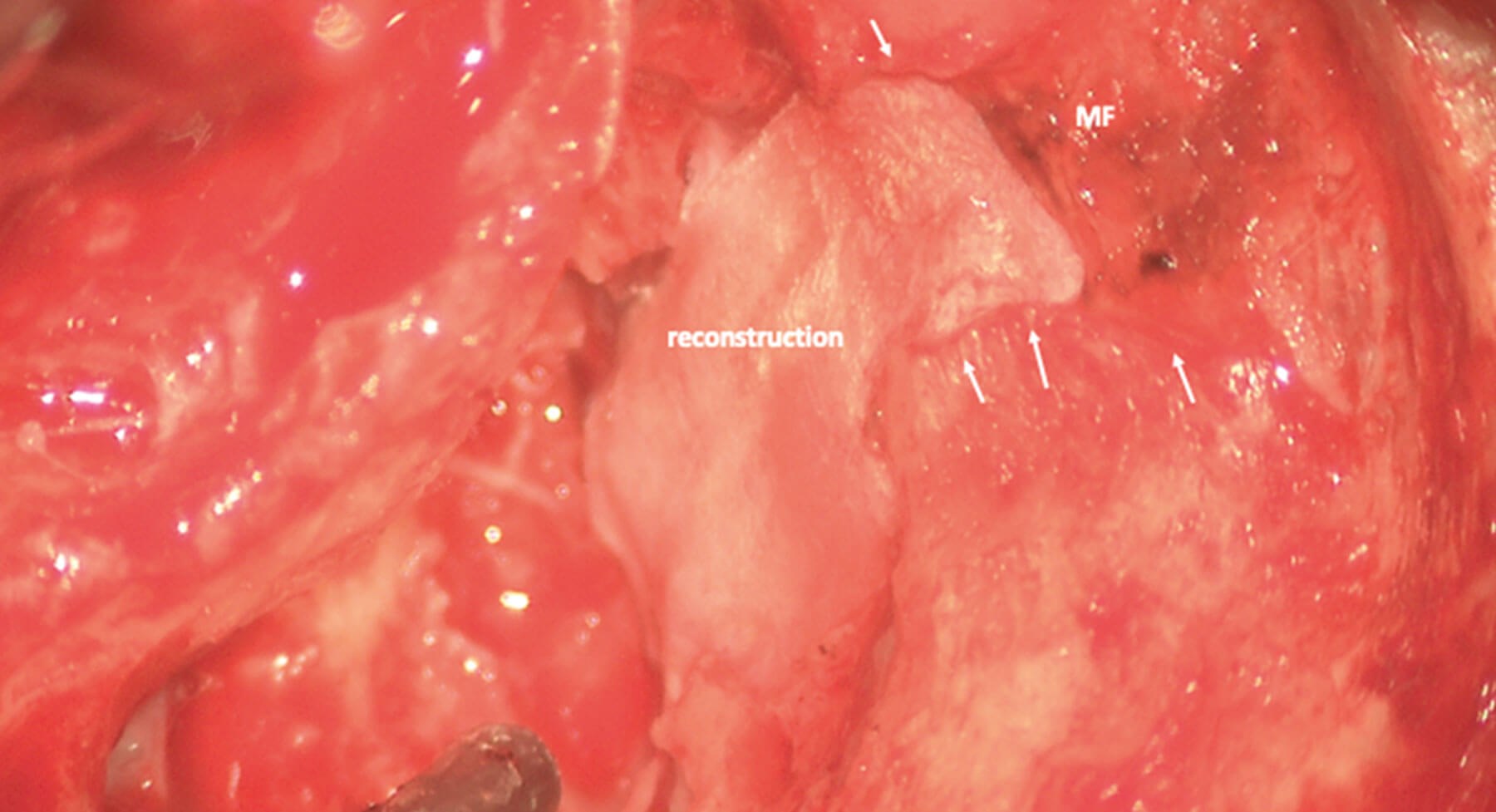
Figure 3. Left large middle fossa (MF) defect reconstruction through the combined transmastoid/middle-fossa approach showing the reconstruction as well as the mini craniotomy (arrows) that allowed careful elevation of the MF.
Once the repair is completed, an intraoperative Valsalva manoeuvre is performed to ensure the grafts are in good position with no residual leak/herniation of intracranial contents. Using this approach, we have avoided the use of a lumbar drain (Figure 3). Patients are observed as inpatients for 48 hours postoperatively under reasonable bed rest and clear advice, and are typically discharged following this period.
Discussion
There is a plethora of approaches and materials used for lateral skull base repair. We present a method, which involves minimum, if any, retraction of the middle fossa, and allows excellent visualisation and access to defects. The authors have found this approach particularly helpful for defects overlying the ossicles, as it allows robust repair without affecting the ossicular chain. The procedure is well-tolerated, and patients are discharged 48 hours following surgery. The use of synthetic material as an underlay graft in our hands provides an airtight closure of middle fossa defects without the use of a postoperative lumbar drain. The largest study of its use as a dural substitute found no increased risk of infection or recurrent CSF leak when compared with non-synthetic materials in craniectomy [4]. The authors of this study raised the issue of increased extra-axial bleeding with synthetic material in craniectomies; however, bleeding is not a commonly encountered complication of transmastoid surgery and this finding may be less applicable to the neuro-otologist.
Such non-absorbable, non-biological, synthetic material can be a useful tool in the arsenal when dealing with the lateral skull base and should be considered a valuable alternative to autologous and allogeneic grafts, particularly in the context of large defects.
References
1. Nelson RF, Gantz BJ, Hansen MR. The rising incidence of spontaneous cerebrospinal fluid leaks in the United States and the association with obesity and obstructive sleep apnea. Otol Neurotol 2015;36[3]:476-80.
2. McNulty B, Schutt CA, Bojrab D, Babu S. Middle Cranial Fossa Encephalocele and Cerebrospinal Fluid Leakage: Etiology, Approach, Outcomes. J Neurol Surg B Skull Base 2020;81(3):268-74.
3. Perez E, Carlton D, Alfarano M, Smouha E. Transmastoid repair of spontaneous cerebrospinal fluid leaks. J Neurol Surg B Skull Base 2018;79(5):451-7.
4. Huang YH, Lee TC, Chen WF, Wang YM. Safety of the Nonabsorbable Dural Substitute in Decompressive Craniectomy for Severe Traumatic Brain Injury. J Trauma 2011; 71(3):533-7.







