Reconstruction of the pinna is one of the most challenging procedures in facial plastic surgery. Although there has been significant progress since one of the earliest recorded descriptions by Sushruta in 600 BC, the complex three-dimensional structure of the pinna and the anatomy of the cartilage and overlying skin, contribute to the challenges of reconstruction [1]. In this article, Nigel Koo Ng and Saghir Sheikh describe a technique for reconstruction of the partial pinna using autologous costal cartilage with a split skin graft in a single-stage procedure.
Introduction
Patients requiring reconstruction of the pinna usually present as a result of congenital abnormalities, trauma or malignancy. For small defects of the pinna, there are simpler surgical techniques for repair and we have found that partial defects involving the helical rim and measuring less than 2cm, can often be repaired satisfactorily with a chondrocutaneous flap. For larger defects of the pinna, treatment options include a prosthesis or surgical reconstruction with alloplastic or autologous material.
The most common material currently used for surgical reconstruction of the pinna is autologous costal cartilage, which is considered to be the material of choice in autologous reconstruction. Tanzer [2,3] introduced the autologous costal cartilage graft technique in 1959 and since then, there have been further modifications with work done by Brent [4-7], Nagata [8-14], Firmin [15,16] and others. There are numerous modifications in reconstructive techniques, with variations including timing of surgery and the number and sequence of stages. Nagata published his two-stage total reconstruction for microtia [8], which was a reduction in the number of stages previously reported.
Case report
We describe a modification of Nagata’s technique, using autologous costal cartilage, a temporoparietal fascia flap and a split skin graft, in a single-stage procedure for partial pinna reconstruction. From our experience, consisting predominantly of adult patients who had sustained significant trauma (often human or animal bites) to the pinna, we have found the following technique to produce reliable and good results.
Preoperatively
The patient undergoes a full clinical assessment and management options including the benefits and risks are discussed. Complications of partial pinna reconstruction may occur from harvesting costal cartilage, from harvesting the temporoparietal fascia (TPF) flap or at the reconstructive site. Specific complications include pneumothorax, chest wall deformities, alopecia, injury to the frontal branch of the facial nerve, graft and flap failure, infection, bleeding, cartilage resorption and an unsatisfactory result.
Patient factors, the patients’ motives for reconstruction and the state of the residual pinna, local tissues and potential donor sites are evaluated. In children, reconstruction is usually not performed generally until after the age of 8 to 10 years old and provided that the chest circumference at the level of the xiphoid process is at least 60cm.
Photographs are obtained and a template of the pinna is created, based on the pinna for reconstruction and also the contralateral pinna.
Intraoperatively
The procedure is performed under general anaesthetic and an intravenous dose of antibiotics (co-amoxiclav) is given on induction. The steps involved include:
- Harvesting costal cartilage.
- Harvesting a pedicled temporoparietal fascia (TPF) flap.
- Preparation of the pinna.
- Sculpting of the costal cartilage and placement of the cartilage framework.
- Covering the cartilage framework with the TPF flap and a split skin graft.
Harvesting costal cartilage – (Figure 1)
Conjoined costal cartilage of the sixth and seventh ribs is harvested en-bloc. This is performed through an oblique incision on the chest, about 2.5-4 cm long and centred over the cartilage of the six and seventh ribs. The cartilage is carefully harvested, with the size of the piece dependent on the size of the pinna defect. The rib perichondrium is left intact and the site is checked for a pneumothorax by temporarily covering the area with a pool of normal saline and performing a valsalva manoeuvre, whilst observing for any bubbles. The perichondrium is closed with a 4-0 polydioxanone (PDS) suture and the chest incision is closed in layers.
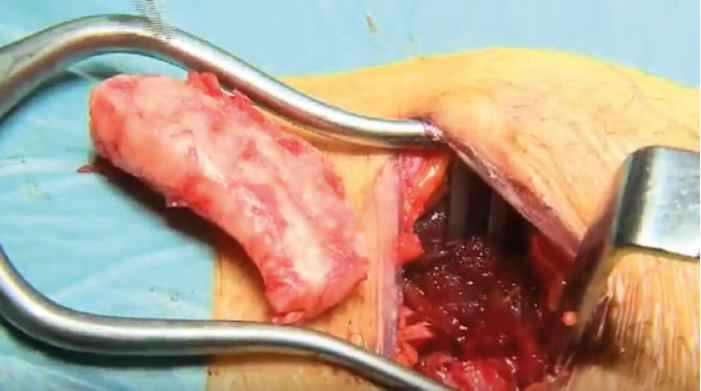
Figure 1.
Harvesting a pedicled temporoparietal fascia (TPF) flap – (Figure 2)
Exposure of the TPF is via a Y-shaped incision which is created, initially, very superficially in order to avoid damaging the TPF. Anterior, posterior and superior skin flaps are elevated to expose the TPF, with particular care taken anterior to the superficial temporal artery, to avoid injury to the frontal branch of the facial nerve. Once the required size of flap is exposed, it needs to be elevated, taking care to protect the vascular base of the flap with the feeding and draining vessels (usually the superficial temporal vessels) under direct vision. Flap elevation starts superiorly and is much simpler and faster than exposing the TPF, as dissection is in the loose areolar avascular plane from the deep temporal fascia.

Figure 2.
Preparation of the pinna
Skin flaps are raised around the residual pinna cartilage and the edges are freshened.
Sculpting of the costal cartilage and placement of the cartilage framework – (Figures 3-6)
The costal cartilage graft is sculpted and carved (using specially designed instruments) based on the template created preoperatively, to form the framework of the reconstructed pinna. We attempt to create the framework using a single piece of cartilage if possible, but otherwise other pieces of cartilage may be attached to the framework as required. The cartilage framework needs to be secured to the residual cartilage of the pinna; this is performed by bevelling the free edge of the graft and placing it just posterior to the existing pinna cartilage to reduce any step deformity, and the whole structure is secured with stainless steel wire sutures.

Figure 3.
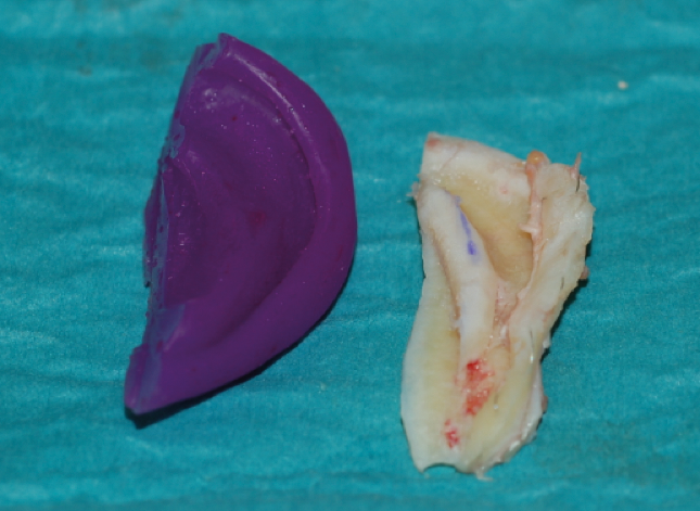
Figure 4.

Figure 5.
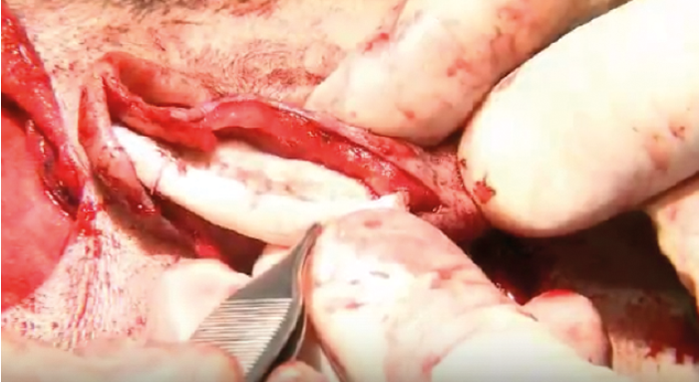
Figure 6.
Covering the cartilage framework with the TPF flap and a split skin graft – (Figures 7-9)
The framework is wrapped with the harvested TPF flap which provides a highly vascular, thin and pliable bed for a split skin graft. The TPF flap is secured with a 5-0 polydioxanone (PDS) suture, and a split skin graft harvested from the forearm or thigh is secured with a 6-0 polyglactin (Vicryl) suture. Two butterfly drains are inserted and a quilting stitch with 5-0 polyglactin (Vicryl) is also used to reduce the risk of a haematoma formation.

Figure 7.

Figure 8.

Figure 9.
“We have found this single-stage procedure based on Nagata’s method to reliably produce good results in partial reconstruction of the pinna with very few complications.”
Postoperatively
The patient and reconstructive site are closely monitored and the patient is admitted overnight. It is important that the vascularity of the reconstructive site is not compromised. If there are no problems, the patient is allowed home the following day with a one-week course of oral antibiotics. The patient returns for review after two days and, if there is no haematoma, the butterfly drains are removed. The patient is then reviewed in clinic initially every week to ensure satisfactory healing.
Discussion
We have found this single-stage procedure based on Nagata’s method to reliably produce good results in partial reconstruction of the pinna with very few complications, which is consistent with the authors of other case series based on Nagata’s method. Occasionally a revision procedure is required to make a small alteration, and we usually perform this two to three months after the initial operation. One of the disadvantages of using a split skin graft is that there can be a difference in skin colour but, from our experience, we have found patients are generally very pleased with the final result.
Summary
- Reconstruction of the pinna is one of the most challenging procedures in facial plastic surgery.
- Patients requiring reconstruction of the pinna usually present as a result of congenital abnormalities, trauma or malignancy.
- For large defects of the pinna, the treatment options include a prosthesis or surgical reconstruction with alloplastic or autologous material.
- The most common material currently used for surgical reconstruction of the pinna is autologous costal cartilage.
- We have found that a modification of Nagata’s technique using autologous costal cartilage, a temporoparietal fascia flap and a split skin graft in a single stage procedure provides reliable and good results in partial pinna reconstruction.
References
1. Kobus K, Szczyt M, Latkowski I, Wojcicki P. Reconstruction of the auricle. British journal of plastic surgery 2002;55(8):645-51.
2. Tanzer RC. Total reconstruction of the external ear. Plastic and reconstructive surgery and the transplantation bulletin 1959;23(1):1-15.
3. Tanzer RC. An analysis of ear reconstruction. Plastic and reconstructive surgery 1963;31:16-30.
4. Brent B. Ear reconstruction with an expansile framework of autogenous rib cartilage. Plastic and reconstructive surgery 1974;53(6):619-28.
5. Brent B. The correction of mi-rotia with autogenous cartilage grafts: I. The classic deformity.? Plastic and reconstructive surgery 1980;66(1):1-12.
6. Brent B. The correction of microtia with autogenous cartilage grafts: II. Atypical and complex deformities. Plastic and reconstructive surgery 1980;66(1):13-21.
7. Brent B. Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal experience with 1200 cases. Plastic and reconstructive surgery 1999;104(2):319-34; discussion 35-8.
8. Nagata S. A new method of total reconstruction of the auricle for microtia. Plastic and reconstructive surgery 1993;92(2):187-201.
9. Nagata S. Modification of the stages in total reconstruction of the auricle: Part I. Grafting the three-dimensional costal cartilage framework for lobule-type microtia. Plastic and reconstructive surgery 1994;93(2):221-30; discussion 67-8.
10. Nagata S. Modification of the stages in total reconstruction of the auricle: Part II. Grafting the three-dimensional costal cartilage framework for concha-type microtia. Plastic and reconstructive surgery 1994;93(2):231-42; discussion 67-8.
11. Nagata S. Modification of the stages in total reconstruction of the auricle: Part III. Grafting the three-dimensional costal cartilage framework for small concha-type microtia. Plastic and reconstructive surgery 1994;93(2):243-53; discussion 67-8.
12. Nagata S. Modification of the stages in total reconstruction of the auricle: Part IV. Ear elevation for the constructed auricle. Plastic and reconstructive surgery 1994;93(2):254-66; discussion 67-8.
13. Nagata S. Total auricular reconstruction with a three-dimensional costal cartilage framework. Annales de chirurgie plastique et esthetique 1995;40(4):371-99; discussion 400-3.
14. Nagata S. Secondary reconstruction for unfavorable microtia results utilizing temporoparietal and innominate fascia flaps. Plastic and reconstructive surgery 1994;94(2):254-65; discussion 66-7.
15. Firmin F. Ear reconstruction in cases of typical microtia. Personal experience based on 352 microtic ear corrections. Scandinavian journal of plastic and reconstructive surgery and hand surgery / Nordisk plastikkirurgisk forening [and] Nordisk klubb for handkirurgi 1998;32(1):35-47.
16. Firmin F. State-of-the-art autogenous ear reconstruction in cases of microtia. Advances in oto-rhino-laryngology 2010;68:25-52.
Declaration of Competing Interests: None declared.
Acknowledgements
This subject was presented at The ENT Scotland Summer Meeting on 9 May 2014 by the senior author Mr Sheikh.






