Occasionally, getting access to the larynx for an intervention can be challenging. Markus Hess and Susanne Fleischer describe a novel way to perform laser treatment in such difficult instances.
Fibre guided office-based endolaryngeal laser surgery has developed to be a preferred therapeutic option in many patients. However, when some of these patients have an excessively pronounced gag response making in-office laser surgery impossible and when, furthermore, direct suspension microlaryngoscopy as the most common alternative is not performable because of a difficult-to-expose larynx, only limited options for intervention are available.
Because of recent improvements in (a) percutaneous injection techniques using transthyrohyoid endolaryngeal approaches as well as (b) new developments in fibre guided laser technology with thin glass fibres, we sought to apply a combination of these approaches to the benefit of the above-mentioned patient group.
Method and results
Our patient (male, aged 33) with progressive adult onset recurrent respiratory papilloma (RRP) could not be treated satisfactorily with in-office transnasal fibre guided photoangiolytic laser surgery due to pronounced gag response and hypersalivation and, unfortunately, his larynx also could not be entirely exposed during direct suspension microlaryngoscopy.
However, we knew that with a small laryngoscope (Kleinsasser types ‘D’ and ‘K’, Karl Storz, Germany) and with the help of a 28cm long rigid 70° telescope (No. A22003A, Olympus Comp, Germany) connected to a 4K camera system (Arthrex AR-3210-0018, Synergy Comp), indirectly his endolaryngeal lumen could be visualised on a monitor during general anaesthesia when a very small 5.5 endotracheal tube (ETT) was used. With adequate endolaryngeal visualisation during general anaesthesia, a transthyrohyoid, percutaneously routed straight 20G 70mm long cannula (Sterican hypodermic needle, B. Braun, Germany) with a laser fibre (300µm bare fibre, A.R.C. Laser Comp, Nuremberg, Germany) inside was inserted until the tip was placed in the endolarynx at the inferior level of the petiole. The cannula was left in place for further endolaryngeal guiding of the thin laser glass fibre for RRP treatment.
The laser glass fibre could easily be advanced and retracted within the cannula and its tip was proud of the tip of the cannula bevel by a few millimetres. This is always visualised on the monitor. With joystick-like movements of the cannula’s hub combined with advancement or retraction of the glass fibre, the glass fibre tip could be positioned close to or into the papilloma tissue at different endolaryngeal sites. With a photoangiolytic laser at 445nm wavelength (WOLF TruBlue®, A.R.C. Laser Comp, Nuremberg, Germany) we treated RRP at different sites, including the free edge of both vocal folds, inferior aspects of vocal folds, ventricular folds, inside of Morgagni’s ventricles, and papilloma within the anterior commissure. We used various laser effects such as photoangiolysis, coagulation, carbonisation, and vaporisation (see also Hess et al [1]; Mallur et al [2]). For all laser applications during anaesthesia, laser safety precautions were complied with, especially lowering of ventilation oxygen saturation far below 50% during anaesthesia. After surgery and retracting the laser glass fibre together with the 20G guiding cannula, off-label intralesional injection of Cidofovir was performed with a smaller cannula (23G and 60mm long).

Figure 1. Percutaneous, cannula guided glass fibre laser surgery during direct
microlaryngoscopy and visualisation with an angled 70° telescope.
The surgeon is directing the glass fibre with joystick-like movements with his right hand.
Left hand holds telescope and camera. Anaesthetist in background with laser protecting glasses.
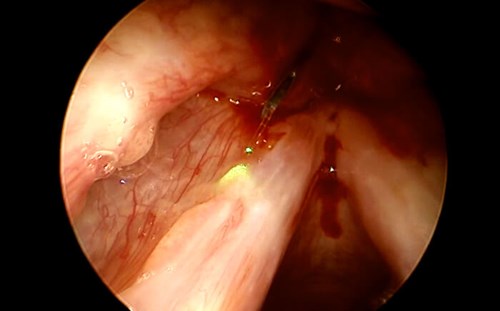
Figure 2. Endolaryngeal visualisation with 70° endoscope.
The bevelled tip of a 20G cannula and the 300µm glass fibre can be seen.
Pilot beam (green) directed onto left vocal fold and papilloma lesions.
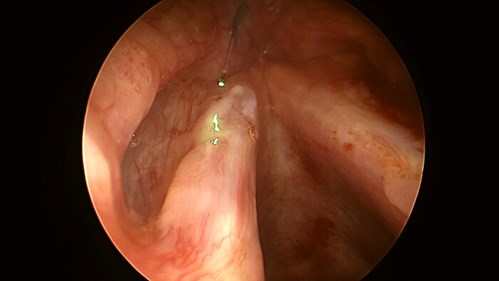
Figure 3. Similar aspect to Figure 2. Here, the cannula tip is not clearly visible, because the glass fibre is more advanced.
The surgeon is about to coagulate the papilloma on left vocal fold surface.
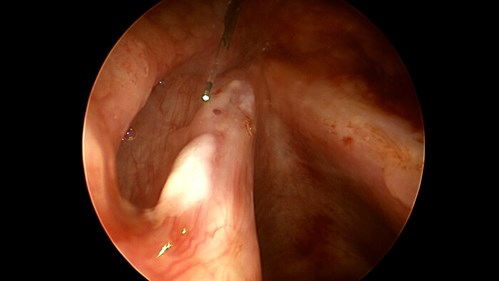
Figure 4. Same operation as in Figure 3. Shortly after laser intervention, the papilloma is blanched (coagulated).
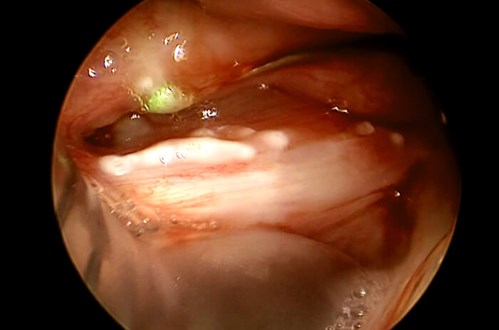
Figure 5. Same operation as in Figure 3 and 4. Now with the telescope rotated, visualisation of the left endolarynx is achieved.
Using the rigidity of the 20G cannula, the ventricular fold was moved aside so that the laser
glass fibre could easily be advanced into the lesion (green pilot beam light within the lesion).
Discussion
We report on a new technique for percutaneous transthyrohyoid laser surgery of the endolarynx. The technique allows one to deliver laser light into the larynx via glass fibre in cases where office-based indirect surgery, as well as direct microlaryngoscopy, is not possible. We have of course evaluated the option of routing a channelled flexible endoscope via the rigid laryngoscope into the endolaryngeal lumen, or during laryngeal mask ventilation.
However, this only enables limited access to some endolaryngeal regions, but not ‘around the corner’ like into the recesses of the lateral part of Morgagni’s ventricles or the inferior aspect of the vocal folds. With the percutaneously inserted cannula, access to all these regions is possible. Routing via different techniques such as cricothyroid or transcartilage approaches can also help but was not necessary in this case.
Thus, all endolaryngeal areas can be reached with such a percutaneous technique. In this patient, we were able to direct the laser glass fibre tip for laser surgery to all endoluminally visible surfaces. In contrast to transorally routed glass fibre laser surgery, we were also able to reach the inferior surfaces of the vocal folds and the very tricky-to-reach region, the far lateral parts of Morgagni’s ventricles, as well as the inferior lateral aspect of the ventricular folds inside the ventricle. For reasons of having enough space for the angled telescope and degrees of freedom for movements of the laser fibre, we decided to not use a thick laser safety tube, which would have been compromising the entire procedure by the significantly bigger size of its outer diameter. It is crucial that oxygen levels have to be as low as possible (in most cases it can be approximately 25%), but for sure lower than 50%.
“The technique allows one to deliver laser light into the larynx via glass fibre in cases where office-based indirect surgery, as well as direct microlaryngoscopy, are not possible”
According to the new ELS nomenclature [3], we are not sure how to abbreviate our technique – maybe TOLMS (transoral laser microsurgery) in general anaesthesia and TOFLS (transoral flexible laser surgery) when used in the office. The armamentarium for interventional laryngology can now be broadened by percutaneous lasers such as blue laser, KTP, Argon, Diode, Neodym-YAG etc. Also, other lesions than RRP can be addressed, such as Reinke’s edema, polyps, contact granuloma, dysplasia, biofilm, ectactic vessels and many more. Smaller glass fibres enable more precise tissue interventions and not only debulking. And of course, in patients who tolerate endoscopy, in-office percutaneous laser surgery is possible when laser fibres cannot be routed transnasally or transorally.
Conclusions
In patients with difficult-to-expose larynges in suspension microlaryngoscopy and impossible transnasal or transoral office laser approach, this new percutaneous laser technique can be a very helpful alternative to achieve access to the endolarynx while avoiding open neck surgery. A 20G cannula serves as an introduction tool and joystick-like guiding instrument, enabling access even to endolaryngeal regions that cannot be accessed easily in transnasal flexible channelled endoscopy or in direct microlaryngoscopy. This approach extends our armamentarium for endolaryngeal surgery.
References
1. Hess M, Fleischer S, Ernstberger M. New 445 nm blue laser for laryngeal surgery combines photoangiolytic and cutting properties. Eur Arch Otorhinolaryngol 2018;275(6):1557-67.
2. Mallur PS, Johns MM 3rd, Amin MR, Rosen CA. Proposed classification system for reporting 532-nm pulsed potassium titanyl phosphate laser treatment effects on vocal fold lesions. Laryngoscope 2014;124(5):1170-5.
3. Remacle M, Arens C, Eldin MB, et al. Laser-assisted surgery of the upper aero-digestive tract: a clarification of nomenclature. A consensus statement of the European Laryngological Society. Eur Arch Otorhinolaryngol 2017;274(10):3723-7.
Further Reading
1. Clary MS, Milam BM, Courey MS. Office-based vocal fold injection with the laryngeal introducer technique. Laryngoscope 2014;124(9):2114-7.
2. Getz AE, Scharf J, Amin MR. Thyrohyoid approach to cidofovir injection: a case study. J Voice 2005;19(3):501-3.
All figures are provided by Deutsche Stimmklinik Management GmbH.
Declaration of Competing Interests: Markus Hess and Susanne Fleischer have consulted in the past with companies (in alphabetical order) as follows: ARC, Biolitec, Laryngograph, Lumenis, Olympus, Pentax, Storz, Wolf, Xion.