There have been many descriptions of soft tissue preparation in the era when subcutaneous tissue was routinely removed with the Nijmegen technique [1] or with the dermatome [2]. More descriptions continue to evolve with the advent of tissue preservation techniques, like ‘punch and drill’ [3], and the minimally invasive ponto surgery (MIPS) [4]. In this article, Adonye Banigo and Alex Bennett describe a simple ‘bus-stop incision’, which combines the benefits of access and excellent wound healing.
The bone-anchored hearing aid (BAHA) is a percutaneous device composed of an implant, abutment and an audioprocessor which transmits sound vibrations directly into the inner ear via an osseointegrated titanium screw (see Figure 1). It was introduced in clinical practice in the 1970s in Sweden [5]. BAHA is the brand name for a specific device from Cochlear®. However, a similar device is also made by Oticon® called the Ponto. This article refers to a BAHA as any percutaneous bone integrated hearing aid with a visible abutment. Bone anchored hearing aid placement is considered a core competence for an ENT surgeon in the UK [7].
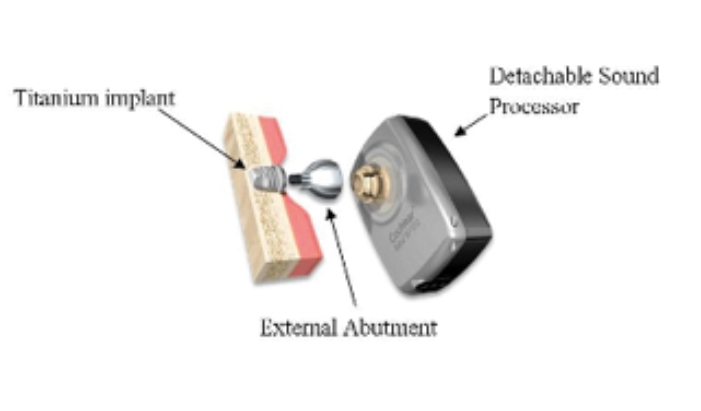
Figure 1. Components of the bone-anchored hearing aid. [6]
It is indicated for patients with conductive or mixed hearing loss, in whom a conventional amplification device is not suitable or contraindicated, and these patients should have adequate bone conduction pure-tone thresholds largely accepted as 45dBHL averaged over 0.5, 1, 2 and 4 kHz; although the most powerful BAHA sound processors can compensate for a sensorineural loss up to 65dBHL [8]. It is also indicated in patients with single-sided senorineural deafness (SSD) i.e. profound unilateral hearing loss (bone conduction on pure tone audiogram >90Dbhl [9]) where it acts like a surgically implanted version of the contralateral routing of signals (CROS) hearing aid, eliminating the head shadow of SSD and occlusion effects of CROS.
“A Plester self-retainer, which is two-pronged on one side with a blunt blade on the other, is placed in the wound to enable access to the bone for drilling, but also enables easy removal at the end of the procedure without snagging the wound edges.”
Soft tissue preparation
Soft tissue reactions around BAHA implants are a common occurrence, and prevalence rates have been quoted as high as 36% in children [10,11]. A review on skin complications associated with bone-anchored hearing aids concluded that the linear incision technique appears to be associated with lower skin complications [12]; however, in our experience, even this technique can give rise to skin tethering and drooping around the abutment leading to exposure of soft tissue resulting in infection (see Figure 2) [13].
Figure 2. (L-R) Drooping of skin from 2 o’clock to 6 o’clock with erythema and discharge, and tethering around abutment with some granulation tissue.
Technique
The operation is performed under local anaesthetic as a one-stage procedure where the implant and abutment are fitted at the same time. The BAHA site is identified and marked as per the manufacturer’s template, and the skin around this area is shaved. Skin thickness is measured before local anaesthesia infiltration to determine the correct length of abutment and the incision to be made over the implant site is marked with a cruciate pattern, with a 2-3cm vertical axis (cranio-caudal distance) (see Figure 3).

Figure 3. Cruciate pattern of incision.
Local anaesthesia is infiltrated and a 5mm skin punch biopsy (which corresponds to the diameter of the abutment shaft) is performed down to bone. The small cylindrical piece of soft tissue and skin is removed (see Figures 4 and 5).
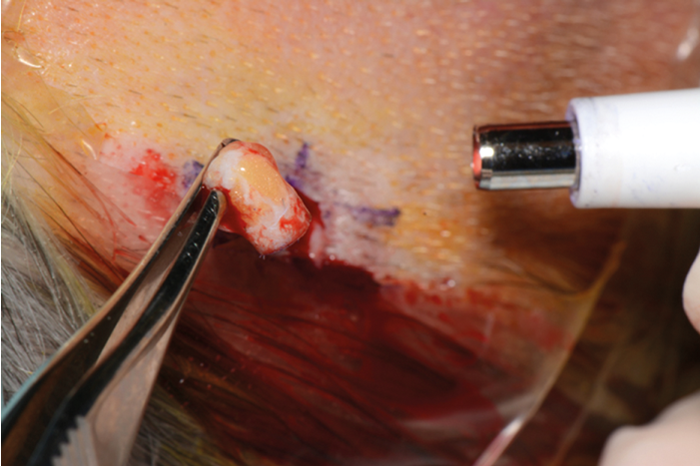
Figure 4. Cylindrical piece of skin removed with punch biopsy.
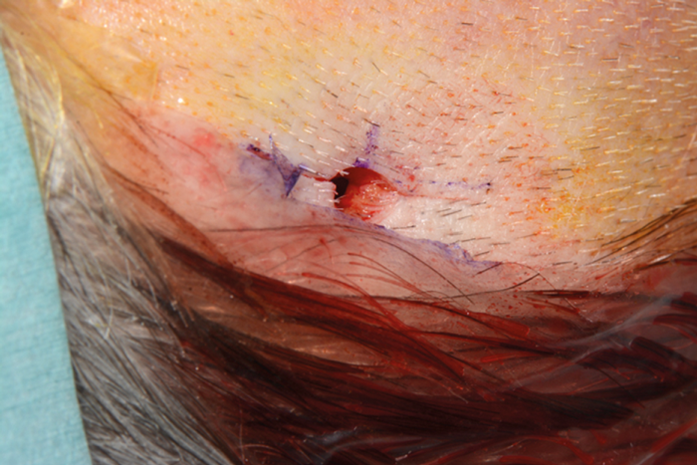
Figure 5. Circular defect created by punch biopsy.
Skin incisions are made which transect through the centre of the wound (see Figure 6).

Figure 6. Skin incisions made along marked sites.
The skin is not thinned. A Plester self-retainer (see Figure 7), which is two-pronged on one side with a blunt blade on the other, is placed in the wound to enable access to the bone for drilling but also enables easy removal at the end of the procedure without snagging the wound edges.
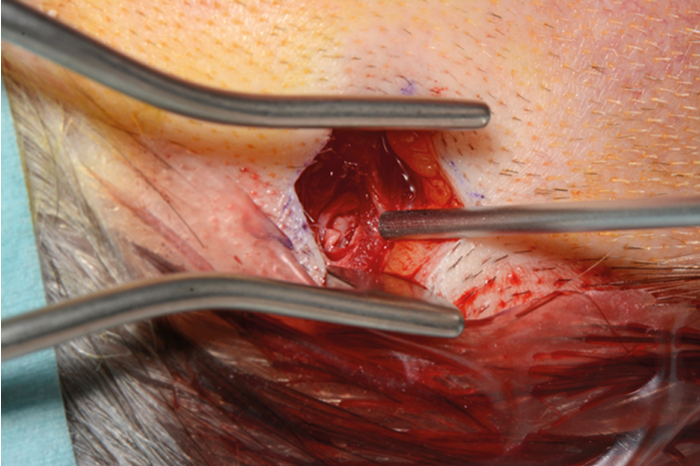
Figure 7. Plester self-retainer in-situ as implant site is being prepared.
The implant and abutment are fitted as per the manufacturer’s instructions, and the wound is closed with two interrupted nylon sutures (as shown in Figures 8 and 9) which are removed in seven days’ time. The bus-stop incision ensures that all the soft tissue and skin fit snugly around the abutment without stretching the skin. Discussion Postoperatively, patients are followed up in a week for removal of sutures, and at six weeks for fitting of the processor. In our experience, this technique provides tension-free wound closure around the abutment and excellent cosmetic results.
“In our experience, this technique provides tension-free wound closure around the abutment and excellent cosmetic results.”
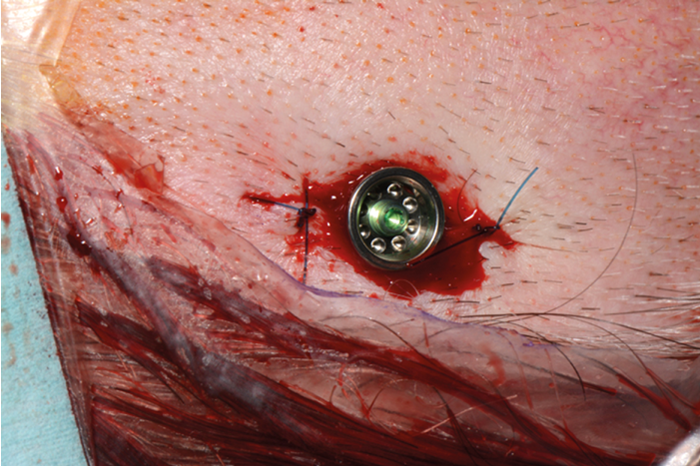
Figure 8. Abutment screwed onto implant with wound closed.
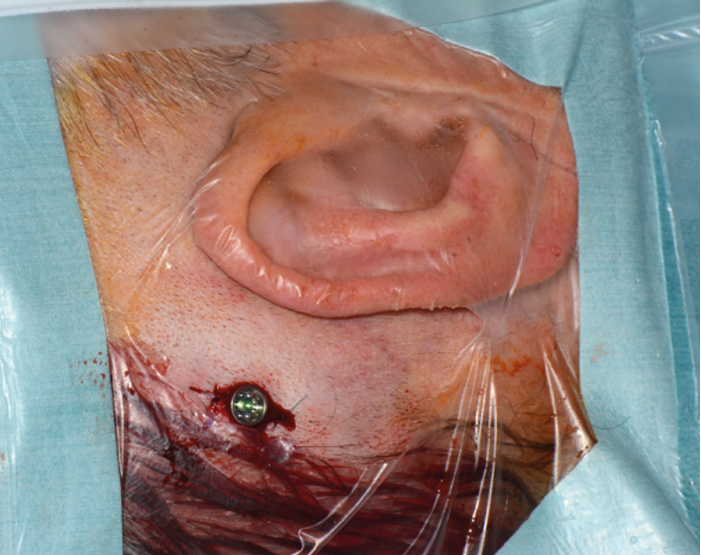
Figure 9. Wound closed with abutment and implant in-situ.
References
1. de Wolf MJ, Hol MK, Huygen PL, et al. Nijmegen results with application of a bone-anchored hearing aid in children: simplified surgical technique. Ann Otol Rhinol Laryngol 2008;117(11):805-14.
2. Van Rompaey V, Claes G, Verstraeten N, et al. Skin reactions following BAHA surgery using the skin flap dermatome. Eur Arch Otorhinolaryngol 2011;268(3):373-6.
3. Dumon T, Medina M, Sperling NM. Punch and Drill: Implantation of bone anchored hearing device through a minimal skin punch incision versus implantation with dermatome and soft tissue reduction. Ann Otol Rhinol Laryngol 2016;125(3):199-206 4. Oticon Medical AB. Ponto Bone Anchored Hearing System.
www.oticonmedical.com/~asset/
cache.ashx?id=44036&type=14&format=web
Last accessed December 2016.
5. Tjellstrom A, Lindstrom J, Hallen O, et al. Osseointegrated titanium implants in the temporal bone. A clinical study on bone-anchored hearing aids. Am J Otol 1981;2(4):304-10.
6. The Ear Foundation. Bone Conducting Hearing Implants.
www.earfoundation.org.uk/
hearing-technologies/bone-conducting-hearing-implants.
Last accessed December .2016
7. The Intercollegiate Surgical Curriculum. Educating the surgeons of the future.
www.iscp.ac.uk/static/public/
gs_curriculum_august_2013.pdf
Last accessed December 2016.
8. Cochlear Candidate Selection Guide. Available at
www.cochlear.com
Last accessed April 2016.
9. Oticon Candidate Selection Guide.
www.oticonmedical.com/~asset/
cache.ashx?id=34821&type=14&format=web
Last accessed December 2016.
10. Tzortzis S, Tzifa K, Tikka T et al. A ten-year review of soft tissue reactions around percutaneous titanium implants for auricular prosthesis. Laryngoscope 2015;125(8):1934-9.
11. Lusting LR, Arts HA, Brackmann DE, et al. Hearing Rehabilitation using the BAHA bone-anchored hearing aid: results in 40 patients. Otology & Neurotology 2001;22:328-34.
12. Mohamad S, Khan I, Hey SY, Hussain SS. A systematic review on skin complications of bone-anchored hearing aids in relation to surgical techniques. Eur Arch Otorhinolaryngol 2016;273(3):559-65.
13. Conejeros TJM, Galofre DJ, Puchades MV, et al. Comparison of skin complications between dermatome and U-graft technique in BAHA surgery. Acta Otorinnolaringol Esp 2009;60(6):422-7.
Declaration of competing interests: None declared.







