Surgery for the eye complications of Grave’s disease is an area that, over the years, ENT has become more and more involved in due to our ability to access the orbit endoscopically. In this article, the authors describe their technique for transnasal endoscopic orbital decompression in the context of Grave’s ophthalmopathy. This involves removal of the medial and inferior walls of the orbit – a ‘two wall’ approach - with the aim of reducing orbital pressure.
Indications
The commonest indication is Grave’s ophthalmopathy, in which decompression addresses the complications of retrobulbar inflammation and fibrosis; namely exophthalmos (which causes both cosmetic deformity and exposure keratitis), diplopia and optic nerve compression. However, the same technique can be used for retrobulbar haemorrhage decompression, subperiosteal abscess drainage or accessing tumours of the orbital apex.
Preop workup
Close collaboration with an oculoplastic ophthalmologist is essential. Severe disease may warrant concurrent medial and lateral tarsorrhaphies (permanently suturing the eyelids together at each end) to further reduce corneal exposure. A ‘three wall’ technique – whereby the ophthalmologist performs a lateral wall decompression – gives a more balanced decompression, resulting in lower rates of diplopia whilst improving decompression. A CT scan of the sinuses is mandatory, both for assessing surgical landmarks and mapping of the intraoperative image guidance system. The patient is also consented for a septoplasty if nasal septal deformities are likely to hinder surgical access. If both eyes are affected, we perform staged procedures unless there is concern regarding pressure on the optic nerve, in which case bilateral decompressions are performed.
Step 1 – preparation
The patient is positioned supine in the reverse Trendelenburg position prior to draping with a head towel, leaving the eyes exposed. The intraoperative navigation system is set up and calibrated (Karl Storz Surgical Cockpit® - Karl Storz, Germany). One in 1000 adrenaline-soaked patties are placed both medial and lateral to the middle turbinate to achieve maximal decongestion. A 0° rigid nasendoscope is used with a lens-cleaning sheath (Endo-Scrub 2 - Medtronic, United States).
Step 2 – Uncinectomy and middle meatal antrostomy
We begin by performing a retrograde uncinectomy. A wide middle meatal antrostomy is fashioned, bringing the anterior limit forward to the lacrimal sac without breaching it. The inferior aspect of the antrostomy is the superior part of the inferior turbinate. This ensures a clear view of the orbital floor and infraorbital nerve, whilst reducing the risk of orbital fat obstructing the antrostomy following decompression.
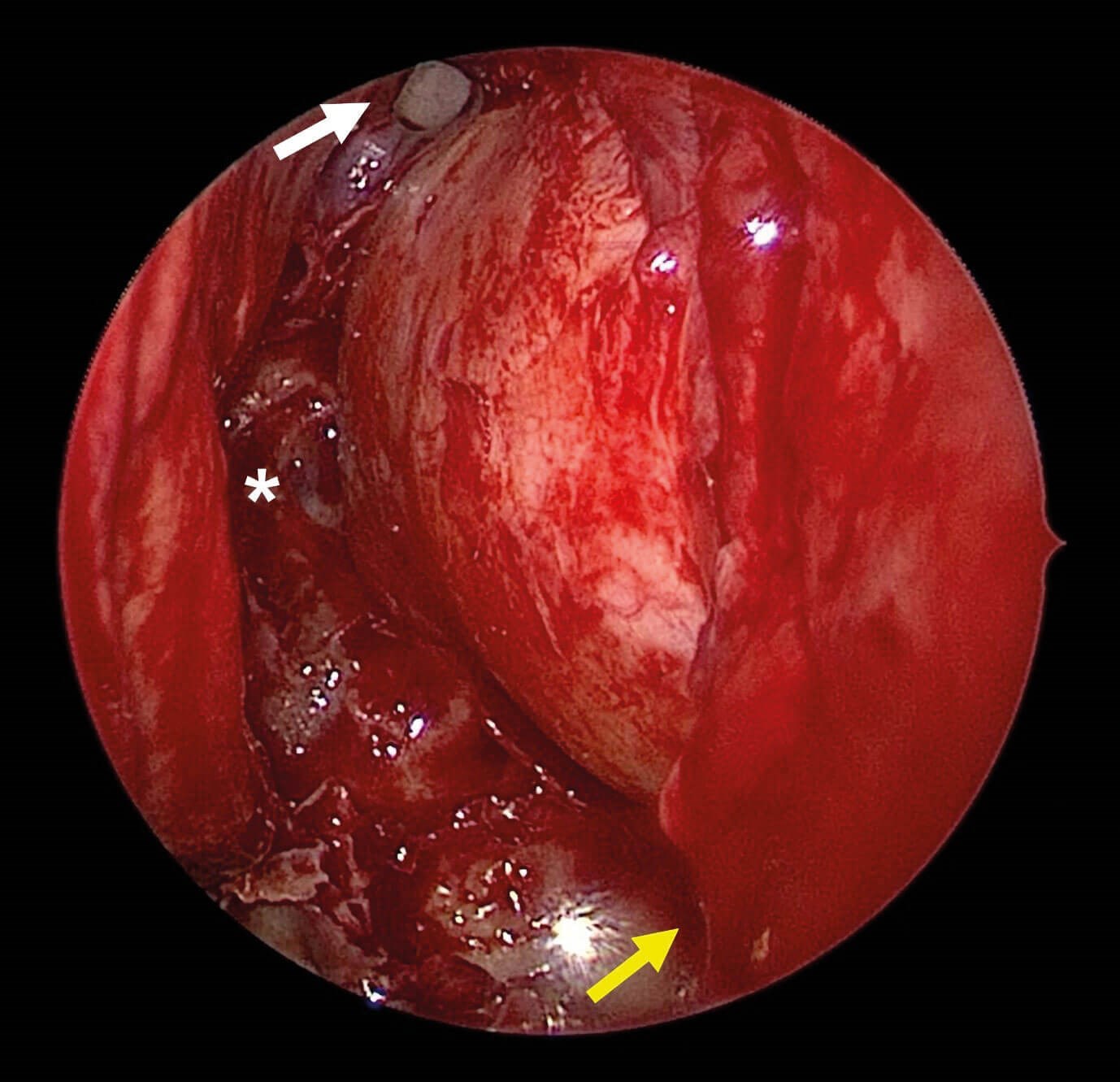
Figure 1. Endoscopic view of the left nasal cavity following anterior and posterior ethmoidectomy.
The lamina papyracea has been removed, revealing the bulging periorbita. Asterisk = face of sphenoid.
White arrow = frontal recess. Yellow arrow = maxillary sinus with excised orbital floor superiorly.
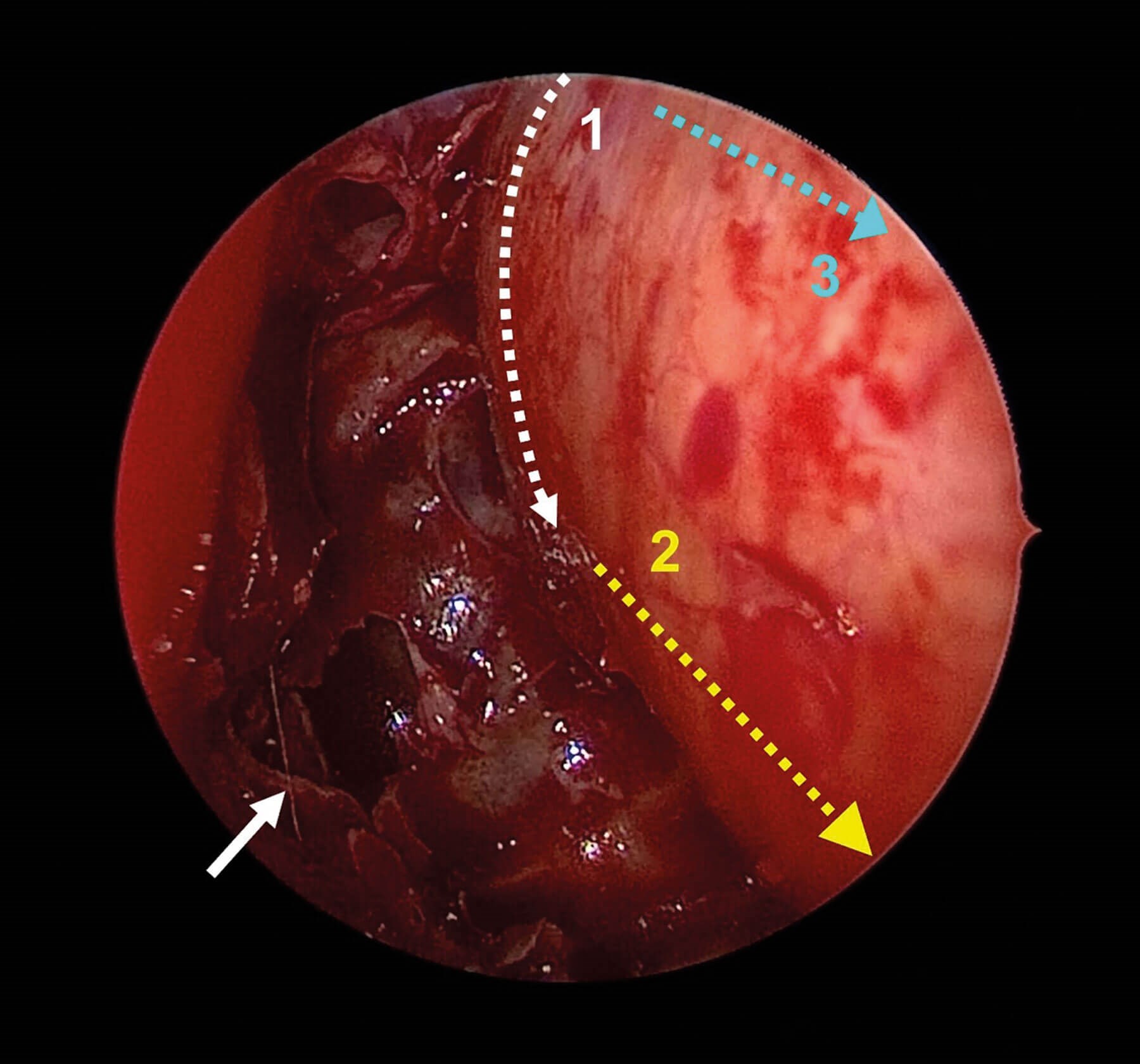
Figure 2. Demonstration of periorbita incisions. 1 = vertical incision using phaco knife.
2 = inferior incision using sickle knife. 3 = superior incision using sickle knife. White arrow = sphenoid ostium.

Figure 3. Pre and postop CT images of a patient with severe Grave’s ophthalmopathy. The postoperative CT neck performed prior to thyroidectomy demonstrates the right sided ‘two wall’ decompression and resulting prolapse of periorbital fat into the nasal cavity. A = preop axial slice showing severe exophthalmos with the entire globe anterior to the orbital rim. B = postop axial slice showing prolapse of orbital contents into nasal cavity and reduction in exophthalmos.
Step 3 – sphenoidotomy and ethmoidectomy
Following a standard anterior ethmoidectomy, the sphenoid ostium is identified and widened to expose the skull base and then the lateral wall. This step helps to define the anterior face of the sphenoid which will form the posterior limit for our decompression. The posterior ethmoid cells are then excised in a posterior to anterior fashion until the frontal recess is reached. The lamina papyracea is carefully identified and exposed along its whole length. At this stage we use the navigation system to confirm ‘two wall’ exposure of the orbit. The middle turbinate is medialised and sutured to the septum using 3-0 Vicryl, creating more space for herniation of orbital fat into the nasal cavity.
Step 4 – excision of lamina and orbital floor
A Freer’s elevator is then used to develop a plane between the lamina papyracea and the periorbita. Blakesley’s forceps are used to carefully remove fragments of the lamina, fully exposing the periorbita of the medial orbit. The bone of the orbital floor is thicker, therefore a Kerisson’s punch and a drill with a cutting burr (Straightshot M4 Microdebrider® - Medtronic) are used for the infero-lateral dissection. If there is no preoperative diplopia, a strut of bone is left between the medial and inferior walls to minimise the risk of postoperative diplopia. In severe cases with marked diplopia, this strut is removed to achieve a full decompression. The navigation system is once again used to confirm the position of the infraorbital nerve, as this constitutes the inferolateral limit of the decompression.
Step 5 – incision of periorbita
A phaco slit knife is used to make a vertical cut at the posterior limit of the periorbita. The orbital apex is just lateral at this point, so great care must be taken to avoid damaging the medial rectus muscle and optic nerve through an overly deep incision. Once the tip of the blade is through the periorbita, the cut is performed from lateral to medial to reduce the risk of injury to these structures. A sickle knife is then used to make posterior-to-anterior cuts inferiorly and then superiorly, at which point the orbital fat will begin to prolapse into the nasal cavity. This sequence prevents prolapsing fat from obscuring the surgeon’s view. A ball-point probe is used to release any remaining bands of fibrous tissue anchoring the periorbita to the orbital fat. The periorbita is removed as infero-laterally as possible to ensure a full release through the orbital floor into the maxillary sinus.
Step 6 – haemostasis and packing
Haemostasis is confirmed after the anaesthetist has returned the patient to a normotensive state. The postnasal space is suctioned and a Posisep® Haemostat (Haemostasis, LLC, United States) nasal pack is inserted if bleeding has been problematic.
Step 7 – postoperative care
The patient is advised not to blow their nose for two weeks postoperatively, thus avoiding a pneumo-orbit. Two weeks of saline nasal douching is prescribed to reduce crusting. The patient is reviewed in clinic following this for suction and debridement of crusts as needed.
Key points
- A wide antrostomy facilitates access and reduces postoperative maxillary sinus outflow obstruction.
- The anterior face of the sphenoid is a key landmark for defining the posterior limit of dissection and should therefore be fully exposed.
- Intraoperative navigation systems are a useful adjunct for safely defining the limits of the decompression.
- To avoid obscuring the operative field with periorbital fat, the periorbita should be incised in the following order:
- Posterior vertical incision (phaco slit knife)
- Inferior posterior-anterior incision (sickle knife)
- Superior posterior-anterior incision (sickle knife)
Further reading
1. Ting JY, Sindwani R. Endoscopic orbital decompression. Oper Tech Otolayngol Head Neck Surg 2014;25:213-7.
2. Shepard KG, Levin PS, Terris DJ. Balanced orbital decompression for Grave’s ophthalmopathy. The Laryngoscope 2009;108(11):1648-53.






