The impact of COVID-19 has been felt on all levels of society and deeply affected our lives. It has challenged us to find new ways of carrying on with our activities at home, work, and school. Jeff Small, Director and Associate Professor, and Navid Shanaz, Associate Professor, School of Audiology and Speech Sciences, University of British Columbia, tell us about the impact of the pandemic at the school and the innovative ways faculty found to teach audiology and speech sciences (hint, it was much more than Zoom!)
Jeff Small
Thank you for taking the time to talk to me today, Jeff. Could you please give us an idea of the impact of COVID-19 in the School of Audiology and Speech Sciences?
 Needless to say, the impact has been profound, whether it be on clinical training, academic course work, research, or administrative operations. Early in March, we started hearing about the possibility of having to curtail in-person clinical, academic and research activities. Then on a weekend in mid-March we received the notification that we were supposed to transition courses to online instruction the following week. Although many of our instructors had some familiarity using UBC’s learning management system, called Canvas, for routine course administrative tasks (e.g. posting syllabus, readings, assignments) there was a lot for our instructors to learn in delivering a course in its entirety online, from how to record and post lectures to how to conduct breakout group discussions online.
Needless to say, the impact has been profound, whether it be on clinical training, academic course work, research, or administrative operations. Early in March, we started hearing about the possibility of having to curtail in-person clinical, academic and research activities. Then on a weekend in mid-March we received the notification that we were supposed to transition courses to online instruction the following week. Although many of our instructors had some familiarity using UBC’s learning management system, called Canvas, for routine course administrative tasks (e.g. posting syllabus, readings, assignments) there was a lot for our instructors to learn in delivering a course in its entirety online, from how to record and post lectures to how to conduct breakout group discussions online.
It was certainly turbulent for the students as well, having to shift things from the way they were used to doing to the online context, such as no more face-to-face peer learning activities and managing all components of assignments and exams online. I believe just being able to finish the term was an achievement for both instructors and students! While most of our courses were able to be fully completed by the end of the term, there were some that had a lab component involving hands-on activities that had to be deferred until later when onsite gatherings would be permitted again.
An important part of dealing with the COVID-19 pandemic has been the psychosocial aspect, for faculty, staff, and students, of adjusting to a virtual work and learning context. The novelty was there for the first few weeks, but after that, it started to get old really fast. Having breakout groups and meetings virtually does not provide the same feel and connection to one another. While we are being asked to look after our mental wellbeing, at the end of the day we are also being asked to provide the same high-quality education and research experiences for students, which can be challenging.
Remote working and learning, and the dependence on technology, also presents challenges. Not everyone has a private, dedicated space to work from, free from distractions. Some of our faculty, staff, and students have children or have to share their space with a partner. Those are aspects that create stress for the remote worker/learner and are not easy to provide a solution for. Hopefully with the beginning of this next stage of our BC reopening plan, the university may grant permission for some individuals to use private work and learning spaces at UBC.
How was it for students to finish their clinical placements and graduate in 2020?
Second-year Audiology students usually finish their last placement in the spring, in time for graduation. Thankfully, we were able to gather in all the hours they required to graduate. For our Speech and Language Pathology second-year students it was not so easy, and our clinical coordinators team had to be creative and resourceful in coming up with a programme of supervised clinical simulation using the software Simucase. For students who need or want additional clinical training hours, we have been able to line up externships in July and August.
Our clinical educators have been fantastic in being supportive of our students as they only recently returned to their reopened clinics. We are also very fortunate to have identified clinical placements for the first year Audiology students, who normally complete two clinical externships during summer, before the fall of second year. The first-year Audiology students also used a software simulation to prepare for their externships. Navid Shanaz will tell you more about that. But for both Audiology and SLP students going into second year, there will be some ground to make up in completing externships alongside their classroom work in the fall.
We are basically doing a reorganisation of the curriculum. The School’s Leadership Planning Committee (consisting of Director, Program Director, Clinical Coordinating Team Lead, Graduate Advisor, Curriculum Committee Chair, and Audiology Faculty member) were instrumental in finding ways to repackage clinical externships and academic coursework in a way that we hope will allow students to progress toward programme completion in 2021.
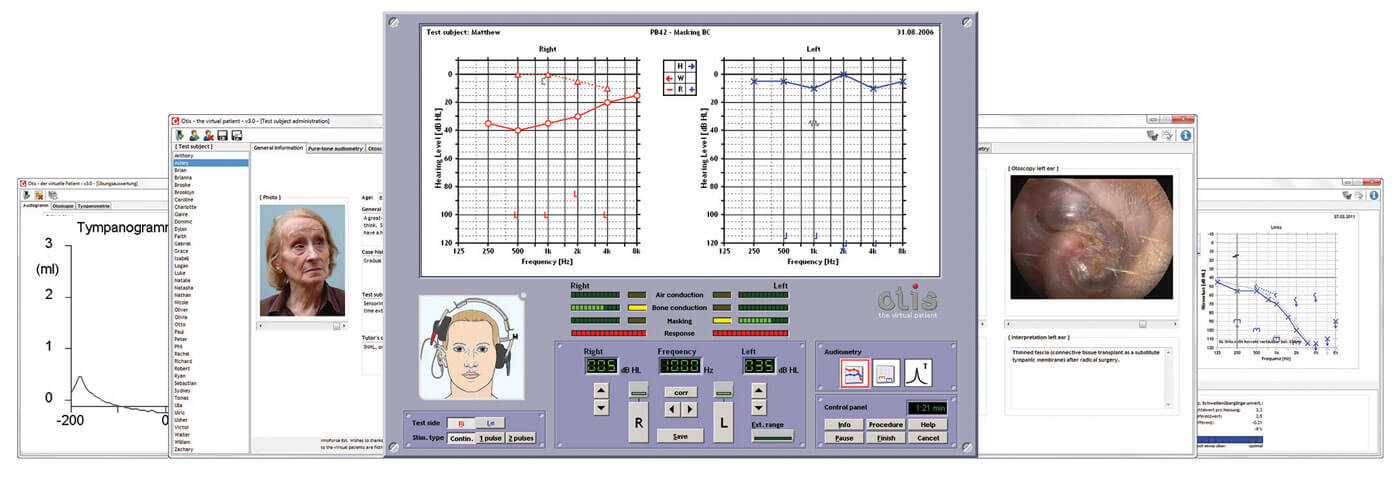
Otis – the virtual patient has been implemented at the School of Audiology and Speech Sciences
as an innovative solution for teaching the Audiology students during the COVID-19 pandemic.
The pandemic has brought all of us together and forced us to be creative and innovative as well. You mentioned Simucase, the case simulation tool used by the clinical instructors. How was the experience for instructors and students? Did the tool help provide the high-quality education the school is committed to?
That is a good question! Because the programme is just winding down for the SLP students, we are just now gathering information from them and from clinical instructors for a formal assessment. We will have the results in a few weeks. Anecdotally, it appears to have been well received by the clinical educators and students and described as a positive experience. Simulation is a tool that we plan to continue using in the foreseeable future.
Speaking of what is to come, how are the plans for the coming fall term?
It has been a busy time for our faculty. Faculty members usually have their summers off from teaching and administrative responsibilities to focus on research, which is half of their job. With research curtailment just recently being lifted in a phased-in approach, faculty have been dedicating their attention to teaching, performing COVID-related service, and/or preparing for online teaching in the fall. There are lots of sacrifices that have to be made to adapt to this new way of doing education and research!
Another group that needs to be acknowledged is our sessional instructors, invited to teach in the fall. We were concerned that those who had been teaching in the past might be reluctant because everything is being offered online, but the reaction has actually been the opposite. They have been enthusiastic and supportive. This new way of teaching will be challenging but achievable, and we are profoundly grateful for the support of sessional instructors and clinical educators.
“We were concerned that those who had been teaching in the past might be reluctant because everything is being offered online, but the reaction has actually been the opposite”
In preparing for the academic curriculum this coming year, we know that instructors will need support for converting their face-to-face courses to online delivery. In this regard, our curriculum Chair, Valter Ciocca, has been working with the Faculty of Medicine’s eHub team, and the Centre for Teaching, Learning and Technology, which provide workshops and resources for instructors, from designing all the way to implementing online courses. The eHub team will also provide tech rovers that will help instructors solve tech challenges as they set up and deliver their courses. Even with these supports in place, we are aware that it is a big ask of our instructors to convert their courses to an online format.
Another challenge for the fall is the requirements around physical distancing and PPE. The university is only allowing students to come to campus for hands-on activities that are absolutely required in their courses. These activities will take place following restrictive physical distancing and PPE guidelines. We will have to increase the number of labs to accommodate the restricted maximum number of people allowed in the lab spaces and will require additional instructors and teaching assistants. However, our faculty is assuming a positive can-do attitude and working hard to plan these activities based on the continued improvement of pandemic conditions here in BC.
Navid Shahnaz
Thank you for taking the time to take my call, Navid. I spoke with Jeff today about the impact that COVID-19 has had at the School of Audiology and Speech Sciences. I heard that you have implemented an innovative solution for the Audiology students – a simulation software. I am very curious to hear about it, please!
 I teach Diagnostic Audiology I and within that course, students go to Worksafe BC for a training day to perform all diagnostic testing they have learned in the course, such as otoscopy, tympanometry, audiogram, speech testing, masking. It is their chance to practise before heading out to their first round of placements in the summer and encountering patients. It is a sort of a badge for them before they start their practicum. When the course was moved to online platforms and clinics were closed in March, I had to come up with a plan to cover that specific clinical training day. I searched for available online simulation tools and came across this software from Liechtenstein, which I had seen in the past: ‘Otis – the virtual patient’. Upon close inspection of the software, I found out that it would in fact meet all the requirements for the training. The developers created a virtual patient simulation with a range of pre-programmed hearing deficits, in addition to the capability for the instructor to create their own cases.
I teach Diagnostic Audiology I and within that course, students go to Worksafe BC for a training day to perform all diagnostic testing they have learned in the course, such as otoscopy, tympanometry, audiogram, speech testing, masking. It is their chance to practise before heading out to their first round of placements in the summer and encountering patients. It is a sort of a badge for them before they start their practicum. When the course was moved to online platforms and clinics were closed in March, I had to come up with a plan to cover that specific clinical training day. I searched for available online simulation tools and came across this software from Liechtenstein, which I had seen in the past: ‘Otis – the virtual patient’. Upon close inspection of the software, I found out that it would in fact meet all the requirements for the training. The developers created a virtual patient simulation with a range of pre-programmed hearing deficits, in addition to the capability for the instructor to create their own cases.
“The developers created a virtual patient simulation with a range of pre-programmed hearing deficits, in addition to the capability for the instructor to create their own cases”
The software uses artificial intelligence and simulates the behaviours of a patient and also detects potential errors that a student would encounter. The student can practise all tasks they would in a real testing situation: perform otoscopy, insert the earphones, estimate hearing thresholds, apply masking as needed, perform UCL (uncomfortable loudness levels). All the while, the software is recording student’s action and timing them. This information is sent back to me as their instructor. I can evaluate the accuracy of the estimated thresholds, of masking levels, and assess the student’s conclusions and reporting of findings. Based on this, I provide students with my feedback.
I am amazed, this is really interesting! How is the interface for the student and what are the requirements of the simulator?
The school was very generous and purchased the software license within very short notice. My understanding is that price was high but reasonable. The software runs on Windows but can also run on a Mac computer with a Windows emulator. The problem that I encountered most often was with older Mac computers that did not run Windows smoothly. For some of the students, I had to come up with a remote access to a computer running Windows so they could complete their practice sessions. In the end, all students were able to successfully complete their training.
The simulator obviously does not provide the same feel and experience of a real patient, but it is a very close and realistic simulation of a patient. I have to say that the students greatly contributed to the success of this experience. They were open to it and enthusiastic about engaging in this new way of teaching/learning. None of this would have been possible if wasn’t for their willingness to participate in this collaborative effort.






