As we celebrate the cochlear implant, we celebrate an amazing work of innovative biomedical engineering that is a life-changer to many recipients around the world. We take for granted the arduous journey of the cochlear implant since its conception. Eric Levi speaks to Professor Graeme Clark, the surgeon scientist who made the multi-channel cochlear implant a reality and takes a peek at the journey of innovation and sacrifices.

Graeme Clark is a co-recipient of the prestigious 2013 Lasker~DeBakey Clinical Medical Research.
Photo taken in his office at The University of Melbourne.
Professor Clark, thank you kindly for your time. What role is held dear to your heart?
Thank you. For me, giving speech understanding to severely-to-profoundly deaf adults and spoken language to deaf children has been the fulfillment of a dream to help deaf people.
How did this journey begin?
As a five-year-old in Sydney, Australia, when asked by my kindergarten teacher what I wanted to do when I grew up, I said: “I want to fix ears”. The reason was I was learning what life was like for my father - a pharmacist, who was severely deaf - and how difficult it was for my mother on social occasions. At 10 years of age when I read the Life of Louis Pasteur by Rene Vallery-Radot, I became inspired by the beauty and simplicity of his experiments and this lit ‘a fire in the belly’ that I too could make discoveries in the biomedical area. So, I also commenced doing experiments in my mother’s laundry room, including studying the diseases affecting the tomatoes in my garden.
What was your path to research and innovation?
At 17 years of age in 1952, I arrived at the University of Sydney, thrilled to be studying medicine. Many years later, I completed my ENT surgical training in Australia and the UK. Then I returned to Australia by ships.
Arriving in Melbourne, I became a partner in an ENT/allergy group where I earned our family’s income doing all the surgery for the practice. But at the same time, to gain experience and professional acceptance, I did honorary public hospital sessions. Although I enjoyed all the surgery I was doing, I longed to be able to do auditory neurophysiological studies. While resting between cases in the park in 1966, I read an article by US surgeon, Blair Simmons, on results from electrical stimulation of the auditory nerve on one of his deaf patients. This ‘fanned the fire’ to do innovative research that had been smouldering inside me. His was the first good scientific study I had read, but Blair could not achieve speech understanding. However, it made me think that if I was to achieve speech understanding for severely deaf people, it would require even more careful and appropriate scientific studies.
“I commenced doing experiments in my mother’s laundry room, including studying the diseases affecting the tomatoes in my garden.”
To develop a truly scientific approach to the problem, I decided to leave my specialist practice in Melbourne and pursue a PhD degree in Sydney. It meant a large sacrifice in salary, especially having to bring my growing young family from Melbourne back to Sydney. The scientific climate at the time was: “Direct stimulation of the auditory nerve fibres with resultant perception of speech is not feasible.” – Physiologist, Merle Lawrence (1964); and “Direct stimulation of the cochlear nerve will from time to time be discovered. There is no indication that it will ever succeed in enabling a patient readily hear speech.” - Audiologist, Ed Fowler (1968). This was challenging, but my own initial PhD neurophysiological research in 1969 concluded that: “meaningful speech may still be perceived if it can be analysed into its important components and these used for electrical stimulation. More work is required to decide which signals are of greatest importance in speech perception.” – Clark, 1969. I reasoned this would require multi-channel stimulation with the place coding of frequency.
That’s a significant conclusion. What did you do after that?
Having reached a crucial point in the electrophysiological treatment of severe deafness, it was disheartening to realise there was nowhere to go to make the next important discoveries. If it had not been for the fact that the University of Melbourne had just created the first chair in otolaryngology in Australasia, there would have been no possibilities to continue my work. I am therefore very grateful to the University of Melbourne for appointing me to the foundation Chair in Otolaryngology. Although my research was potentially groundbreaking, it was a very high risk, and I was the youngest clinical professor at the university.
“Many thought I was sending out the message that we hoped to achieve super hearing, which of course was not the case.”
In accepting the Chair in Otolaryngology, I had to take on many responsibilities, and that afforded me little time to further my auditory electrophysiological research for severe deafness, and I had virtually no money. I tried, whenever possible, to continue my research, raise funds for this research, and personally inspire young graduates in medicine, engineering and science to join with me in pursuing this goal.
Were there other challenges you had to overcome?
My basic studies showed why a single-channel implant was limited, and that multi-channel stimulation would be required for speech understanding. But just how to represent the complex patterns of speech with multi-channel stimulation could not be well understood on the experimental animal, and had to be carried out on humans, as we are the only species with well-developed speech. This meant I had to ethically manage my patients not only to gain essential research information, but to do it in such a way that they also received the help needed to communicate in an auditory-verbal environment as soon as possible. To evaluate speech coding strategies with a prototype multi-channel implant was going to cost some hundreds of thousands of dollars. I did not have that sort of money. Nevertheless, I believed if I persisted in receiving small donations from service clubs for after-dinner talks, I would at least have $15,000 to purchase a computer with 8KB of random access memory to start the research. I was not prepared to do experimental surgery on patients without carrying out every study possible to maximise safety and success.
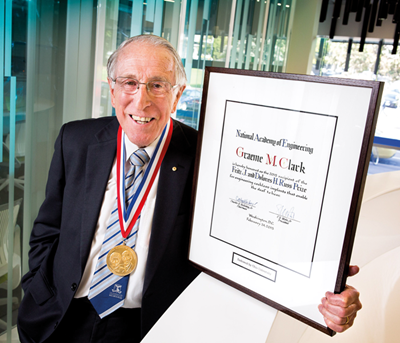
Australia’s bionic ear pioneer and Academy Fellow, Laureate Professor Emeritus
Graeme Clark, is a joint recipient of the prestigious 2015 Russ Prize.
Photo taken in the Centre for Neural Engineering at The University of Melbourne.
Was fundraising and community acceptance for your work difficult?
I had to consider fundraising from the community to take our work further. A TV station was very generous with its support and ran telethons. At one of our meetings in 1974 we needed to have a name that would resonate with the public and capture the essence of our research. At the time The Six Million Dollar Man, starring Lee Majors, was showing, and his injuries were being repaired with bionic limbs. That gave us the idea to identify our telethons as raising funds for nerve deafness, and in particular a bionic ear. To my knowledge, that was the first time the term was used for a medical application combining medicine and engineering. I was strongly criticised the first time I included it as a title for a conference presentation. Many thought I was sending out the message that we hoped to achieve super hearing, which of course was not the case. Since that time, it has become a well-used and respected term.
What about the first implantation?
After many years and many scientific studies, I was finally ready to do the first operation on 1 August 1978. There was an air of expectancy around the hospital and certainly in the operating theatre. A colleague stood outside my operating theatre and said: “Professor Clark, your moment of truth has arrived”. One thing I learned from this surgery is that it is not a great idea to do something that is breaking new ground for the first time with media attention. It is stressful enough to be doing the procedure, but if you fail the whole world will know. Fortunately, that did not occur, and the press soon became very interested in the work.
You must have been very relieved. How significant was this to your work?
When I started research to give hearing to profoundly deaf people with electrical stimulation of the auditory nerve, I said I would not stop until I had achieved normal hearing for most people. It was, of course, an idealistic goal but that was the way I viewed this challenge. Having shown that the University of Melbourne / Cochlear monaural multi-channel implant could provide speech understanding with and without lip reading, I was keen to see improved benefits in noise and everyday communication, by providing binaural hearing. For this reason, I carried out the first bilateral multi-channel implant in 1989. Again, that was shown to be beneficial.
“It is not a great idea to do something that is breaking new ground for the first time with media attention. It is stressful enough to be doing the procedure, but if you fail the whole world will know.”
However, my greatest passion, one that had driven me through many years of struggle, was the desire to give hearing, especially speech perception and spoken language, to deaf children. I planned for the research on children when the programme to help adults deafened later in life was well under way. The encouraging results from Melbourne in 1985 to 1986 led to a world trial for the US FDA which was approved on June 27, 1990. The approval by the FDA was the culmination of all my dreams and hopes for deaf children. This was independent and objective confirmation. It helped to establish the multi-channel cochlear implant as the first major innovation helping deaf children to communicate in over 200 years since Sign Language of the Deaf was used at the Paris Deaf School by Abbe l’Epee.
What can we learn from your journey of innovation?
The multi-channel cochlear implant illustrates the success of bionics for engineering devices that model brain mechanisms. I worked with various scientists, electronics, medical engineers and software engineers who made the bionic ear a reality. Advances in electronics, nanotechnology, micromechanics, polymer chemistry, and molecular biology should lead to cochlear implants that give high-fidelity sound. The research is the basis for a new discipline that I have called medical bionics, which should also contribute to spinal cord repair and the relief of blindness.
Interviewed by Eric Levi.