After more than four decades of paediatric clinical practice, Trevor McGill shares his wealth of experience and knowledge with Pat Bradley.
Trevor, as a national and internationally acknowledged Paediatric Oto-Rhino-Laryngologist, Head and Neck Surgeon, to what do you owe this achievement?
I have been a full-time otolaryngologist at Boston Children’s Hospital since 1976. Over the past four decades, Dr Gerald Healy and I established the ENT department as one of the premier units in the USA. In doing so, I developed a special expertise in caring for patients with complex otological disease, head and neck tumours, congenital anomalies and lesions of the paediatric airway. My special expertise is the care of children with head and neck tumours, hemangiomas and vascular malformations. In the 1980s we reintroduced surgery as the treatment of choice for paediatric head and neck sarcomas, resulting in altering clinical care.
I altered the understanding of middle ear congenital cholesteatoma. Two distinct temporal bone histopathological types were described:
- a closed keratotic cyst in the anterior mesotympanum and
- an open infiltrated type of which there is no containment of keratotic debris and the cholesteatoma makes direct contact with the middle ear mucosa. Surgical eradication of the open type is difficult and failure is associated with residual disease whereas in the closed keratotic cyst type is easily removed.
Fulminant aspergillosis of the nose and paranasal sinuses as a unique new clinical entity was first described in 1980 by our centre. This severe form of aspergillosis occurs primarily in individuals with compromised immunological responses. Control of this disease requires surgery, systemic anti-fungal therapy and correction of the immunological deficit.
Dr Geza Yako [1] and others developed a micromanipulator to couple the carbon dioxide laser to the operating microscope. When surgical laser became available, Drs Strong [2], Vaughn and Healy published an article in 1976 outlining their clinical experience in treating 110 patients with recurrent respiratory papillomatosis. Dr Healy, and I, advocated laser in the surgical management of subglottic hemangioma; however, propranolol is now the treatment of choice.
The value of my contributions is evidenced by repeated invitations to talk on various aspects of paediatric otolaryngology at national and international meetings. To date, I have been co-editor of three paediatric otolaryngology textbooks: the most recent being, Paediatric Otolaryngology: Principles and Pathway [3], now in its second edition.
As an ‘Irishman abroad’ for decades you must have suffered from the ‘must-go-home-syndrome’! How did you respond?
Following my training in the UK, I would have liked to return to Ireland, but there were no consultant positions available in paediatric otolaryngology. I am in constant touch with my family in Ireland and England, and I also keep in touch with with former ENT colleagues as I regularly attend ESPO (European Society of Paediatric Otorhinolaryngology) meetings.
Over the years I have delivered the William Wilde Discourse at the IOS (Irish Otolaryngological Society), the John Evans Lecture at the 2012 meeting of BAPO (British Association of Paediatric Otolaryngology) and have spoken on a number of occasions at the RSM (Royal Society of Medicine) in London.
I have maintained contact with my alma mater, UCD (University College Dublin, Medical School) by being President of University College Medical Graduate Association of North America,1996 - 1998. In 2001 I was the UCD Medical Alumnus of the year. A liaison has been established between Boston Children’s Hospital and the Irish Otolaryngology Training Program, whereby a specialist registrar rotates through our department for six months every year.
Having spent some early years in England, followed by a period as a research fellow in Boston, how did your desire to super-specialise in paediatrics come about?
I commenced my training in otolaryngology at the Royal National Throat, Nose and Ear Hospital in Golden Square, London, and Myrtle Street Hospital, Liverpool. Those four and a half years were some of the happiest times of my life. The last of my four years in Alder Hey Hospital under Mr Bob Pracy; thus, I had a significant experience in paediatric otolaryngology prior to coming to Boston.
This was followed by a two year Fellowship in Otology at the Massachusetts Eye and Ear Infirmary. The first year was focused on temporal bone histopathology and sensorineural hearing loss, and the second year was as a clinical Fellowship with Dr Harold Schuknecht and Dr Bill Montgomery.
In the spring of 1976, Dr Schuknecht asked me to consider a full time faculty position at Boston Children’s Hospital. I was interviewed by Dr Judah Folkman, (father of angiogenesis), the Surgeon-in-Chief at Boston Children’s Hospital. He took me on a tour of the hospital and asked immediately if I would like to start working. In response to my proposal for a start date in late July or in the autumn, he asked, “what about tonight”. That is how one got a consultant post in 1976. Serendipity!
Dr Stuart Strong [3] asked Dr Gerald Healy to come to Children’s Hospital to oversee the Boston University residents through their rotation in otolaryngology. Around the same time, Dr Schuknecht asked me to oversee the Harvard Medical School residents in his department. I arrived at Boston Children’s Hospital a few months before Dr Healy in the summer of 1976. The department at that time consisted of the two of us, two residents and half-time secretary, this staffing has now expanded to 16 surgeons, 4 fellows and 3 residents, with an ancillary staff of approximately 180 individuals.
Liverpool lads and lasses, 1970s. L to R: Gerry Leonard, Hugh Burns,
Anne Manning, Marie Burns, Trevor McGill, Kevin Manning, Kate Leonard,
Anne Tobin, Kieran Tobin. Front: Angela McGill.
Boston Children’s Hospital, Depart-ment of Otolaryngology has gained ‘premier status’ as one of the top five ranked USA hospitals for decades. How has this been achieved?
Boston Children’s Hospital is the nation’s largest paediatric medical centre and is the primary paediatric teaching facility affiliated with Harvard Medical School. The hospital opened in 1869, a little more than 20 years after the first public demonstration of ether anaesthesia in Boston. Housing over 350 beds, it serves not only the Children’s Hospital for Boston, but also the greater New England area, as well as many national and international patients. Boston Children’s Hospital is ranked ‘No 1’ by US News and World Report.
The research commitment of the hospital is represented by the John F Enders and the Karp family Research Laboratories, comprising the largest paediatric research facility in the world. Our department actively participates in this research effort, with an emphasis on cellular and molecular hearing research. The hospital is affiliated with the contiguous Dana Farber Cancer Institute, and with the Neonatal Departments of the Brigham and Women’s Hospital and Beth Israel Deaconess Medical Center.
When Gerry Healy and I arrived, we realised that all airway problems were managed by the Anaesthesia Department and all head and neck surgeries including tracheotomies were performed by the General Surgical Department. As we demonstrated our expertise in all aspects of otolaryngology, particularly endoscopy, we soon became the service of choice in dealing with all head and neck problems including the paediatric airway.
Over the past four decades, our department has grown to 16 physicians and 180 associated staff, who care for 60,000 children annually. During that time we have developed various specialty programmes designed for more complicated problems working in a multidisciplinary clinician fashion. Specialty programmes at the Boston Children’s Hospital include:
- Augmentative Communication
- Program for Balance andVestibular Research
- Centre for Airway Disorders (CAD)
- Centre for Head, Neck and Skull Base Surgery
- Cochlear Implant
- Deaf and Hard of Hearing
- Sinonasal Disorders
- Speech and Language Pathology
- Voice and Velopharyngeal
- Simulation Training Programme
- Node Assessment Programme (NAP)
- Sleep Apnoea and Sleep Surgery
Otolaryngologist-in-Chief, Dr Gerald Healy, began the Fellowship Program in 1978, and under our leadership, this programme grew to be one of the most respected in the USA. Since then we have trained in excess of 400 residents and 74 fellows, these include many of today’s leading experts in this specialty.
Dr Healy was elected President of the American College of Surgeons and began his presidency in the fall of 2007. On Dr Healy’s retirement in 2009, Dr Michael Cunningham became the Otolaryng-ologist-in-Chief. He has continued to enhance the clinical activities of the department with the addition of four new attendings and the development of the Balance and Vestibular Program all of which has significantly improved the academic output of the department.
My life has been changed by our association
“No one can deny that Trevor’s sense of humour and humanity are his most endearing traits. My life has been changeda by being associated with Trevor and I feel deeply grateful for his guidance, teaching and friendship.”
Professor Ellen M Friedman Professor in Otolaryngology and Pediatrics Baylor College of Medicine, Houston, Texas, USA
The consummate clinician and educator
“Trevor has such a kind, encouraging and quietly inspiring way about connecting with his peers. The field of paediatric otolaryngology has benefited from his commitment to patient care, education and leadership.”
Dana Mara Thompson, MD, MS, FACS Professor of Otolaryngology Ann & Robert H Lurie Children’s Hospital of Chicago, Chicago, USA
You were appointed Professor of Otology and Laryngology at Harvard Medical School. Can you explain how this award came about?
The promotion process at Harvard Medical School is rigorous and forever changing. One starts out as an Instructor and then moves up the ranks to Assistant Professor, Associate Professor and, hopefully, finally a full Professor. To achieve promotion to Professor, one must have a sustained national, and in many cases, international, reputation as a leader and an innovator in otolaryngology.
The endowed McGill Chair in our Department was created by Dr Michael Cunningham in 2010, to provide administrative support for the fellowship director. Currently Dr Reza Rahba is the recipient of this Chair. The Chair was created by a significant financial donation from our department which was matched by Boston Children’s Hospital.
Proud and honoured to be his colleague
“I personally feel his most outstanding contribution has been in clinical teaching and mentorship. I am both proud and honoured to be his colleague.”
Michael J Cunningham Present Otolaryngologist-in-Chief Boston Children’s Hospital Department of Otolaryngology and Communication Enhancement
During your early career did any person or group of people influence your professional destiny, resulting in your pursuing an academic career in paediatric otolaryngology?
It is true that parents are the first educators and it was my parents, Kathleen and Jack, who first taught me the value of education. Anything that I have subsequently achieved finds it origins in their inculcation of this value in someone who was never a model student.
Mr Phillip Stell, Head and Neck Surgeon at Myrtle Street Hospital, Liverpool, was the first surgeon who taught me how to study, how to think, how to analyse. He was an excellent surgeon, tireless in his pursuit of the optimal therapeutic management of his patients with head and neck cancer. He was a great inspiration. He published extensively both in the English and Dutch language. My first paper about laryngeal cancer and exposure to asbestos was published with him in the Lancet.
It was Mr Bob Pracy, Paediatric Otolaryngologist, at Alder Hey Children’s Hospital in Liverpool, who was responsible for my pursuing a career in paediatric otolaryngology. He had a wealth of experience in managing patients with complex paediatric airway problems. He was an excellent endoscopist and a father figure to me. He clearly wanted me to return to the UK following my fellowship at the Massachusetts Eye and Ear Infirmary and was rather disappointed that I did not take up that consultant post at Great Ormond Street Hospital in the late seventies.
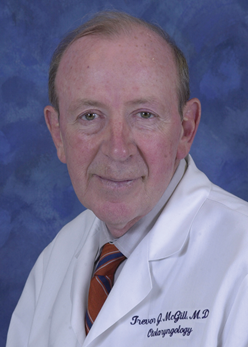
However, it was Gerry Healy, my colleague for 33 years and dear friend, who consummated my career in paediatric otolaryngology. Dr Healy is by any measure one of the most accomplished surgeons in the 150 year history of the Department of Otology and Laryngology at Harvard Medical School. Gerry served as President of ASPO (American Society of Pediatric Otolaryngology), ABEA (American Broncho-Esophagological Association), ALA (American Laryngological Association), the Triological Society, and ultimately President of the ACS (American College of Surgeons). It was from this leadership platform that he raised the profile of paediatric otolaryngology among adult colleagues and for this we will be forever grateful.
In 2008 Dr Healy was honoured by the Royal College of Surgeons of England and the Royal College of Surgeons of Ireland for his contributions in the area of surgical education and patient safety. In case you do not know, Dr Healy is Irish and very proud of it.
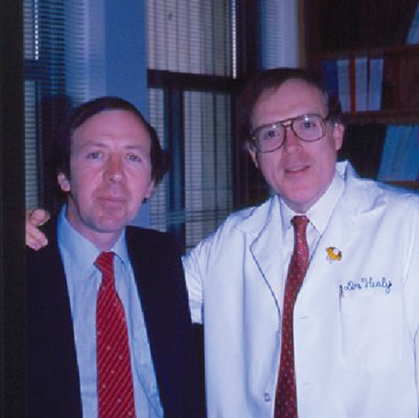
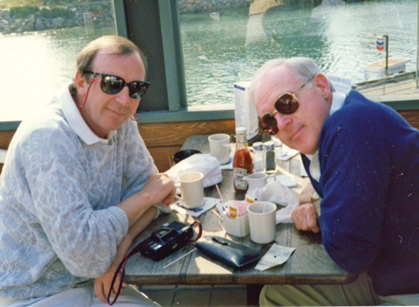
Trevor McGill and Gerry Healy – colleagues for 33 years.
His skills as a surgeon and his unique teaching style are legendary
“My admiration for him as a doctor, teacher and friend is boundless. His love of family and ability to tell great stories are in the finest tradition of his Irish culture.”
Gerald B Healy Emeritus Otolaryngologist-in-chief and Surgeon-in-chief Boston Children’s Hospital
Oh that we could clone him!
“In his quiet, yet highly effective way he opened up head and neck surgery for the next generations of pediatric otolaryngologists. He has always been the most pleasant of company and exudes the warmest of collegial friendship. Oh that we could clone him!”
Robert J Ruben, MD, FAAP, FACS Editor in Chief, International Journal of Paediatric Otolaryngology, New York
What in your opinion has been the greatest ‘invention’ / ‘change in practice’ in ORL-HNS during your professional medical life?
There have been two main areas where there has been significant change allowing us to improve our diagnosis and management of patients - head and neck diagnostic imaging and endoscopic techniques.
With advances in diagnostic imaging our pre-operative planning of resection of complex tumours of the neck, sinuses and skull base has been transformed. In tandem endoscopic sinus and skull base techniques allow us to access these areas safely without the morbidity. Likewise in the airway, nowadays it is a very rare event when we have to perform a laryngofissure to repair a laryngeal cleft, even a type III.
During your career, you have achieved many honours. What has driven (motivated) you to strive to achieve these recognitions?
One receives an Honorary MA from Harvard University on being appointed full Professor. Several senior otolaryngological societies in North America have honoured my contributions to paediatric otolaryngology, as their guest of honour including ASPO, ABEA, ALA, Triological Society. The Ainsworth Scholarship was awarded by the National University in Ireland, to allow me to travel to various centres in North America. The George Seed Memorial Prize was awarded by the North of England ENT Society in the early seventies. The Fogarty International Postdoctoral Fellowship Award awarded by the National Institute of Health in 1974-1976, funded my fellowship at the Massachusetts Eye and Ear Infirmary. In June 2011, University College Dublin awarded me an Honorary Degree of Doctor of Science. I was awarded the TG Wilson Medal at the ESPO 2014.
It has been rumoured that you are a friend of Vincent Browne, Irish journalist and broadcaster, and that the political magazine Magill has some association with that relationship?
Yes, Vincent and I are very good friends. My name was associated with the political magazine, Magill, of which he was editor, but I was not responsible for its eventual demise. He is one of a very tight cadre of University College Dublin graduates, not exclusively medical. We meet up, once a year over the past four decades, as a group of 10 people for a college reunion. Personally he is very engaging and great ‘craic’, however rather shy when meeting new people. He spent some time here in Boston and in fact, got married to his wife, Jean Learmond, from Delgany, County Wicklow, on Cape Cod, Massachusetts in the seventies. He has had a very interesting and successful career. He did forego opportunities to work for the Times and the Guardian in the UK to return to Ireland as an investigative journalist and TV host.
The Irish Otolaryngology ‘Mafia’ at Boston Children’s Hospital.
L to R: Paul Lennon (Resident from Irish Specialist Registrar Training Program),
Trevor McGill, Karen Watters (Otolaryngology Attending), Stephen Kieran (Otolaryngology Fellow).
Your family – wife, Angela, and son, Trevor Jr., I know have been a great source of comfort, solace, confidence during your long career. How have you fit in your home life with that of a ‘high-flyer academic’?
During my early days at Boston Children’s Hospital, Gerry and I, recognised that reorganising the Department of Otolaryngology was indeed a formidable project but, in the end, a very rewarding challenge. Encompassing family life, a new department and an academic career, may seem quite a task. We managed to keep in touch with our family and friends with summer family vacations to Europe, Christmas and school vacations travelling to Ireland, and our love of skiing, which all three of us clearly enjoyed. Life can be a balancing act and we seized our opportunities.
His clinical knowledge and experience are beyond accolade
“He is the rare individual who has found the ‘perfect’ balance between being a full-time academic clinician and a devoted family man.”
Karen Watters, MB BCh BAO, MPH Associate in Paediatric Otolaryngology Boston Children’s Hospital Associate Professor at Harvard
You and Gerry had and have a love for the outdoors and travelled widely seeking much ‘R&R’, including golf. Would you consider that golf be mandatory for ‘surgeons’?
We developed a relationship with the paediatric otolaryngologists at the Children’s Hospital of Philadelphia whereby we alternated a golf tournament with them for many years. Unfortunately the trophy resides in Philadelphia. We planned many different golfing trips to many countries with medical colleagues. Golf became a great source of ‘R&R’ and exercise. Having had a significant interest in the game, albeit a very humbling and frustrating game, but I would highly recommend it not only to surgeons, but to anyone who enjoys “a good walk spoiled”.
Have you any advice to give ORL-HNS trainees about how to succeed with gaining their credentials, and comment on behaviour when they achieve consultant status?
-
On being appointed consultant, an individual should establish a cordial relationship with his/her colleagues in other disciplines.
-
In managing difficult clinical cases, frequently ask advice from your more experienced colleagues.
-
One should develop a good working relationship with the hospital administration and maintain respect for each other.
-
When difficult problems are encountered, either clinical activities or administrative problems, communicate personally, rather than collectively via mass email as is commonly done nowadays.
-
Please be accommodating, always available and be very supportive of ancillary staff.
-
Continue to raise the profile of ENT with your colleagues in other disciplines.
-
Try and devote one day a week to academic activities, including teaching and clinical research.
-
Be humble but confident in dealing with patients. “Patients don’t care how much you know unless they know how much you care.”
GB Healy, 2008

Above right: Enjoying the fairways in the Carolinas – ‘A moment of frivolity’.
What plans have you for your impending retirement – whenever?
Or is that something for the future, to be confronted when it happens? I am over the last hurdle and into the final furlong of my medical odyssey. The possibility of a sabbatical looms in the air, and during that time, I would like to pursue some clinical research, write a history of the Department of Otolaryngology of Boston Children’s Hospital and visit colleagues in Ireland, the UK and Europe. Boston will always be my home because of our family and grandchildren, but I will spend some extended time both in Dublin and London.
References
1. Dr Geza Yako, a Hungarian Otolaryngologist who fought in the Hungarian Rising of 1956.
2. Dr Stuart Strong and I shared the same birthplace, Kells, Co Meath, Ireland.
3. Paediatric Otolaryngology: Principles and Pathway. Wetmore/Muntz/McGill. Publication date: January 2012, 2nd edition, 976 pp, hardback, ISBN (Americas):9781604064131.
Interviewed by Prof Patrick J Bradley.