A decade of innovation in digital, remote endoscopy is paving the way for ‘drop-in’ nasendoscopy, improving early head and neck cancer diagnosis in high-risk communities.
In May 2026, the University Hospitals North Midlands (UHNM) will inaugurate its newly established clinical diagnostic centre (CDC). These centrally funded extensions to secondary care provide in-demand diagnostic services at the centre of the community.

Figure 1: The CDC in Hanley.
The Hanley CDC in Stoke-on-Trent (Figure 1) will be situated at the heart of one of the most socially deprived regions of the United Kingdom, contributing to the rectification of healthcare inequality. Despite our efforts to raise awareness of head and neck cancer, we continue to observe late presentations to the head and neck service at advanced stages because the vague nature of head and neck symptomatology often leads patients to delay the inconvenience of a general practitioner consultation. Our objective is to overcome these referral barriers and provide an opportunity for patients residing in ‘high-risk’ regions to obtain a definitive diagnostic reassurance regarding their symptoms. Most referred patients simply seek a timely determination of whether they have throat cancer or not.
To diagnose cancer, we require visualisation. This can be achieved through radiology or endoscopy, both powerful diagnostic tools. However, traditionally, these investigations have been confined to the secondary care setting, necessitating patients to overcome the primary care gatekeepers to access these once-restricted resources.
"Our objective is to overcome these referral barriers and provide an opportunity for patients residing in ‘high-risk’ regions to obtain a definitive diagnostic reassurance regarding their symptoms"
Over the years, significant advancements have been made in both imaging and endoscopic technology. It is evident that artificial intelligence (AI) will play a pivotal role in the future of radiology, particularly in interpreting pixel data related to tumour density. Endoscopy, however, presents a substantial challenge due to the multitude of variables involved, including a variety of endoscopic equipment capabilities, light sources, the performing endoscopists’ technique and differing image resolutions. For many years, ENT surgeons relied on fibreoptic endoscopes, which were subsequently enhanced with the introduction of digital chip camera heads. In the present day, integrated ‘chip tip’ technology has dominated the diagnostic ENT endoscopy field, providing exceptional images that can be combined with light-altering technologies such as chromoendoscopy and soon, hyperspectral imaging.
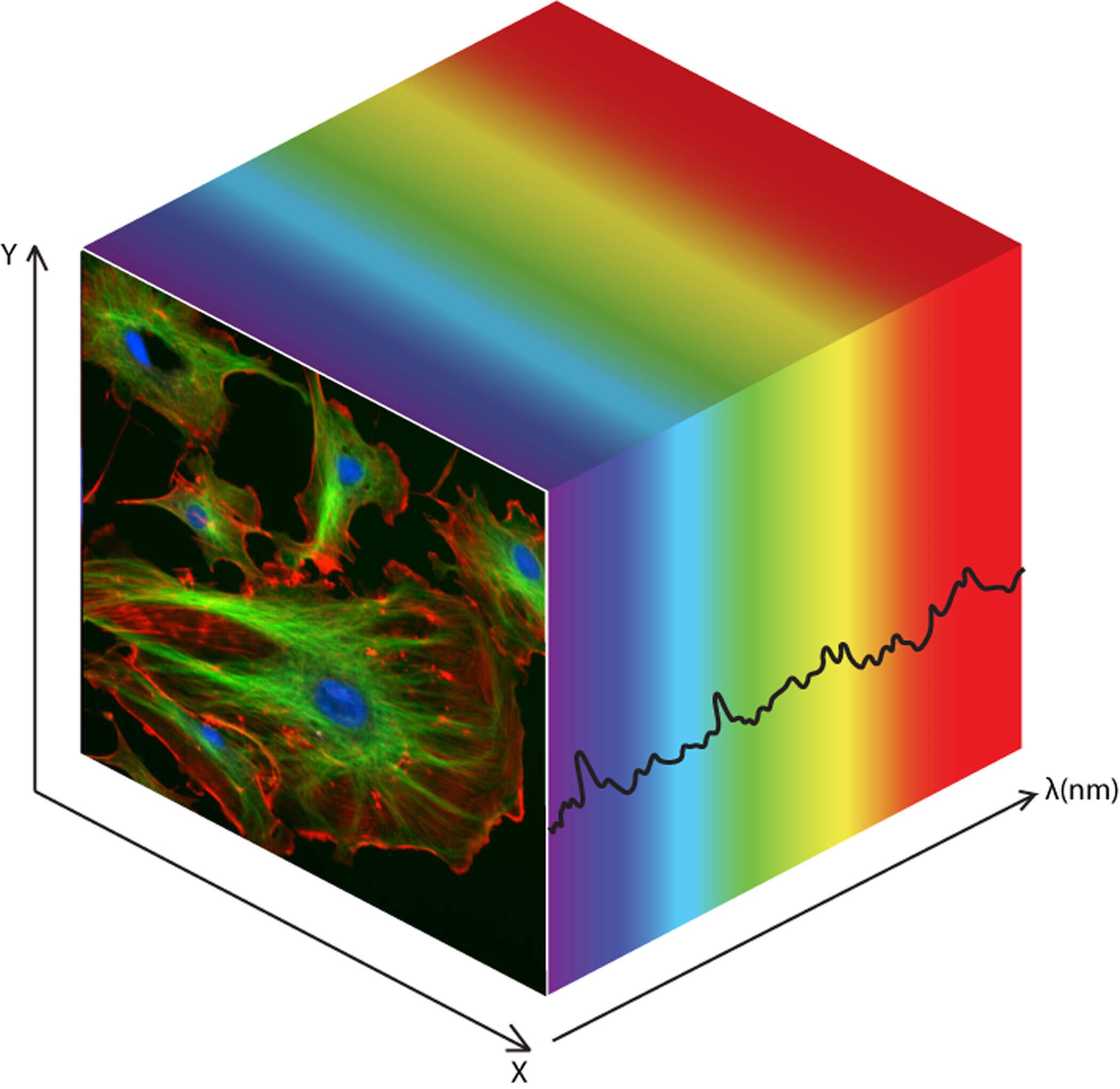
Figure 2: Hyperspectral images provide a 3D depth cube of light emitted by tissues.
To look at with the human eye, they make no sense. Courtesy of CleanPNG.
Traditional white light images may be eventually replaced by nonsensical light maps that represent invisible light emitted by normal and pathological cells (Figure 2). This concept may sound like science fiction, but our company, endoscope-i, has consistently envisioned endoscopy as the cornerstone of head and neck cancer diagnosis, potentially automated through machine learning. We are looking to build a platform that supports those changes for the future.
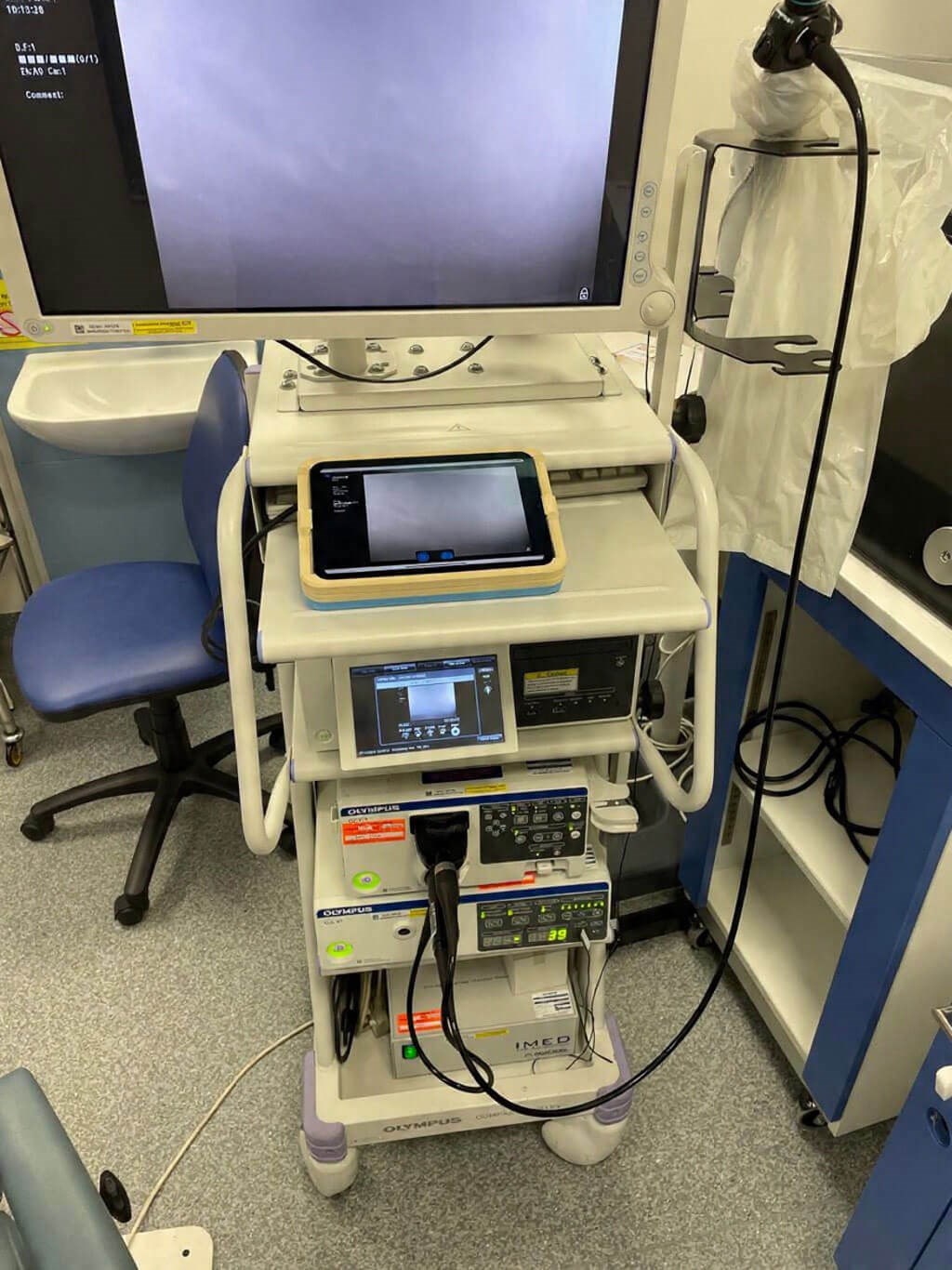
Figure 3a: Rapid Stack incorporated on a standard endoscopy stack.

Figure 3b: Rapid Stack capturing live endolaryngeal images.
To achieve this vision, we developed a novel concept that combines endoscopes with powerful mobile computers – what we recognise today as smartphones and tablets. The endoscopic-i ‘Rapid Stack’ (Figures 3a, b) can draw out the digital data from any commercially available endoscopy system, standardising image quality and acquisition and incorporating it into a digital file that can be encrypted through the cloud.
Over the past 12 years, engineers and clinicians within endoscope-i have dedicated themselves to overcoming significant challenges to establish a concept of telemedicine-endoscopy known as ‘telescopy’. This concept, when combined with a remote consultation, forms a ‘telescopic referral’. It captures the essence of any ENT consultation. A few carefully selected questions and a high-quality endoscopic image are combined into a digital format and collectively sent to a clinical expert for remote reporting. This model is widely recognised in the fields of dermatology and ophthalmology, and it has also been adopted in some remote regions of the world within ENT. However, within the National Health Service (NHS), ENT departments continue to operate on the traditional route, where all patients should be seen face to face. The primary challenges faced by the NHS include insufficient resources to accommodate over 250,000 urgent suspected cancer referrals annually, a static workforce that is increasingly experiencing burnout and the growing demands of a patient population that seeks not only verbal reassurance but also some form of diagnostic information.
Since the pandemic, head and neck cancer management has adopted a common triage approach in many UK institutions. ‘Low-risk’ patients constitute the majority of referrals, making them ideal candidates for a ‘telescopic referral’. In 2022, the NHS Cancer Programme, supported by the Small Business Research Initiative (SBRI), secured a £600,000 grant for endoscope-i Ltd to investigate how ‘telescopic referrals’ could not only maintain a high standard of care and safety in managing low-risk referrals on the cancer pathway but also do so in a significantly cost-effective manner. The benefit-cost ratio (BCR) was calculated at 0.7, indicating a return on investment from using the technology within five years. Consequently, UHNM has procured the ‘telescopic referral service’ for over five years. The enhanced capacity in endoscopy enables additional diagnostic slots for a crucial aspect that has always been important to me: a drop-in nasendoscopy clinic that eliminates the barriers of primary care. Patients from May 2026 will be able to ‘drop in’ to the new CDC in Hanley where they will receive a telescopic endoscopy to rule out concerns of head and neck cancer. The report will be provided by a consultant head and neck surgeon within 48 hours of the investigation and will be directly accessible on their NHS app in a digital format.
A lot of work and collaborative efforts between the industry and clinical governance at UHNM, for both clinical safety and cybersecurity, have been undertaken, as all digital data will be transmitted over the cloud. Consequently, all the digital endoscopic data collected will be utilised to develop a machine learning model that supports the automated diagnosis of head and neck cancer. This intellectual property (IP) sharing agreement has been reached between the UHNM and endoscope-i Ltd. The ‘telescopic referral’ pathway represents the first of its kind globally, with a robust evidence base. In the future, further innovative proposals, such as automated triage that could be achieved through the work of the Everest-HN study, would further enhance the telescopic pathway, providing even greater access to remote digital endoscopy. Currently, trained nurse endoscopists perform all nasendoscopy procedures. However, with the advent of flexible endoluminal robotics combined with machine learning, it is feasible to envisage a fully automated nasendoscopy service.
Further reading
1. GIRFT. Transforming Ear, Nose and Throat Outpatient Services: A practical guide to delivery. Page 13.
https://gettingitrightfirsttime.co.uk/wp-content/
uploads/2023/07/Transforming-ENT-Outpatient
-Services-FINAL-V2-June-2023.pdf
2. NHS Cancer Programme Innovation in the early detection and diagnosis of cancer. Page 33–4.
https://sbrihealthcare.co.uk/media/pages/
nhs-cancer-programme/impact/946942
ea8a-1696349139/cancer-booklet-compressed
_1-compressed-compressed.pdf.
3. Hardman JC, Tikka T, Paleri V, et al. Remote triage incorporating symptom-based risk stratification for suspected head and neck cancer referrals: A prospective population-based study. Cancer 2021;127(22):4177–89.
4. Metcalfe C, Oh S, Glazzard N, et al. A novel remote assessment pathway to streamline the management of two-week-wait suspected head and neck cancer referrals: a prospective analysis of 660 patients. J Laryngol Otol 2024;138(6):667–71.
5. George A, Tikka T, Conway D. Innovative Approaches to Head and Neck Cancer Diagnosis. Otolaryngol Clin North Am 2026;59(1):63–76.
6. Albutt A, Hardman J, McVey L, et al. Qualitative study exploring the design of a patient-reported symptom-based risk stratification system for suspected head and neck cancer referrals: protocol for work packages 1 and 2 within the EVEREST-HN programme. BMJ Open 2024;14(4):e081151.
[Links last accessed December 2025]
Declaration of competing interests: AG is the Medical Director for endoscope-i Ltd.








