Hyposalivation remains a stubbornly difficult condition to treat, but novel therapies may not be far away.
Saliva has many essential functions, including aiding digestion and swallowing, lubrication, maintaining tooth integrity and antibacterial activity. When patients experience reduced saliva production (hyposalivation), it can severely impact their quality of life. They commonly report difficulty swallowing food, speaking and xerostomia (subjective feeling of a dry mouth).
Anatomically, the salivary glands consist of three ‘major’ paired glands: the parotid, submandibular and sublingual glands that produce approximately 95% of total saliva. Hyposalivation occurs if there is either destruction of these cells or a lack of stimulation. The aetiology of this can be attributed mainly to medications, autoimmune conditions and radiotherapy for head and neck cancers [1]. Implicated medications are those with an anticholinergic mechanism of action such as antipsychotics and antispasmodics. Acetylcholine is the responsible neurotransmitter and binds to muscarinic receptors on the salivary cells, triggering salivation. Anticholinergic medications competitively inhibit the activation of these receptors. In Sjögren’s syndrome (SS), immune dysregulation drives lymphocytic invasion via the upregulation of genes such as human leukocyte antigen, leading to acinar cell damage. Damage inflicted by radiotherapy results from the inability to delineate well between a cancerous and normal cell and, as such, healthy acinar cells are destroyed when a patient is undergoing treatment.
A diagnosis of hyposalivation is largely clinical with a focused history and examination. Although there is no globally accepted diagnostic test, saliva output can be evaluated, termed sialometry. In this instance, salivary flow rate can be measured as either unstimulated (uSFR) or stimulated (sSFR). Typically, measurement of uSFR correlates better with patient symptoms, with a uSFR of <1.5ml in 15 minutes indicative of hyposalivation. The clinician should attempt to determine the root cause and assess the impact on the patient’s quality of life.
Current treatments
Management of hyposalivation is currently limited, with few effective interventions available. Patient education is key to ensuring the best possible symptom control. Patients should be advised to stay well hydrated, ensuring they have a frequent intake of water and reducing their intake of coffee/tea to prevent dehydration. Furthermore, they should be encouraged to adopt healthier lifestyle choices, such as cessation of smoking.
"The salivary glands lend themselves well to gene therapy due to characteristics such as ease of access via intraoral cannulation"
Pharmacological management should begin with the removal of the offending medication, should this be the cause, and the prescription of an alternative. Artificial saliva substitutes are another choice, such as those containing mucin or carboxymethylcellulose. However as these do not stimulate salivation, the effects are short-lived and therefore require repeated application.
Sialogogues are substances that stimulate the production of saliva and are currently the only alternative intervention to those mentioned previously. Chewing gum containing sorbitol or xylitol acts as a sialogogue but, once again, is short-acting. Systemic cholinergic medications such as pilocarpine and cevimeline are longer acting, however, cevimeline is not licensed in the United Kingdom. Pilocarpine is given orally and is initiated at 5mg three times per day but can be titrated up to a maximum of 30mg per day (in divided doses). However, it does take four to eight weeks to reach maximum therapeutic effect and should be discontinued if no effect is seen after three months. It is important to note that these medications require residual salivary gland function, are associated with side effects such as gastrointestinal upset and have variable efficacy.
Stem cells
Stem cells possess the capacity to transform into specific cell types and, among them, mesenchymal stem cells (MSCs) are of interest. These adult stem cells exhibit multipotency, enabling them to develop into various specialised cell lineages. This distinguishing feature, combined with their ability to be extracted from multiple tissues, be easily cultured in lab settings, and induce minimal immune responses (attributed to the absence of molecules like MHC II) designates them as promising contenders in the field of regenerative medicine.
Studies evaluating the efficacy of MSCs in stimulating saliva secretion in both animal and human subjects have been conducted. SS mouse models utilising bone marrow MSCs (BMMSCs) in mice showed both early and late-stage BMMSC-treated groups had increased SFR compared to untreated mice, but the effects were short-lived. Umbilical cord MSCs (UCMSCs) in human subjects reported conflicting statements about the presence of xerostomia symptoms [2].
"While MSC-based approaches show promise in improving salivary function, comprehensive, large‑scale studies are needed to establish their long-term effectiveness and broader applicability"
Adipose-derived MSCs (AdMSCs) have also been considered as an alternative to BMMSCs due to their higher densities and less invasive harvesting. Research has demonstrated improved SFR in a murine model with AdMSC treatment compared to controls. In human trials, AdMSCs injected into irradiated submandibular glands led to substantial increases in unstimulated whole SFR over one to four months [3]. However, the study’s limited sample size and lack of comprehensive variable analysis restrict generalisability.
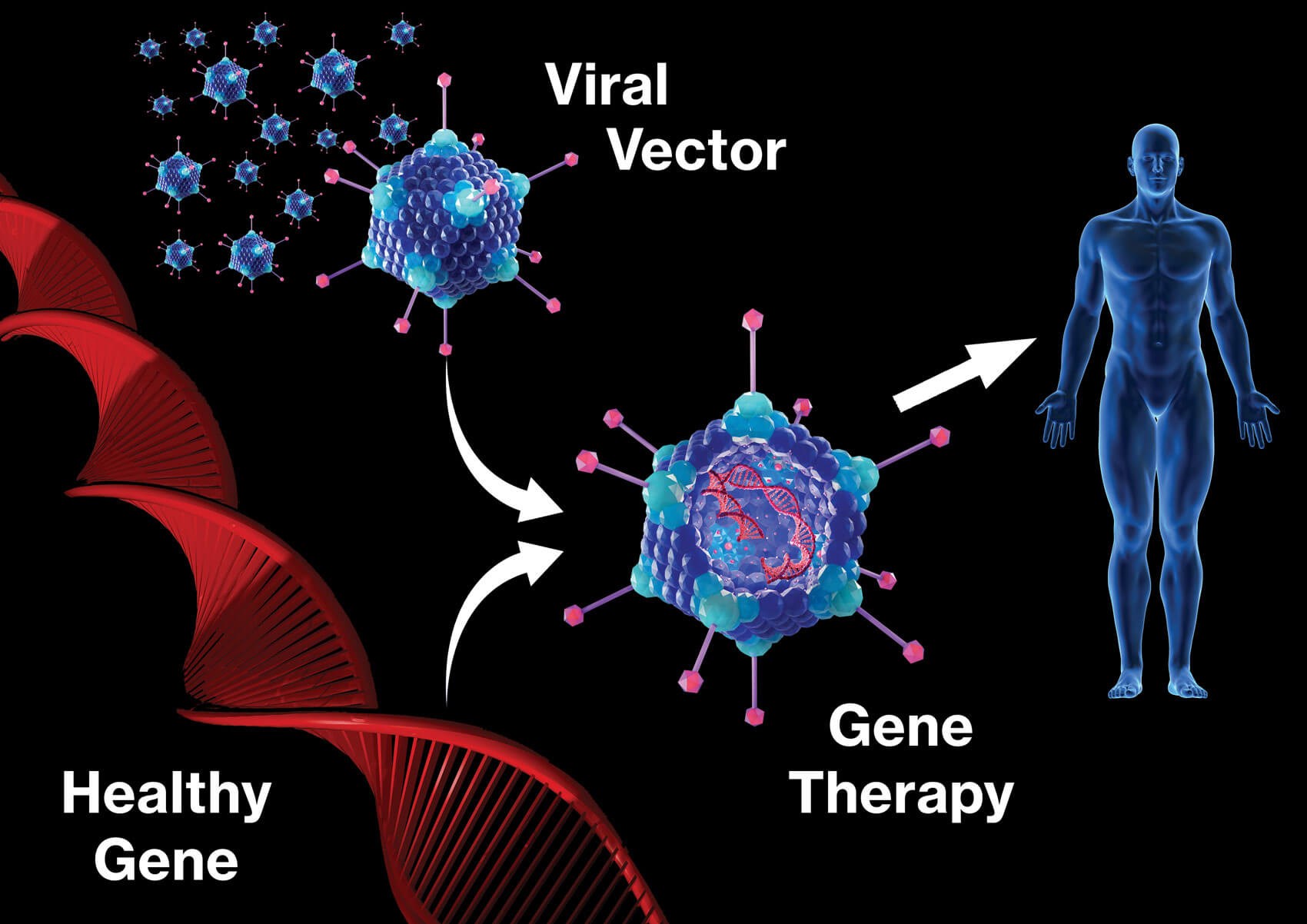
Figure 1: Gene therapy.
Gene therapy
Gene therapy is a technique whereby genetic material is transferred into cells to treat disease (Figure 1). The salivary glands lend themselves well to gene therapy due to characteristics such as ease of access via intraoral cannulation, and encapsulation of the gland reduces the chance of vector spread. Aquaporins (AQP) are transmembrane channel proteins that allow water across cell membranes, therefore facilitating saliva secretion.
AQP 1 has been evaluated in humans using adenoviral-mediated AQP 1 cDNA transfer. Results showed significant improvement in both absolute volume and proportional change in parotid flow rates following treatment. Although these results initially seemed promising, five subjects had no improvement, or worsening of their function on closer inspection [4]. Furthermore, the vector used does not deliver permanent gene transfer, so further evaluation will be required.
Aquaporins are not the only molecules responsible for salivary gland function, and other gene therapies have been studied. Unfortunately, transmembrane activator and CAML interactor (TACI) gene transfer have been ineffective in recovering salivary gland function thus far. However, success has been achieved by modulating the hedgehog pathway via the transfer of the Sonic Hedgehog (Shh) gene into the irradiated parotids of pigs. Shh genes were delivered at four and sixteen weeks post irradiation. In both cases, the relative saliva flows were better than the control group. Furthermore, Shh was shown to increase blood flow, another mechanism by which salivary function may be restored [5]. This data has been reproduced in similar studies involving other animals but is yet to be evaluated in humans.
Conclusion
Current treatments for hyposalivation are limited by their efficacy and have a debatable impact on patient quality of life. Overall, while MSC-based approaches show promise in improving salivary function, comprehensive, large-scale studies are needed to establish their long-term effectiveness and broader applicability. Similarly, gene therapy is an evolving prospect, but optimism can be retained in the knowledge that clinical trials are ongoing, and their results are eagerly awaited.
References
1. Turner MD. Hyposalivation and xerostomia: etiology, complications, and medical management. Dent Clin North Am 2016;60(2):435–43.
2. Xu J, Wang D, Liu D, et al. Allogeneic mesenchymal stem cell treatment alleviates experimental and clinical Sjögren syndrome. Blood 2012;120(15):3142–51.
3. Grønhøj C, Jensen DH, Vester-Glowinski P, et al. Safety and efficacy of mesenchymal stem cells for radiation-induced xerostomia: a randomized, placebo-controlled phase 1/2 trial (MESRIX). Int J Radiat Oncol Biol Phys 2018;101(3):581–92.
4. Baum BJ, Alevizos I, Zheng C, et al. Early responses to adenoviral-mediated transfer of the aquaporin-1 cDNA for radiation-induced salivary hypofunction. Proc Natl Acad Sci U S A 2012;109(47):19403–7.
5. Hu L, Zhu Z, Hai B, et al. Intragland Shh gene delivery mitigated irradiation-induced hyposalivation in a miniature pig model. Theranostics 2018;8(16):4321.
Declaration of competing interests: None declared.









