
Per-oral surgical access to the larynx can be hampered by the presence of an endotracheal tube. Various systems have been developed for tubeless ventilation, but these all carry a risk of aerosolisation of secretions with obvious inherent risks. We hear about a novel approach to ventilation.
Conventional ventilation supports inhalation by supplying gas at a certain volume (volume controlled ventilation - VCV), or pressure (pressure controlled ventilation - PCV). Expiration is passive, depending on elastic properties of the lungs and the chest wall. Risks of positive pressure ventilation are known: barotrauma, volutrauma, atelectasis, oxygen toxicity, and ventilator induced lung injury (VILI).
Various lung-protective strategies are being researched ever since the 1960s, with the low tidal volume strategy studied in the famous ARDS Network trial published in 2000 being the most widely adopted to reduce mortality in ARDS (acute respiratory distress syndrome). Nevertheless, VILI remains a clinical problem.
Traditionally, lung-protective ventilation focuses on optimising the inspiration phase which represents only 30-50% of the (artificial) respiratory cycle. In 2014, Goebel and colleagues investigated the expiration phase and showed that slowing down the mechanical exhalation, or linearisation of the expiratory gas flow, can limit lung damage.
EVA and FCV: unique ventilation methods
Expiratory ventilation assistance (EVA) has a fully controlled ventilation cycle. Both inward and outward gas flows are constant and linear. Addition of resistance in the respiratory circuit, and expiratory assistance by suctioning (using the Venturi effect), make the exhalation controlled.
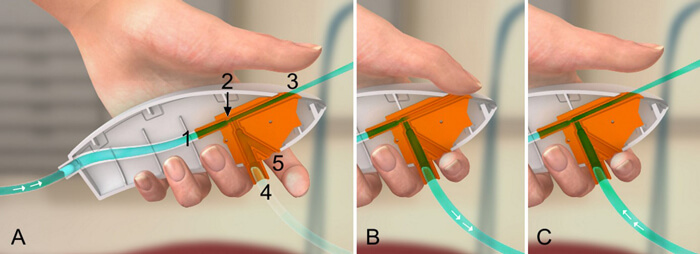
Figure 1. The mechanism of expiratory ventilation assistance (EVA) is explained by the cross section of Ventrain above. The gas flows via the inlet (1) through a very narrow nozzle (2) and exhaust pipe (3) to the outside. The narrow nozzle (2) accelerates the gas and, according to Bernoulli’s principle, creates a sub atmospheric pressure entraining gas from port (4), which is connected to the patient catheter. The bypass (5) functions as an on/off switch.
A) When bypass (5) is opened, there is no significant positive or negative pressure at the catheter tip, resulting in equilibration/safety mode. Closing bypass (5) enables ventilation as in B and C.
B) Closing exhaust pipe (3) results in inspiration flow through port (4).
C) Opening exhaust pipe (3) results in an active expiration.
EVA was first used with the handheld ventilator, Ventrain (Ventinova Medical BV; Figure 1) via extremely thin (ID 2.0 mm) ventilatory tubes, to ventilate critically obstructed airways. These tubes could be placed via both the subglottic (needle cannula) and oral routes. Ventrain has been very effective, even lifesaving, in reoxygenation during hypoxia, laryngeal surgery and single lung ventilation [1]. Success with the manual application of EVA, led to its automated form: FCV®, delivered through mechanical ventilator Evone® (Ventinova Medical BV, Eindhoven, the Netherlands). FCV keeps both inspiratory and expiratory gas flows constant, with the ventilatory pressures being preset (PEEP and Ppeak). This results in linear rise and fall in intra-tracheal pressures (Figure 2).
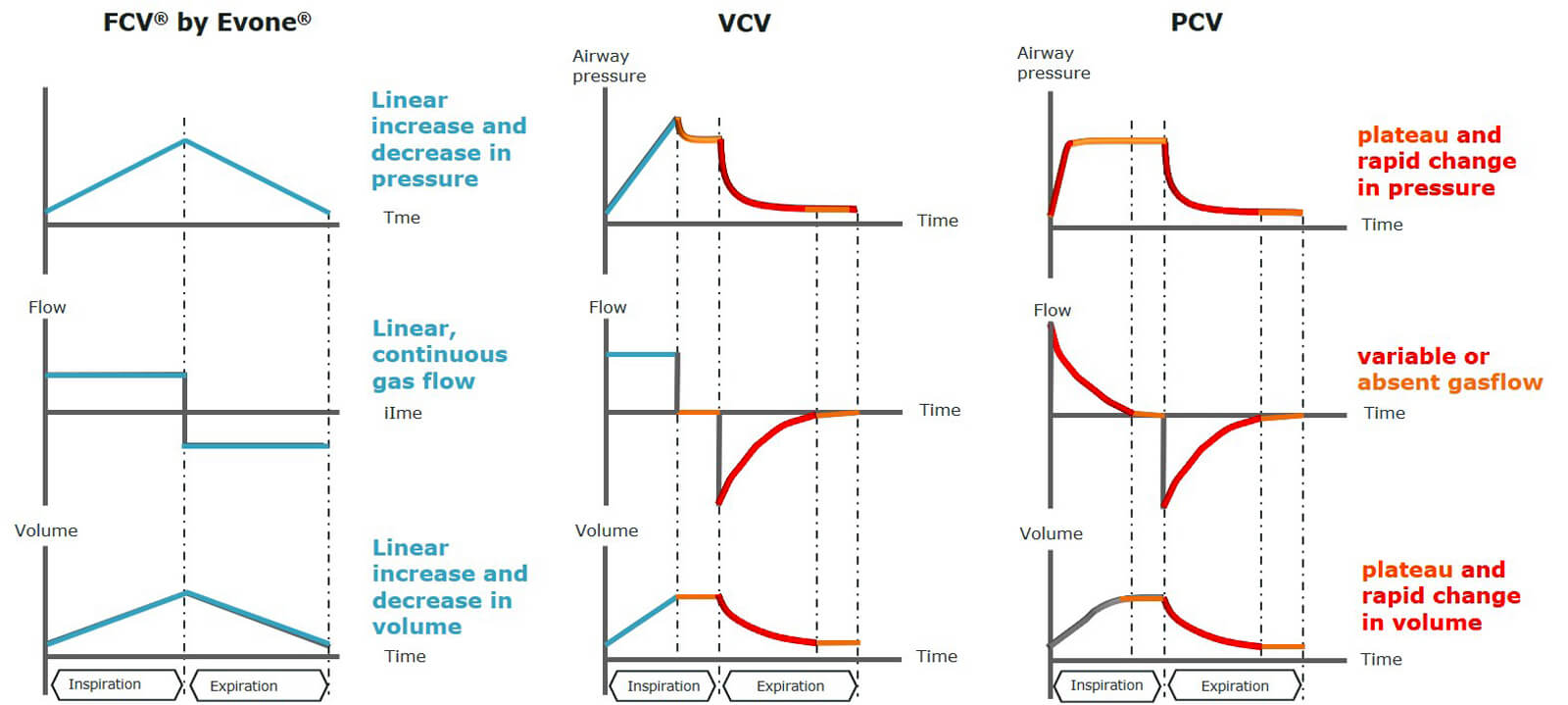
Figure 2. FCV has linear pressure, flow and volume changes in inspiration and expiration. Both VCV and PCV have variable flow and volume changes, periods with no flow and rapid pressure drops especially in exhalation.
Unlike during VCV and PCV, there are no significant periods without flow. Like EVA, FCV® requires a high resistant breathing circuit in order to fully control both the inspiration and expiration phase. This resistance can be applied using an ultra-thin, cuffed endotracheal tube Tritube (Figure 3; outer diameter of 4.4mm) or using a high resistant breathing tubing to allow ventilation through a conventional endotracheal tube (ID >5mm).
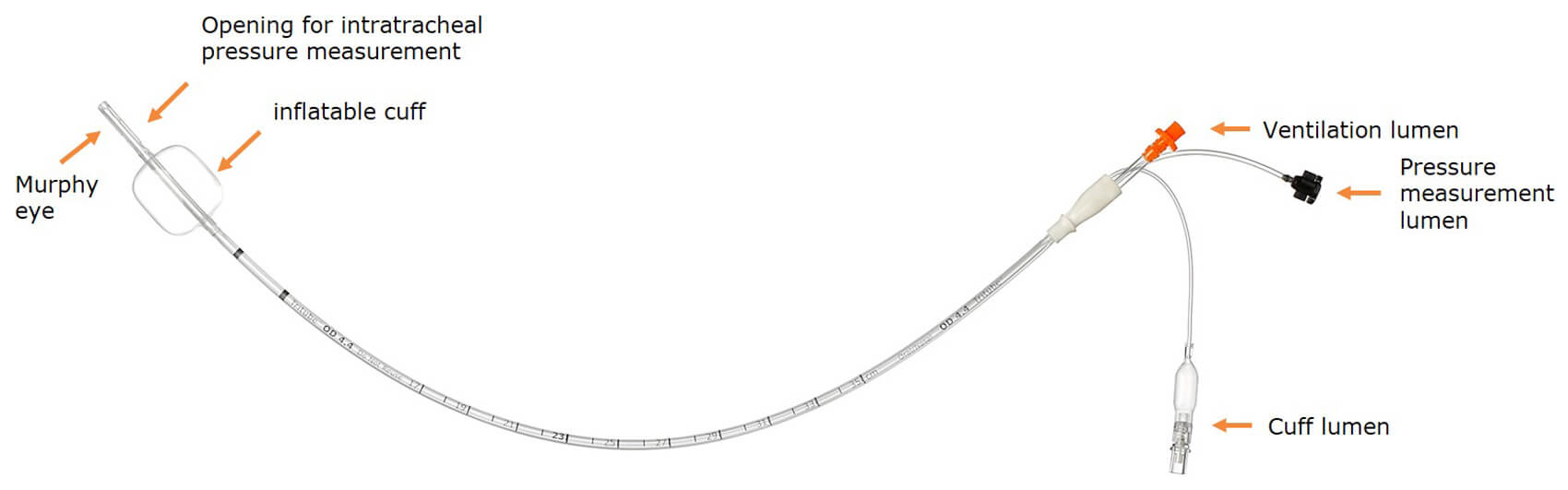
Figure 3. Tritube (cuffed endotracheal tube (4.4mm OD) for adults in combination with Ventrain/ Evone) with a distal opening for measuring intratracheal pressures.
The first multicentre observational study with clinical application of FCV® in combination with Tritube showed adequate etCO2 levels with relatively low minute volumes. The thin ventilation tube was a valuable extension of the instruments for airway surgery. [2]
FCV: ventilating through a thin tube
In a case series of laryngeal surgery, Michael Kristensen and colleagues combined Tritube with Ventrain. In 2017 he described an unprecedented good visibility of the airways during oral and upper airway procedures. [3]
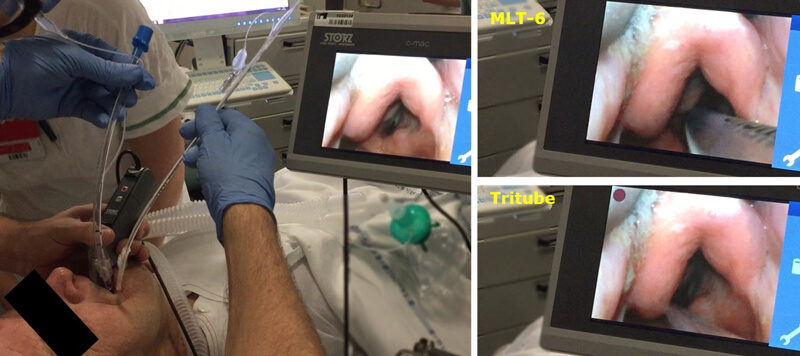
Figure 4. In situ comparison of MLT-6 (right top photo) and Tritube (right bottom photo) during intubation. (www.airwaymanagement.dk)
Two randomised controlled trials [4,5] confirmed the benefits of Tritube over an MLT-6 tube during laryngeal surgery (Figure 4). Kristensen and colleagues showed that in patients with predicted difficult airways intubation conditions, surgical conditions and visibility were significantly improved. Patients tolerated the Tritube (cuff deflated) during postoperative maintenance of airway access just as well as a tube changer: they could breathe/talk while still being intubated.
High pressure jet ventilation uses a thin tube but needs an open airway to prevent barotrauma. Recognised drawbacks include moving anatomy through backflow, moderate CO2 elimination, aspiration risk and contamination risk for the surgeon. The exact advantages of FCV over jet ventilation have not been studied but seem evident, as FCV uses a cuffed tube to reduce contamination risk and aspiration risk, prevents moving anatomy and eliminates CO2 effectively. This reasoning was recently confirmed by Prof Vander Poorten and colleagues who used Tritube and Evone in 15 patients undergoing upper airway surgery [6].
FCV: keeping the lungs open and a more efficient ventilation
In lung healthy patients, FCV improves oxygenation and CO2 removal, with higher mean tracheal pressure [7]. In obese patients FCV better maintains end expiratory lung volume as compared to VCV, indicating less incidence of atelectasis [8]. The results of these studies are in line with previously published preclinical studies. In pigs with both normal lungs, and ARDS, FCV showed better arterial oxygenation with lower minute volumes, better aeration, reduced atelectasis (Figure 5), and less lung damage at the alveolar level.
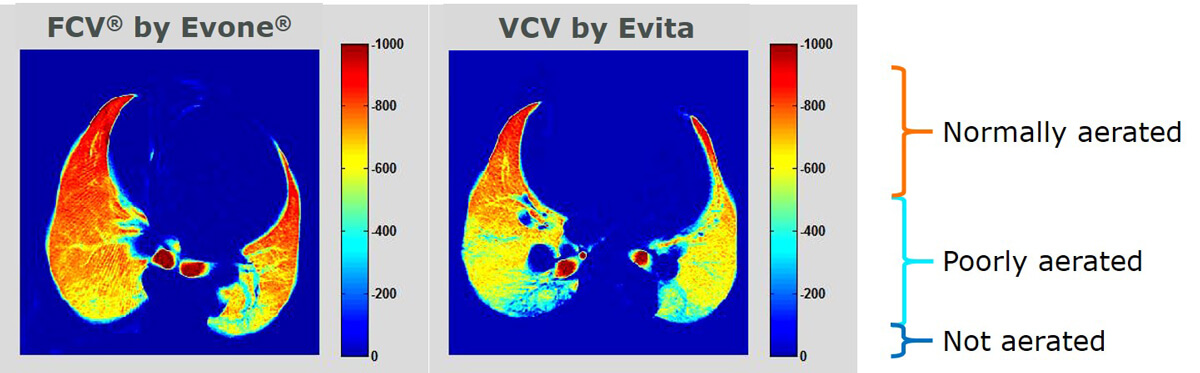
Figure 5. CT scan images of porcine lung ventilation with FCV (left), giving better aeration compared to VCV (right) [9].
Better lung aeration and a more effective ventilation with FCV may have positive effects on the development of postoperative lung complications that are correlated to atelectasis and poor gas exchange.
FCV limitation of lung damage
Mechanical ventilation can cause tissue damage through energy dissipation (surface area of pressure volume loop) into the lung: this can be calculated by measuring intratracheal pressures (Figure 6). Evone is unique in reliably measuring pressures actually in the trachea, unlike conventional ventilators, that calculate airway pressures from pressures measured at the ventilator side of the respiratory circuit. Barnes and Enk showed in a single patient study that FCV, with constant linear flow and lower shear stress, dissipates about 0.17 J/L energy – this is approximately half of the energy dissipated by PCV and two thirds of that by VCV, and also within the normal physiological range (0.2-0.7 J/L.) Thus, FCV leaves little extra energy to be absorbed by the lungs, thereby reducing the risk of tissue damage.
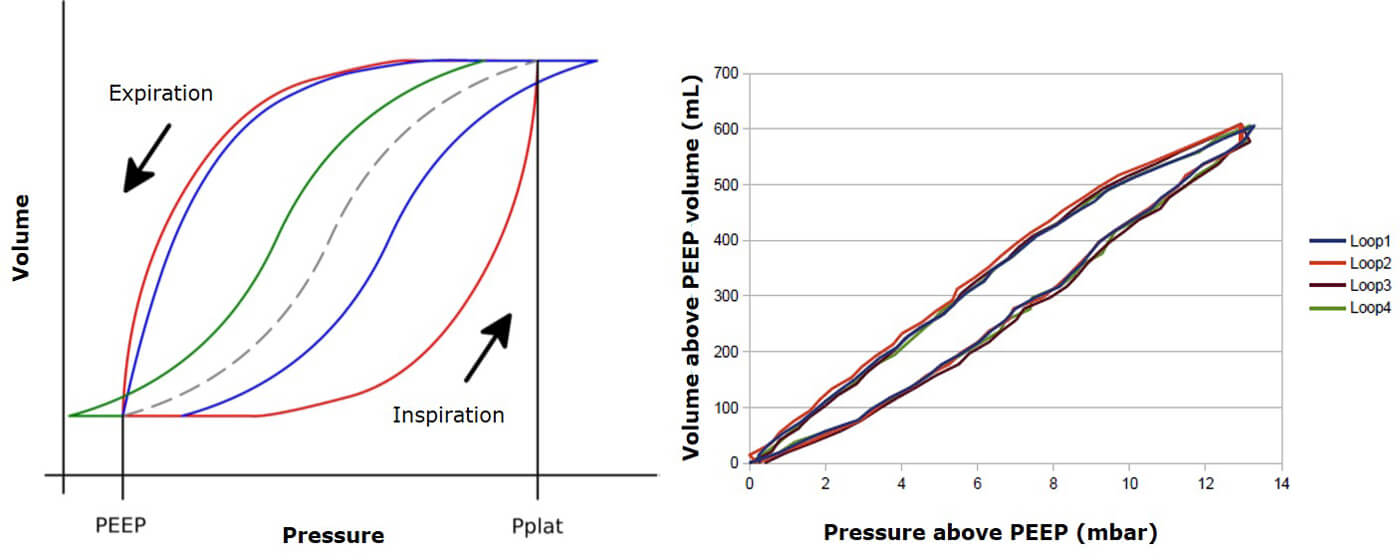
Figure 6. (Left) Schematic PV loops: the area of the loop = amount of dissipated energy during FCV (blue line during inspiration, green line during expiration), VCV (blue line) and PCV (red line). The dotted line = static compliance. (Right) Clinically measured PV loops during FCV ventilation with Evone. The small area of the PV loops shows a minimised energy dissipation [10].
FCV future directions
FCV is simple and innovative: by controlling both inspiration and expiration, it simulates natural breathing (gas flow). The above studies confirm its increased ventilation efficiency, better lung recruitment, the potential to reduce lung damage, and the benefits of a thin tube with cuff during laryngeal surgery. The scientific evidence for the clinical benefits is unambiguous but limited. Further research is needed to further evaluate the extent of (potential) benefits of FCV, and whether there are any limitations. The effects of FCV during long-term ventilation in intensive care remain to be investigated. Possibly, critically ill patients with a relatively high risk of VILI benefit from this new method of ventilation.
References
1. Doyle DJ. Ventilation via Narrow-Bore Catheters: Clinical and Technical Perspectives on the Ventrain Ventilation System. The Open Anesthesia Journal 2018;12:49-60.
2. Schmidt J, F Günther, J Weber, et al. Flow-controlled ventilation during ear, nose and throat surgery: A prospective observational study. Eur J Anaesthesiol 2019;36(5):327-34.
3. Kristensen MS, de Wolf MWP, Rasmussen LS. Ventilation via the 2.4 mm internal diameter Tritube® with cuff - new possibilities in airway management. Acta Anaesthesiol Scand. 2017;61(6):580-9.
4. Schmidt J, Guenther F, Weber J. et al. Glottic visibility for laryngeal surgery: Tritube vs. microlaryngeal tube: A randomised controlled trial. Eur J Anaesthesiol 2019;36(12):963-71.
5. Kristensen MS, Abildstrøm HH. Endotracheal video-laryngoscope guided intubation with a 2.4 mm cuff’ed tube and active expiration by a dedicated ventilator versus a standard tube/ventilator. A randomized single blinded study in patients with a predicted difficult airway. - A paradigm shift in airway management? Abstract published at Euroanaesthesia 2019. 2019;3755.
6. Meulemans J, Jans A, Vermeulen K, et al. Evone Flow-controlled Ventilaiton during upper airway surgery: A clinical feasibility study and safety assessment. Frontiers in Surgery 2020;7:6.
7. Weber J, Schmidt J, Straka L, et al. Flow-controlled ventilation improves gas exchange in lung-healthy patients— a randomized interventional cross-over study. Acta Anaesthesiologica Scandinavica 2020;64:481-8.
8. Weber J, Straka L, Borgmann S, et al. Flow-controlled ventilation (FCV) improves regional ventilation in obese patients – a randomized controlled crossover trial. BMC Anesthesiology 2020;20:24.
9. Schmidt J, Wenzel C, Mahn M, et al. Improved lung recruitment and oxygenation during mandatory ventilation with a new expiratory ventilation assistance device: A controlled interventional trial in healthy pigs. Eur J Anaesthesiol 2018;35(10):736-44.
10. Barnes T, Enk D. Ventilation for low dissipated energy achieved using flow control during both inspiration and expiration. Trends in Anaesthesia and Critical Care 2019;24:5-12.





