Where in the world is Halifax? Many outside of Canada have never heard of the Maritime Canadian town of Halifax. Before leaving to start a year-long fellowship there, we both had to answer many questions from family and friends about where it was, how cold it would be and if we would need a sled to get to work.
Halifax is the capital of Nova Scotia, Canada, with a population of approximately 400,000 in its metropolitan area. It is a harbour city located on the east coast in a region called the Maritimes or Atlantic Canada, affectionately known as the friendliest part of Canada. It is a small city with a lot of charm, more temperate weather than many other parts of Canada and it is certainly possible to walk to work in the winter. There are still the Canadian essentials, like maple leaves, snow and ice hockey; but it’s all served with lobster, donair (a local delicacy) and fresh, salty air. Halifax has the feel of a very down to earth place with a very practical, easy going attitude.
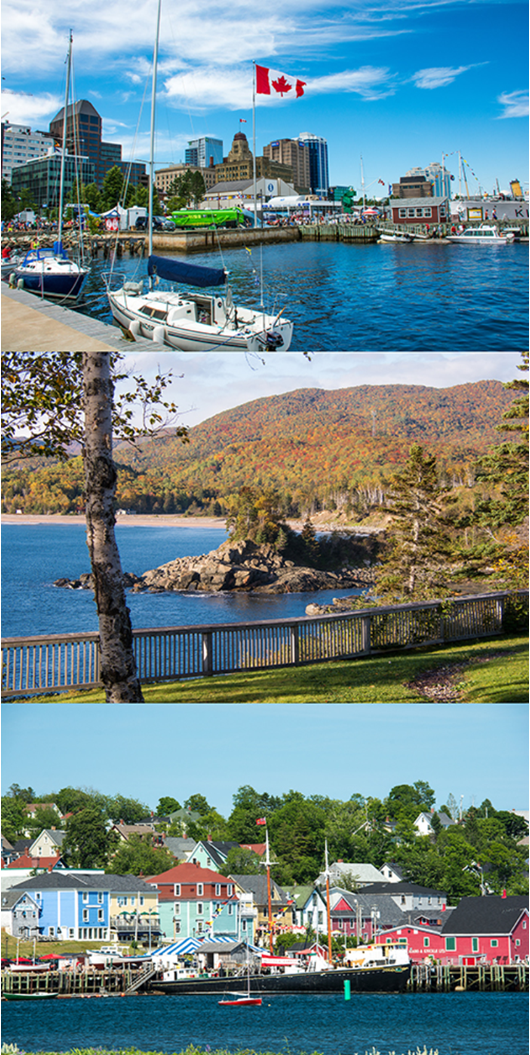
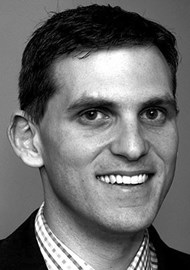
Figure 1: (Top to bottom) A view of Halifax from the waterfront boardwalk; Ingonish beach on Cape Breton Island;
Lunenberg, a port town on the south shore of Nova Scotia, western side of Mahone Bay, a UNESCO World Heritage Site.
The main hospital in Halifax is the Queen Elizabeth II Health Sciences Centre which is a large teaching hospital affiliated with Dalhousie University. It is an amalgamation of multiple hospital sites, the largest two being Victoria General and Halifax Infirmary, each with a main hospital and a number of ancillary buildings on their respective campuses. The IWK Health Centre is adjacent to Victoria General and provides paediatric, obstetric and gynaecological services. These hospitals provide tertiary and quaternary otorhinolaryngological specialist care for four Maritime Canadian provinces: Nova Scotia, Newfoundland, Prince Edward Island and New Brunswick, with a combined population of almost 2,000,000.
“There was an abundance of research opportunities in otology, both in contributing to a number of existing projects and the initiating of new ones.”
There are a range of surgical fellowships on offer at the hospitals in Halifax. There are two offered in ENT in both head and neck surgery and otology and neurotology. Over 2015/16 these fellowships were both simultaneously filled by Australian ENT surgeons. By coincidence there was also an Australian anaesthesiology fellow and two Australian orthopaedic surgery fellows, along with fellows in other specialties from many different countries, including Switzerland, Japan and China.
Otology / Neurotology Fellowship
The Otology / Neurotology Fellowship has been running for well over 10 years and is open to international and Canadian applicants. It is awarded following an application and competitive interview process. The successful candidate is selected by the start of the year preceding their July start date. The fellowship is also now associated with the TWJ Foundation, which will be sending a UK Fellow to Halifax every third year commencing in July 2017.
The fellowship co-supervisors are Manohar Bance and David Morris. Professor Bance is the Head of the Division of Otolaryngology at QEII Health Sciences Centre and the Director of the Ear and Auditory Research (EAR) and Sensory Encoding and Neural Sensory Engineering (SENSE) research labs at Dalhousie University. Dr Morris is also the Fellowship Director and was the first fellow in the position in 2002. Additionally, he is also very involved in teaching and medical education through Dalhousie University. Both supervisors complement each other very well, with both being excellent surgeons and clinicians, but each providing fantastic opportunities for research and teaching experience.
Figure 2: (L-R) Nicholas Jufas, David Morris and Manohar Bance in the outpatient clinic
on a Friday wearing customary bow ties marking the end of the working week.
There was a large amount of operating experience in the fellowship in otology / neurotology. In principle, each supervisor had at least one full day per week of operating which resulted in a total of at least two days per week for the fellow. In practice, extra lists and combination cases with neurosurgery resulted in an average of at least three operating days per week.
The operating rooms were well equipped with the latest microscopes, endoscopes and instruments. There were a number of trials and studies performed in the operating room, as well as a wide exposure to a range of procedures. Just over 450 operative procedures were performed during the course of the year, with a more specific breakdown of case numbers as follows:
- Tympanoplasty and / or ossiculoplasty – 178
- Mastoidectomy and / or mastoid obliteration – 73
- Cochlear implants (equal distribution of Cochlear / MED EL / Advanced Bionics) – 41
- Stapedotomy – 31
- Bone anchored devices (either per- or trans-cutaneous) – 18
- Vestibular schwannoma or other intracranial pathology – 12
Other cases included:
- Semicircular canal obliteration
- Eustachian tuboplasty
- Endolymphatic sac surgery
- Middle ear implants
The outpatient clinics for otology / neurotology were busy but there was always opportunity for thorough clinical diagnosis and discussion about more complex cases with the consultant and residents. They usually occurred two days per week, one with each supervisor. Patient referrals to the clinic were limited solely to otologic problems, and most of these were tertiary referrals with complex and multiple issues. The clinics were extremely well stocked, with an abundance of equipment and the latest technology (including microscopes, endoscopes and several high definition television screens in each room).
Minor procedures such as tympanoplasty, and even percutaneous bone anchored hearing aids using a minimally invasive approach were also performed in the clinic. There was a full complement of experienced nursing staff on hand to assist, as well as a very experienced audiology department in adjoining rooms available every day for a full range of diagnostic testing. Researchers were also on hand in the adjoining laboratories for patients that were suitable for participation (with consent) in a number of ongoing studies. Finally, a number of specialty clinics were also held monthly, including a Maritime Lateral Skull Base Clinic, a Video Endoscopic Evaluation of Eustachian Tube (VEET) Clinic and a Paediatric Otology Clinic.

Figure 3: (L-R) Mark Taylor and Eric Levi sporting facial hair growth during ’Manuary’,
raising funds to support research and improve clinical care for those with head and neck cancer.
There was an abundance of research opportunities in otology, both in contributing to a number of existing projects and the initiating of new ones. During my year, these involved research in optical coherence tomography, sonotubometry, and feasibility studies on a number of novel endoscopic approaches.
Finally, there was the opportunity to attend and present at a number of conferences, including the AAO-HNS Annual Meeting in Dallas, COSM in Chicago, CI2016 in Toronto, CSO-HNS Annual Meeting in Charlottetown, Chole 2016 in Edinburgh. The opportunity to do this certainly strengthened the fellowship experience as well as the professional relationship with the supervisors.
Head and Neck Surgery Fellowship
This would be the third time that this position was filled by a fellow from Australasia. Like the previous two RACS fellows, this fellowship has exceeded personal expectations. The breadth and depth of experience on offer is fantastic.
There are four full-time faculty head and neck surgeons in the department. The Fellowship Director is the current President of the Canadian Academy of Facial Plastic and Reconstructive Surgery and also the upcoming President of the Canadian Society of Otolaryngology, Professor S Mark Taylor. He has special expertise in transoral laser microsurgery and facial plastic surgery. The other staff members, Jonathan Trites, Rob Hart and Matthew Rigby, provide an array of subspecialty ablative, reconstructive and endocrine head and neck services. They’re a wonderful team with complementary skills and an absolute delight to work with.
On a typical week, there is a Multidisciplinary Tumour Board Meeting where about 15 cases are discussed. There would be four to five full days of operating with concurrent head and neck operating rooms on some days. This is in conjunction with clinics and minor operative surgery sessions where facial plastic (e.g. facelifts, eyelids) and minor oncologic procedures are performed (e.g. skin excision, auricle, local flaps). There are also the occasional combined cases with other specialties, such as carotid body tumour excision, etc. The biggest problem often encountered is the dilemma of choosing where to be and which operating list to attend because there are too many good things going on at the same time.
My 12-month operative logbook looked like this:
- Free flaps – 34
- Pedicled flaps – 73
- Neck dissections – 121
- Transoral laser microsurgeries – 67
- Total laryngectomies – 11
- Mandible, maxilla surgery – 51
- Total thyroids, hemithyroids, parathyroids – 73
- Parotidectomies – 24
- Open rhinoplasties – 12
- Blepharoplasties, facelifts – 25
There was most certainly a broad range of head and neck procedures with a volume that would prepare me extremely well for my practice in the Australian setting. Research opportunities are plentiful. The fellowship is exclusively head and neck, which means that the exposure to general ENT, rhinology, neurorhinology, and paediatric cases is limited.
Overall
There was significant department integration and involvement. Grand rounds is held every Wednesday morning, and Journal Club held every month. Teaching of residents and medical students was an integral and enriching experience within the fellowship. This occurred in both formal and informal sessions in the operating room, clinics, wards and emergency room. Both fellows are also appointed as clinical lecturers to Dalhousie University.
There were two dissection courses held over three days, each in the anatomical laboratories at Dalhousie University over the year. Fellows joined the staff in teaching residents over these days.

Figure 4: (Top to bottom) View of Victoria General Hospital and the IWK centre,
one of the QEII Health Sciences Sites in Halifax during the summer; View from the operating
suites at Victoria General east toward Halifax harbor during the winter.
Both fellowship positions are paid a salary, which is a major advantage given how expensive a fellowship year can be. There is also an on-call requirement on the consultant / staff roster during the year, which further supplements the salary. While living costs in Halifax were not considerably different from Australia; the costs of relocating to a new place, with our families for both of us, are significant. However, the benefit of our fellowship year in Halifax was immeasurable, both professionally and personally.
There were practical challenges in the relocation process for both of our families. The seemingly insurmountable paperwork requirement to apply for medical registration in Nova Scotia felt never-ending in the months prior to leaving for Halifax. Despite being warned by colleagues to start the process several months before commencing the fellowship, it seemed that there was an inbuilt design for it to take up until the last minute. There was also a frequent sense of being in a vicious circle – where in order to complete a step you needed something that could only be obtained by completing the very same step! Needless to say we both were victorious in our battle with bureaucracy in the end.

Figure 5: (Top to bottom) Supporting the local Halifax Mooseheads Hockey Team during the season;
MacDonald Bridge across Halifax Harbour adorned with Canadian flags on Natal Day;
The annual Harvest Hootenanny and Pumpkin Smash to dispose of accrued gourds after Halloween.
Another noteworthy challenge that we and our wives faced early on in our year in Nova Scotia was sitting our driving tests, both written and practical, as Australian licences are not recognised in Nova Scotia. As it was summer when we arrived, we all lined up with nervous teenagers who had just started school holidays. We studied the road rule book and learnt together how to interpret road signs with moose silhouettes and which part of the road would freeze first.
“The biggest problem often encountered is the dilemma of choosing where to be and which operating list to attend because there are too many good things going on at the same time.”
Halifax proved itself many times over to earn the mantle of one of the friendliest places to live in Canada. Our families quickly made friends with people in the neighbourhood, and not just through connections with the hospital. People were welcoming and there were constant community events and festivals throughout Nova Scotia. During the early summer months, we picked blueberries in the Annapolis Valley, visited Prince Edward Island and the picturesque Lunenburg and Peggy’s Cove.
In the autumn, we carved jack-o’-lanterns and got lost in a corn maze. In winter, our kids learnt to ice skate at the Halifax Commons outdoor ice skating and went sledding downhill from the Halifax Citadel. In the spring we went into the Cobequids to see maple trees being tapped and their sap boiled into delicious maple syrup.
In the year, we learnt a phenomenal amount and will return to Australia with a different and new perspective as ENT surgeons and as people. The augmentation that a fellowship such as those on offer in Halifax brings to what is already rigorous specialist training cannot be measured. Living for a year in a foreign country brings a new appreciation for friends and family back home but also broadens your ability to appreciate the many different ways that people live on this planet. And ultimately, that understanding will help us to connect with future patients, from all walks of life. All we can say is that if you are contemplating undertaking a fellowship, in particular in Halifax, we are certain that you will look back after the year is done and wonder why you ever hesitated.