Here, ENT trainees share their experiences of adaptations to both clinical practice and training during the COVID-19 pandemic. We welcome other colleagues from around the world to share their experiences with us via social media or the website.
Australia
Olivia Ruskin, ENT Trainee, Alfred Hospital, Victoria, Australia.
March 2020 marked significant changes to life - in ENT and otherwise - here in Australia. The high risk to ENT surgeons was realised from experience and communication from overseas – in particular the UK and USA. Substantial changes were made to ENT training and practice. The body governing training, The Australian Society of Otolaryngology Head and Neck Surgery (ASOHNS) released clear and overarching directives for safe practice.
Many ENT teams were divided to work alternate weeks; but no trainees underwent redeployment out of specialist training. Unit meetings were held using programs such as Microsoft Teams or Zoom. The curtailment of all non-urgent elective surgery by the Australian Government has no doubt been disadvantageous to training; however, the trade-off has been that no hospital has been under-resourced for management of COVID patients. Currently elective surgery is resuming across the country.
Clinical contact and patient exposure reduced dramatically as online and virtual forms of communication increased and fast became the norm. Face-to-face consultations in the outpatient setting reduced and telephone and telehealth methods were instituted to varying degrees. Patients requiring urgent care were still able to receive it.
Compulsory conferences and courses for trainees were all cancelled. Some were converted to virtual formats for login at the viewers’ convenience. ENT trainees usually attend a weekly tutorial in their respective training state; these are now broadcast via webinar.
The disruption to ENT training has not been without cost, and the longer-term implications for training are now being addressed. Whilst we miss the collegiality of regular tutorials and conferences, the necessary modification into virtual formats does bring some convenience and flexibility to training. Additionally, any sacrifices made to training have ensured the safety of our colleagues and community.
Canada and United States
Kiersten Pianosi, PGY 4 Resident, Department of Otolaryngology - Head & Neck Surgery, University of Western Ontario, Canada.
Cautiously optimistic: that is the feeling as we go from strict self-isolation protocols to staged reopening. In Canada, this acts as a strange marker of success – ‘the curve has been flattened.’ In healthcare though, the transition brings a mixture of nervousness and hope.
When COVID-19 entered pandemic status, there was uncertainty and anxiety. As the number of coronavirus cases rose, the healthcare system scaled back on clinics and surgeries to reduce exposure. A drastic decrease in elective, and even semi-urgent, surgeries equated to a drastic decrease in clinical volume.
This impact was felt across the country, and many residency training programmes switched from their regular rotation schedules to team-based approaches.
The team-based approach was effective in reducing unnecessary exposures and allowing for self-isolation in the time following a period on service. Even when in the hospital, surgical cases were only attended by one resident. There were strict guidelines. During this time, there was looming anxiety with the threat of insufficient PPE, and uncertainty as to when we may regain a sense of normalcy.
With surgeries drastically decreased, the operative component of our residency training was impacted. Senior residents went from operating four-to-five days per week, to operating four-to-five days per month. However as one aspect of residency training was hindered, another was heightened: didactic learning.
Teaching sessions were moved to online platforms and offered to residents across Canada, rather than simply a home institution; a half-day academic teaching programme was viewed by half of the other programmes across the country! Larger institutions in the United States partnered to form a collaborative multi-institutional education programme, offered throughout the day, every day. Dr John Oghalai, Chair of the Department of Otolaryngology - Head and Neck Surgery at the University of Southern California Caruso, and one of the lead organisers of the Collaborative Multi-Institutional Otolaryngology Residency Education Program, said he was very privileged to work with a stellar faculty from around the US to develop the programme: “The interest level was very high and I am grateful that people found it meaningful and educational. The recorded videos are still each being watched 500-600 times in the two to three weeks after being posted. To date, we have over 36,000 views of the recorded videos. We will keep the site up in the years to come and permit the addition of further recorded videos.” As residents, we’d had the opportunity to learn from experts in the field, that we otherwise may never have encountered.
In true Canadian spirit, amongst the chaos and uncertainty, a message prevailed; one of unity and community. Residents are keen to increase their operative exposure, and hopeful to maintain the decrease in COVID-19 exposure… That is the cautious optimism.
United Kingdom
Anika Kaura, ENT Registrar, Clinical Research Fellow, UCL Ear Institute, UK and Sheneen Meghji, ST6 ENT Registrar, James Paget University Hospital, East of England.
The education committee for the Association of Otolaryngologists in Training (AOT), has been instrumental in coordinating this new way of teaching and training in the UK. A new education calendar gives a timetable of all webinars, links with how to register, and access to previously recorded talks.
The first online lectures were aired on 12 April by ‘ENT Grand Rounds’. Mr Rajeev Mathew has led this initiative: “We set up ENT Grand Rounds to help maintain team spirit and continued learning during a time of great change for doctors during the pandemic. We covered important curriculum topics, as well as some interesting non-clinical topics such as the Science of Aerosol, Sustainable Surgery, and Mental Wellbeing. We have been overwhelmed by the participation and positive feedback and hope to keep this initiative going.” The first lecture, on the Science of Aerosol, saw more than 95 people logging on.
Since then, regular sessions have been introduced by Barts ENT Online Teaching, the National Association of Programme Directors in ENT (NAPDENT), British Association of Paediatric Otolaryngology (BAPO) and others. To date there have been more than 50 lectures and training days delivered online, with participant number rising to 300 for the NAPDENT Otology Training day. The team at Barts ENT Online Teaching shared: “We feel that online teaching will be the ‘new normal’ and has already shown to be able to reach a wider audience. We have had attendees from Jamaica and Kenya; it has already been much more successful than we had anticipated and there is a huge appetite for more!”
As with anything new, there has been a steep learning curve in delivering online teaching. Problems have included poor connectivity, reaching participant capacity, and unwanted guests! There was a resultant quick education in online safety and acquisition of more robust, capacious resources.
Whilst we all hope that traditional surgical training returns soon, COVID-19 has changed the way we work. A silver lining has been the accessible, exceptionally high-quality education for all, from national and international faculty. We hope this will continue beyond the pandemic and recovery phase; and in the ‘new normal,’ will we ever need to travel to regional training days again?
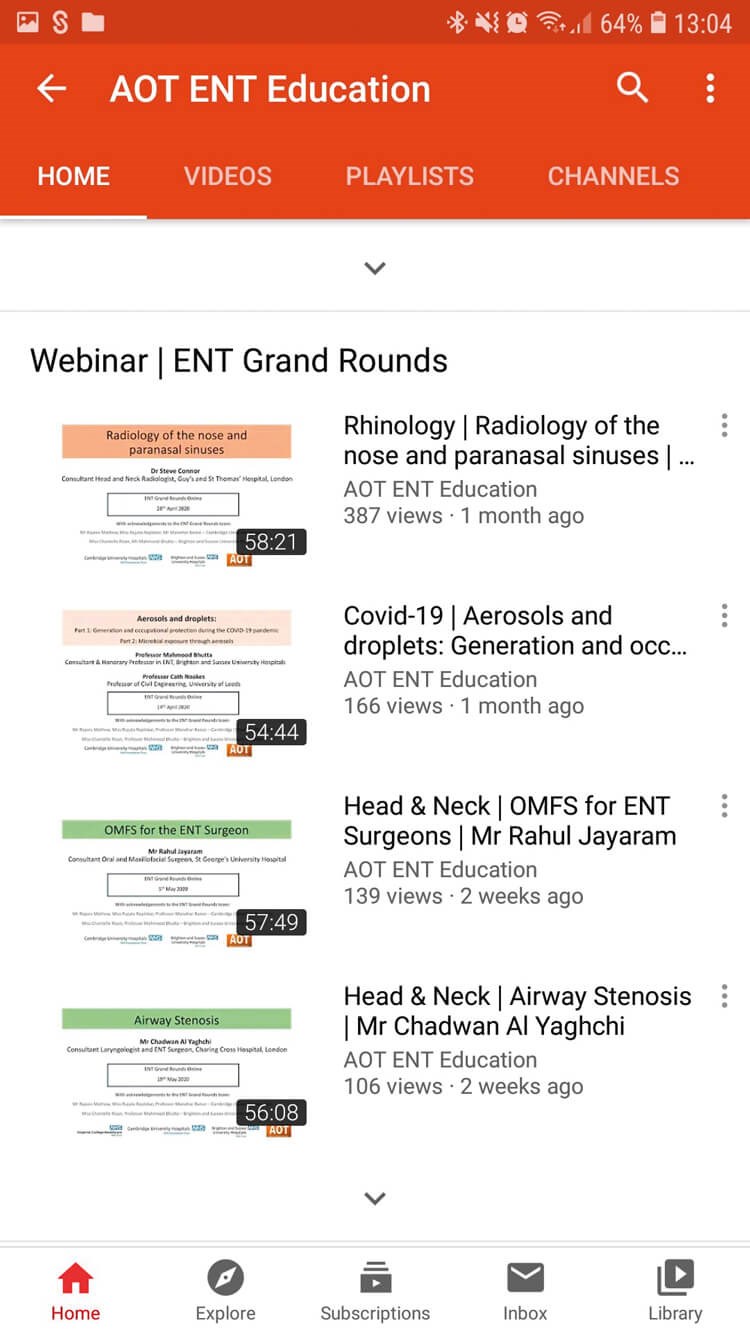
Online lectures have been made available on the AOT ENT Education
youtube channel, including ENT Grand Rounds webinars.
Trainees have found the altruism of trainers and educators, as well as peers, is a positive in an otherwise unpleasant and difficult time. As our writers have highlighted, alongside the new normal that may make itself apparent in clinical work, there is potential for a new – and perhaps better – normal for ENT training.
It’s important, as the acute phase of the pandemic changes, to recognise that trainees will perhaps not have as much free ‘down’ time to receive training outside of the formal training environment (whatever that will be in the new normal).
“The trade-off has been that no hospital has been under-resourced for management of COVID patients”
The success and popularity of the remote teaching options has meant occasionally, there have been two or three webinars scheduled in an evening. Sessions that ran during working hours, and/or as ones that trainees can take study leave for, circumvent this. It also does not place an unfair pressure, and possibly exclude, those trainees with carer or similar out-of-work commitments. Surgical training must be mindful of not placing pressure on trainees’ and trainers’ free time as clinical work returns.
A webinar cannot be a substitute for surgical training. However, in the new normal, considerations regarding PPE and managing exposure risk impacts on timing for a theatre list. With fewer cases in the same theatre lists, trainees may find their hands-on experience is reduced in quantity. However, with the enthusiasm of trainers and educators for the alternative modes of delivering didactic training and sharing their knowledge and experience, there is great potential. If we can achieve the marriage of enthusiastic education and training on a webinar, with focused theatre experience, the new normal may maximise the quality of hands on surgical training.









