Richard Gans and Kimberly Rutherford, renowned experts from The American Institute of Balance, give their team’s overview of the stages involved in reaching ‘diagnosis based strategies’. For the dizzy patient, this focuses on patient-centred clinical pathways for individualised therapy with an MDT approach.
According to leading epidemiologists, dizziness ranks as the number one complaint made to physicians by patients 65 years and older. More importantly, perhaps, is that dizziness is the third most common complaint made by all adult patients, preceded only by headache and lower back pain.
Clearly, these symptoms are not only common, but account for a significant percentage of physician office visits, as well as considerable laboratory and radiographic imaging costs, and the incalculable cost of human pain and suffering. When balance dysfunction and the consequence of falls in the older population are factored in, it is not surprising that equilibrium disorders were classified as early as 1995 by the National Institutes of Health, as a national healthcare crisis in the USA. This article will present the current evidence-based models and the team approach of physicians, audiologists and physiotherapists, used and taught for over 25 years by the American Institute of Balance.
“Once a preliminary diagnosis has been established, a comprehensive neuro-diagnostic evaluation is conducted based on the nature of the patient’s history and symptoms”
Causes of equilibrium dysfunction and target populations
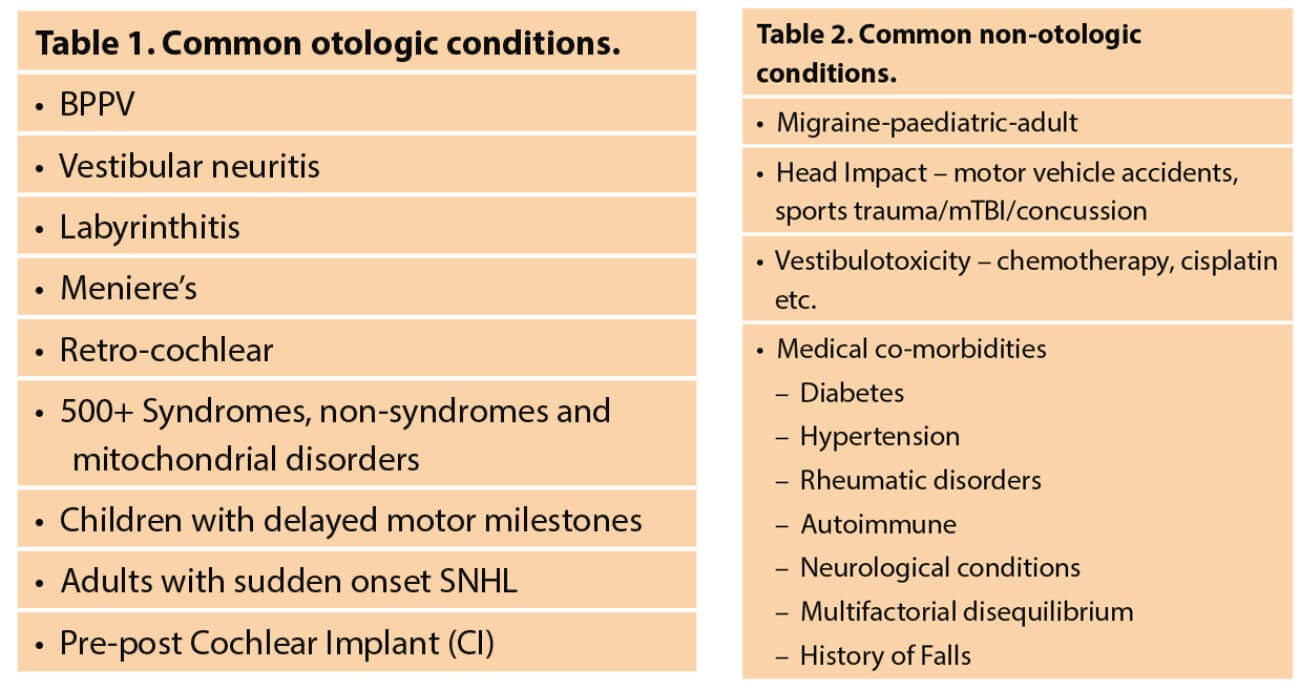
Equilibrium dysfunction is well documented across the lifespan, from congenital to age-onset. The most common otologic conditions and candidates for evaluation are outlined in Table 1. There are also many non-otologic causes of equilibrium related to numerous comorbidities as shown in Table 2. Therefore, it is critically important for all healthcare practitioners focused on the evaluation and management of individuals with equilibrium dysfunction to also be aware that most are not candidates for pharmacological or surgical intervention.
The majority will require management with non-medical treatments such as canalith repositioning, vestibular rehabilitation therapy (VRT), balance retraining therapy (BRT), fall risk management with fall recovery strategies, and activities of daily living, to allow safe ageing in place. For those experiencing a mild traumatic brain injury (mTBI) or concussion, secondary to a head trauma from a fall, sports or other impact trauma, there will need to be clinical decisions on the patient’s ability to return to activities (RTA) and return to play (RTP) post mTBI and concussion. This typically requires a team approach of diagnosticians and rehabilitation specialists.
Medical triage and evaluation protocols
Once a patient has sought care from their physician, walk-in clinic or hospital emergency department, they are often referred to a ‘balance specialist’. Depending on what the provisional diagnosis may be, the referral could be to any one of those practitioners, who by specialty, reputation, or success, have become recognised as the ‘expert’ in their community.
The availability of well-trained professionals and the technology to evaluate patients will determine which clinical pathways and testing protocols are engaged. In locales where minimum technology is available, the use of bedside protocols may be the norm. Many facilities around the world do not have access to VNG, vHIT or rotary chair testing, so more modest protocols, which still retain good sensitivity, should be utilised. Often, even these modest protocols will provide excellent information to assist diagnosticians and rehabilitation specialists in the proper triage and treatment. Both bedside and range of technologies and their respective pros and cons are shown in Table 3.
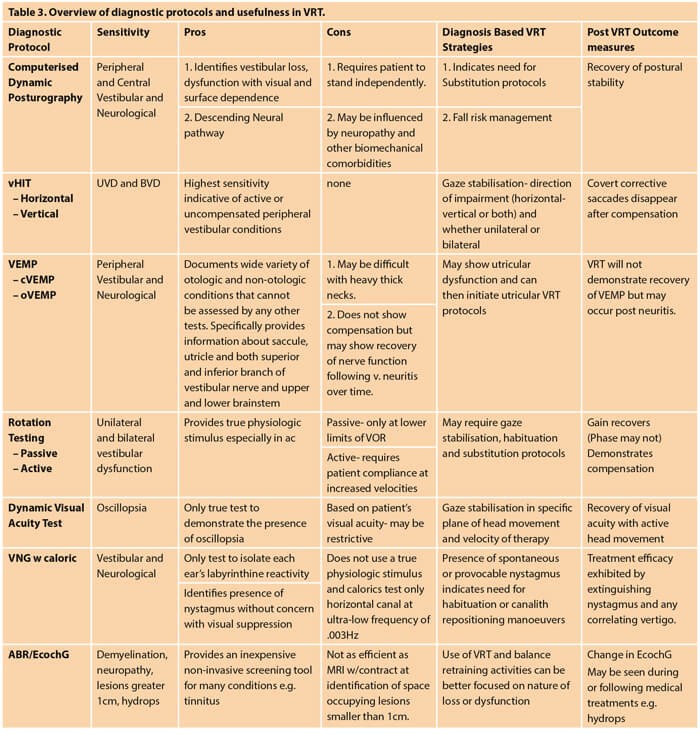
The goal is to accurately determine what is the nature of the involvement and best management strategies for the individual patient, once any necessary immediate medical care has been rendered. Most practitioners, regardless of technology limitations, should be able to provide at least some basic screening protocols e.g. head impulse test, modified Hallpike, or dynamic visual acuity testing, from which patients may then be triaged to those practitioners with specialty qualifications and experience as needed.
“The goal is to not use a ‘one-size-fits-all’ approach to therapy, but rather an individualised or prescriptive approach based on the functional impairments from the dysfunction”
Since 1992, the American Institute of Balance (AIB) has evaluated over 150,000 patients and treated over 15,000 BPPV patients with canalith repositioning. An interdisciplinary approach is encouraged and utilised for the majority of patients. The Institute accepts patients only through physician referral.
Once a preliminary diagnosis has been established, a comprehensive neuro-diagnostic evaluation is conducted based on the nature of the patient’s history and symptoms which may include all or some of the following: audiologic studies, postural stability testing, computerised dynamic posturography (CDP), vHIT, VEMP, ABR, EChoG, rotary chair, dynamic visual acuity testing. Once the patient has been cleared medically and their functional impairment(s) have been established through the test results, e.g. oscillopsia at 2 cps horizontal head movement, we may proceed with the appropriate non-medical management.

Figure 1. Basic VRT and balance therapy.

Figure 2. Advanced technology VRT with virtual reality.
Diagnosis based strategies: producing and measuring successful outcomes
The use of ‘diagnosis based strategies’ which focuss on patient-centred clinical pathways, was first recommended by Richard Gans in 1996. The goal is to not use a ‘one-size-fits-all’ approach to therapy, but rather an individualised or prescriptive approach based on the functional impairments from the dysfunction e.g. positional vertigo, oscillopsia, vestibular recruitment or visual/surface dependence. This ensures the shortest course of treatment and successful measurable outcomes in extinguishing the symptoms, as well as enhancing everyday functioning to normal. As examples, shown in Figures 1 and 2, therapy protocols for VRT may range from postural stabilisation on static and dynamic surfaces, to the use of VRT with advanced technology with full immersion virtual reality. The goal is always to produce the most efficacious treatment in the shortest amount of time, allowing the patient to return to a full, active and safe lifestyle.
Conclusions
It is estimated that dizziness, vertigo, falls and/or mTBI effects over 15%, or more than 1.2 billion individuals worldwide every year. Although many individuals will enjoy spontaneous resolution of their symptoms, most will not. This results in untold costs in medical visits, hospitalisations, loss of worker productivity and human suffering. Practitioners in otolaryngology, audiology, neurology and physiotherapy have the opportunity to work collaboratively in the early intervention, evaluation and treatment of this population. Working together as an interdisciplinary team assures patients the best possibility for recovery and return to normal function and an improved quality of life.
References
1. Gans RE. Vestibular Rehabilitation Therapy. In: Dispenza F, De Stefano A, (Eds.). Textbook of Vertigo Diagnosis and Management. London, UK; Jaypee Brothers Medical Publishers; 2013.
2. Gans RE. Vestibular Rehabilitative Therapy. In Katz, J, (Ed.). Handbook of Clinical Audiology, 7th Edition. Philadelphia, PA, USA; Wolters, Kluwer Health; 2015.
3. Chua K, Gans R, Spinks S. Demographic and clinical characteristics of BPPV patients: a retrospective large cohort study of 1599 patients. Journal of Otolaryngology-ENT Research 2020;12(1):20-30.
4. Roberts RA, Bittel SN, Gans RE. Positional Nystagmus in Patients Evaluated for Dizziness and Imbalance. Advances in Otolaryngology 2016;1-10.
5. Roberts RA, Abrams H, Sembach MK, et.al. Utility Measures of Health-Related Quality of Life in Patients Treated for Benign Paroxysmal Positional Vertigo. Ear and Hearing 2009;30:369-76.
Declaration of Competing Interests: Drs Gans and Rutherford are senior staff at The American Institute of Balance, which organises certification workshops for physicians, audiologists, physical and occupational therapists in vestibular and balance science, worldwide.






