Cochlear Implantation (CI) in children with single-sided deafness (SSD) is a controversial treatment option. Profs Karen Gordon, Papsin and Cushing discuss the rationale and early findings on the relative success of achieving binaural hearing for SSD with CI.
If you’d asked us 10 years ago whether cochlear implants could be used by children who heard with one normal hearing ear, we might have answered skeptically. At that time, we were investigating deficits related to the limited representation of sound frequencies provided by the cochlear implant in children, including challenges for hearing musical cues and for recognising emotion in speech. Simulations heard by individuals with normal hearing highlighted the distortions created by cochlear implants.
How then could we expect to combine cochlear implant hearing in one ear with acoustic hearing in the other (bimodal hearing)? Wouldn’t the sound from the cochlear implant interfere with or distract the better hearing ear? Presently, those concerns have given way in light of our increased understanding of the deficits associated with asymmetric and unilateral hearing loss when it occurs in development. As a halfway point, we’ve learned that children can benefit from hearing with amplified acoustic sound through a hearing aid in one ear and electrical hearing through a cochlear implant in the other ear. With this new information in mind, it is time to evaluate the use of a cochlear implant in children who have severe to profound hearing loss in one ear and who listen without the need for a hearing device in their other ear.
Why treat children with single-sided deafness?
The most obvious impairment of single-sided deafness is the loss of binaural hearing and, thus, impaired localisation of sound in space [1]. For a long time, this was felt to be an annoyance, but not critical to development. It is now clear, however, that the loss of spatial hearing in early childhood is associated with slower language acquisition, risk of poor academic performance, increased listening effort, and poorer quality of life relative to peers with normal hearing [2,3]. These deficits do not demonstrate causality due to poor binaural hearing but it is worthwhile thinking about why such a specific auditory impairment in sound localisation might lead to global challenges in children. One possibility is that spatial hearing is more essential to children’s function than previously thought. The locations of different sound sources are used to distinguish one from another and children are likely to use these cues throughout their day. Children are rarely alone in a quiet environment and, indeed, should be surrounded by family and peers for safety, interaction, and learning. These environments, like the one shown in Figure 1, are typically dynamic and require the child to hear surrounding sounds from all directions (we call this the ‘child’s cocktail party’).

Figure 1. A child with unilateral hearing loss in a typical ‘child’s cocktail party’ like the game above will have difficulty identifying the location of each speaker and will have trouble hearing the children on her impaired side. (Image from www.dreamstime.com)
Without spatial hearing, a child with unilateral hearing loss (shown in the centre in Figure 1) has to focus on other acoustic features that make each sound distinct; this becomes increasingly difficult as the number of speakers and other sounds increases, particularly when the target sound is closer to the impaired ear. This head shadow effect is illustrated in Figure 1. Children with unilateral hearing loss show abnormal recruitment and connectivity with cortical areas involved in attention, executive memory and cognition, suggesting that they are working hard to hear [3]. Along with their hearing challenges, we have learned that vestibular and balance problems are also prevalent in children with unilateral hearing loss [4]. It is thus reasonable to suspect that deficits in spatial hearing and vestibular/balance function lead to other developmental challenges in children with unilateral hearing loss.
Why use cochlear implants to treat single-sided deafness?
Cochlear implants are considered the most effective way to provide an ear with severe to profound deafness with access to sound. Why then might this treatment be of concern in children with single-sided deafness? As discussed above, there were initial fears that the electrical hearing would interfere with the hearing from the better ear. In addition, the usual risks of cochlear implant surgery must be considered prior to consenting to this treatment.
These risks have become minimal but are amplified by the elective and currently experimental application of implantation in this setting. There is also considerable follow-up required after surgery which could ‘medicalise’ children with unilateral hearing loss. It is for these reasons that many families of children with unilateral deafness who we consider candidates for cochlear implantation choose not to pursue this option. It is important to note here that between one third and one half of children with single-sided deafness are not candidates for cochlear implantation due to hypoplasia of the auditory nerve.
On the other hand, cochlear implantation could prevent the brain changes we see in children who have single-sided access to sound. In such cases, binaural hearing will be compromised by the development of an aural preference for the better ear [2]. Bone anchored hearing aids and CROS hearing aids have been considered to reduce the head shadow effect but rely on further use of the preferred ear and do not provide binaural/spatial hearing [2]. Thus, a limited duration of deafness in the impaired ear is a key criteria for cochlear implantation in children with single-sided deafness by our multidisciplinary team.
“It may be particularly important to reduce aural preference and reliance on the better ear by preserving bilateral hearing in children with congenital cytomegalovirus.”
Other factors important for candidacy are: medical suitability for surgery; speech and language abilities; overall development, social and learning abilities; reasonable expectations of the child and/or caregiver; family support and structure and; availability of educational support services. We have also begun to think about the future of the hearing ear. Many children with single-sided deafness carry a diagnosis of congenital cytomegalovirus, often detected by PCR analysis of their neonatal blood spot. These children are at great risk for progressive hearing loss in their better ear. With this in mind, it may be particularly important to reduce aural preference and reliance on the better ear by preserving bilateral hearing in children with congenital cytomegalovirus.
What are the outcomes of cochlear implantation in children with single-sided deafness?
The overarching aim of cochlear implants in children with single-sided deafness is to promote binaural hearing in an effort to reduce their listening challenges and support overall development. The aims are being assessed by a number of research groups. Our group is presently following almost 30 children with single-sided deafness who received a cochlear implant using the candidacy criteria indicated above, including limited duration of deafness. Thus far, we have reported that most use their devices consistently, suggesting perceived benefits of wearing the implant. Also encouraging are data from the first group of infants which revealed that cortical representation from both ears was established by six months of cochlear implant use (see Figure 2).
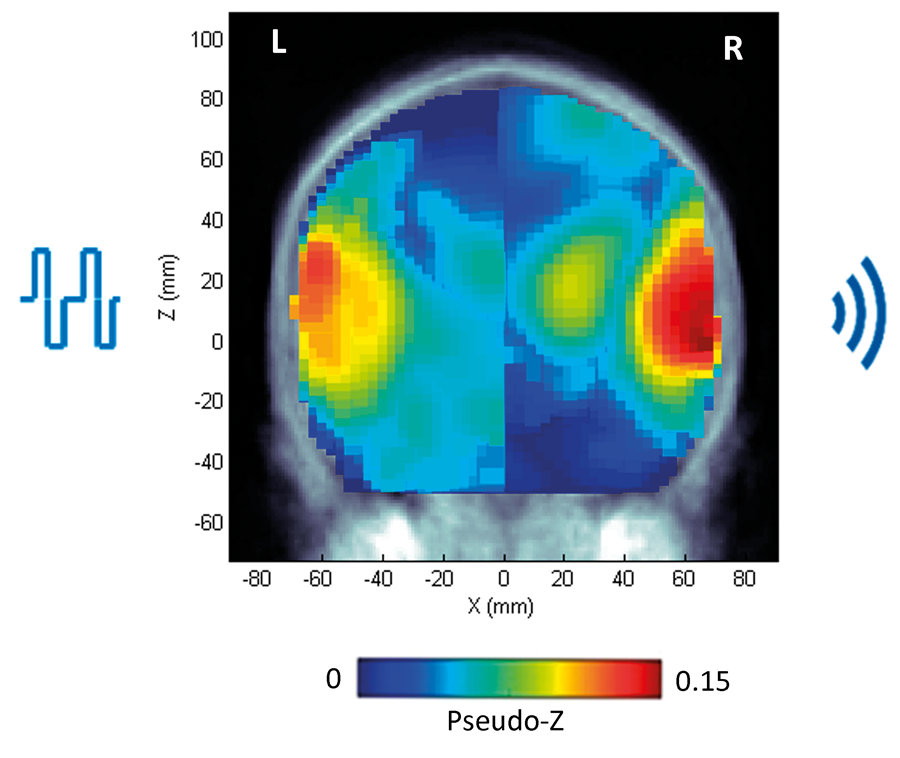
Figure 2. Young children with single-sided deafness were implanted in the impaired right ear. Cortical representation from the right ear was established by three to six months of cochlear implant use. Electrical stimulation from the cochlear implant and acoustic sound in the normal hearing ear stimulated both left and right auditory cortices, as shown in the coronal view of cortical sources above [5].
Based on outcomes of cochlear implantation in adults with single-sided deafness, we also expect that sound localisation will improve. Parents have also provided helpful comments. For example, from a mother of a child with single-sided deafness (and congenital cytomegalovirus) who was implanted as an infant:
“I know this isn’t scientific at all, but ‘C’ is flourishing. At her most recent audiogram, the CI works as well as her hearing ear. She wears it all the time, asks for it and it helps improve her balance. Every day we are grateful she was able to be a part of your work. ‘C’ attends a daycare with 24 three to five year-olds - so it’s noisy :) And she has no problems hearing and her language continues to blow us away.”
Summary
If you ask us now about cochlear implantation in children with single-sided deafness, we are optimistic but practical. This may not be a solution that all children will want or can make use of and it is unlikely that normal access to binaural/spatial hearing will be provided. On the other hand, we are already seeing evidence that hearing in both ears can be preserved and that this hearing can provide benefits over the clear deficits of listening with one ear alone. We look forward to revisiting this question again in the future as we continue to learn from these children.
References
1. Litovsky RY, Gordon K. Bilateral cochlear implants in children: Effects of auditory experience and deprivation on auditory perception. Hear Res 2016;338:76-87.
2. Gordon K, Henkin Y, Kral A. Asymmetric Hearing During Development: The Aural Preference Syndrome and Treatment Options. Pediatrics 2015;136(1):141-53.
3. van Wieringen A, Boudewyns A, Sangen A, et al. Unilateral congenital hearing loss in children: Challenges and potentials. Hear Res 2018;1(10).
4. Sokolov M, Gordon KA, Polonenko M, et al. Vestibular and balance function is often impaired in children with profound unilateral sensorineural hearing loss. Hear Res 2018;3(32).
5. Polonenko MJ, Gordon KA, Cushing SL, Papsin BC. Cortical organization restored by cochlear implantation in young children with single-sided deafness. Sci Rep 2017;7(1):16900.
Declaration of Competing Interests:
The authors have received funding from Cochlear Corp. KG was a consultant for Advanced Bionics; SC is on the speakers’ bureau for Interacoustics Inc.







