Explore the innovative minimum stimulus strategy (MSS) for diagnosing benign paroxysmal positional vertigo (BPPV), enhancing accuracy while minimising patient discomfort.
Benign paroxysmal positional vertigo (BPPV) is a common vestibular disorder where canalolithiasis or cupulolithiasis causes sudden episodes of vertigo, triggered by head movements. The diagnostic workup for BPPV focuses on identifying the affected ear, canal and the type of positional nystagmus that results either from the free-floating debris moving in the canals (canalolithiasis) or from persistent cupular bending due to otoconia overloading the cupula itself (cupulolithiasis). This article explores a novel approach to simplify and improve diagnostic efficiency for BPPV, known as the minimum stimulus strategy (MSS).
Overview of the diagnostic manoeuvres for BPPV
Diagnostic manoeuvres are critical in confirming BPPV, particularly through inducing positional nystagmus which is a key indicator of the condition.
The most common diagnostic tests include the Dix-Hallpike manoeuvre and the supine head roll test (sHRT). These tests rely on gravity as well as inertial and centrifugal forces, briskly moving both the head and trunk of the patient, either from a sitting to supine position with the head turned toward the explored ear (Dix Hallpike) or turning 180° from one side to the other with the patient supine (sHRT). While the first manoeuvre is used for the diagnosis of posterior semicircular canal (PSC) BPPV, the sHRT is used to detect otoconia in the ampullary (apogeotropic variant) or non-ampullary arm (geotropic variant) in horizontal semicircular canal (HSC) BPPV. In PSC-BPPV, the paroxysmal positional nystagmus is typically vertical / torsional with up-beating / ipsilesional components and the affected side is where the positional nystagmus is elicited.
"The key component of MSS is the upright BPPV protocol (UBP), a technique that involves keeping the patient seated during diagnostic tests"
In HSC-BPPV, the positional nystagmus is purely horizontal on both sides and changes direction based on where the otoliths are located within the canal. Geotropic HSC-BPPV is characterised by paroxysmal nystagmus that beats bilaterally toward the ground at the sHRT and the affected side is where nystagmus is stronger, while apogeotropic HSC-BPPV shows nystagmus that beats bilaterally away from the ground and is stronger on the unaffected side [1]. However, these tests can be challenging in patients with severe autonomic symptoms, especially during the acute ‘active period’ of BPPV, which is typically the first 24 to 72 hours of symptom onset.
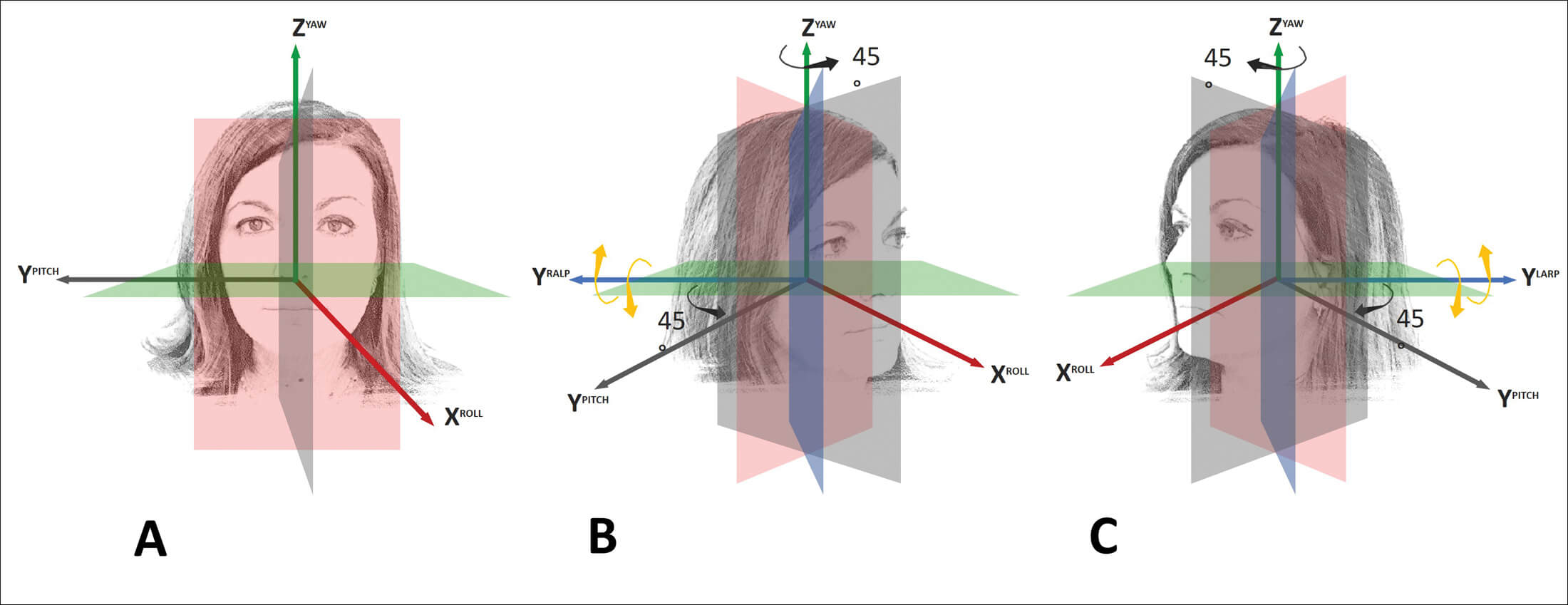
Figure 1: A) Schematic overview of head rotations along the roll, pitch and yaw planes rotating around the X, Y and Z axes, respectively; B) Right anterior–left posterior (RALP); and C) Left anterior–right posterior (LARP) canal planes with corresponding head rotations around the YRALP / YLARP axes, respectively.
The MSS addresses these issues by minimising the number of diagnostic movements, thereby reducing patient discomfort while still ensuring accurate diagnosis. The key component of MSS is the upright BPPV protocol (UBP), a technique that involves keeping the patient seated during diagnostic tests. By using gravity through gentle head movements, this strategy effectively displaces canaliths and induces nystagmus, making it easier to identify the affected canal without requiring the patient to lie down. According to the axis around which the head is rotated (X, Y and Z axes), each test in UBP has been appropriately labelled based on the spatial plane (roll, pitch and yaw plane, respectively – see Figure 1a). Furthermore, two additional planes – left anterior–right posterior (LARP) and right anterior–left posterior (RALP) – aligned with each pair of vertical canals can be used considering the spatial orientation of the vertical canals (Figure 1b,c) [2].
The UBP procedure
The UBP is a structured series of diagnostic tests performed while the patient is seated. It starts with an evaluation of pseudo-spontaneous nystagmus (PSN) in the primary gaze position which may indicate, if detectable, a canalo / cupulolithiasis in the HSC as it beats towards the healthy side in geotropic variants and towards the affected side in apogeotropic variants / cupulolithiasis. This is due to the natural 30° anterior-inclination of the HSC with respect to the horizontal plane, allowing slow ampullopetal / ampullofugal otoconial shifts within the affected canal arm [3].
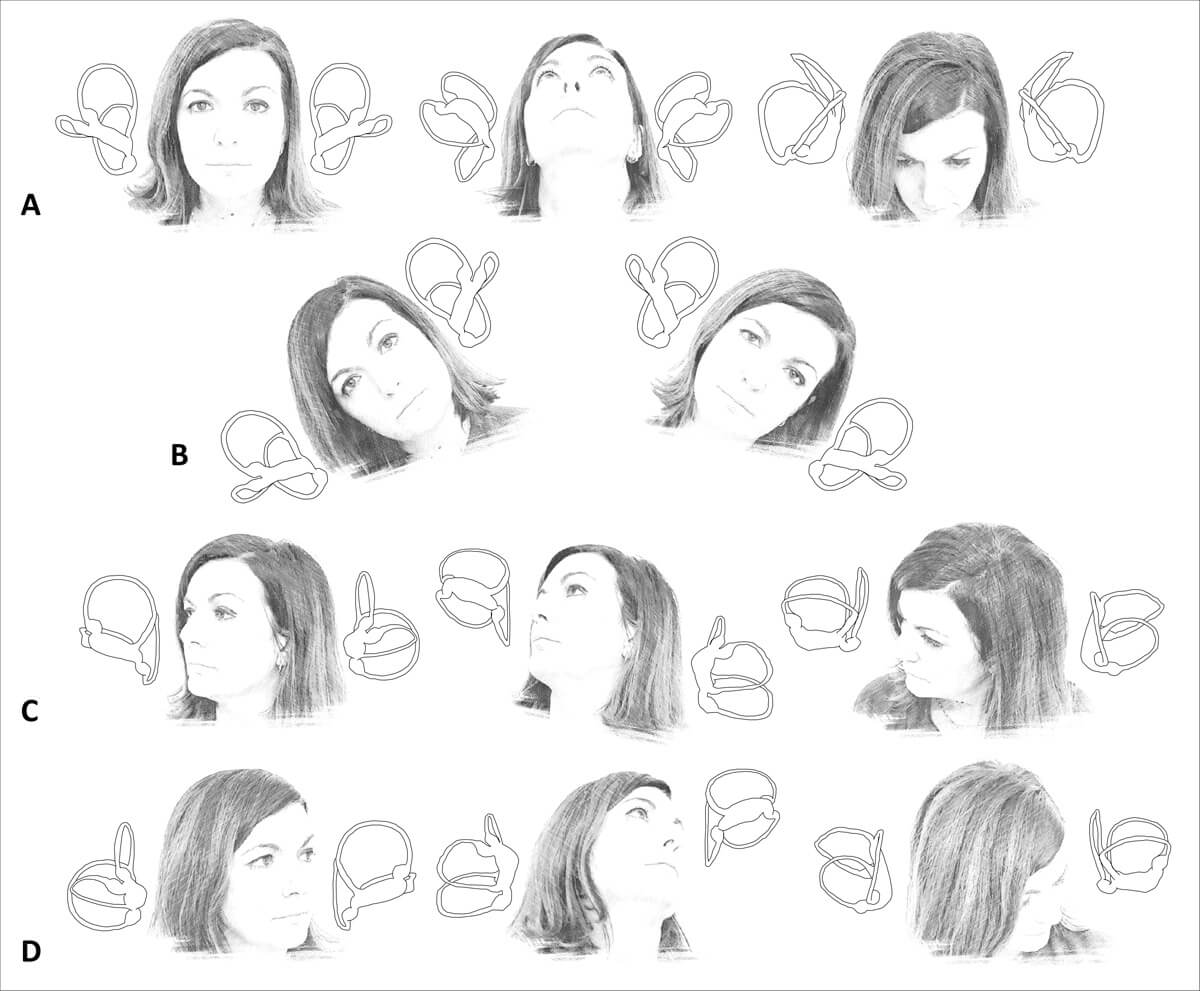
Figure 2: Upright BPPV protocol (UBP). A) Upright head pitch test (uHPT): the patient’s head is bent backward and forward around the Y (inter-aural) axis and along the pitch plane. B) Upright head roll test (uHRT): the patient’s head is tilted rightward and leftward around the X (naso-occipital) axis and along the roll plane. C) uRALP/uLARP test: the patient’s head is bent backward and forward along the RALP and LARP planes and around the YRALP / YLARP axes, respectively.
The following test in the UBP is the upright head pitch test (uHPT), also known as the ‘bow and lean test’ (Figure 2a). During this test, the patient’s head is gently tilted forward 60° and then backward 30° along the pitch plane and around the Y-axis. The presence of nystagmus at the uHPT, particularly its direction and characteristics, is central to diagnosing the affected canal, as the nystagmus response during these movements helps identify whether horizontal or vertical canal involvement is present. In fact, in HSC-BPPV the uHPT changes the direction of the previously identified PSN while, in the absence of a PSN, it may cause horizontal nystagmus that reverses based on the head-bending angle. On the other hand, the uHPT may cause vertical / torsional nystagmus addressing towards a PSC-BPPV [3].
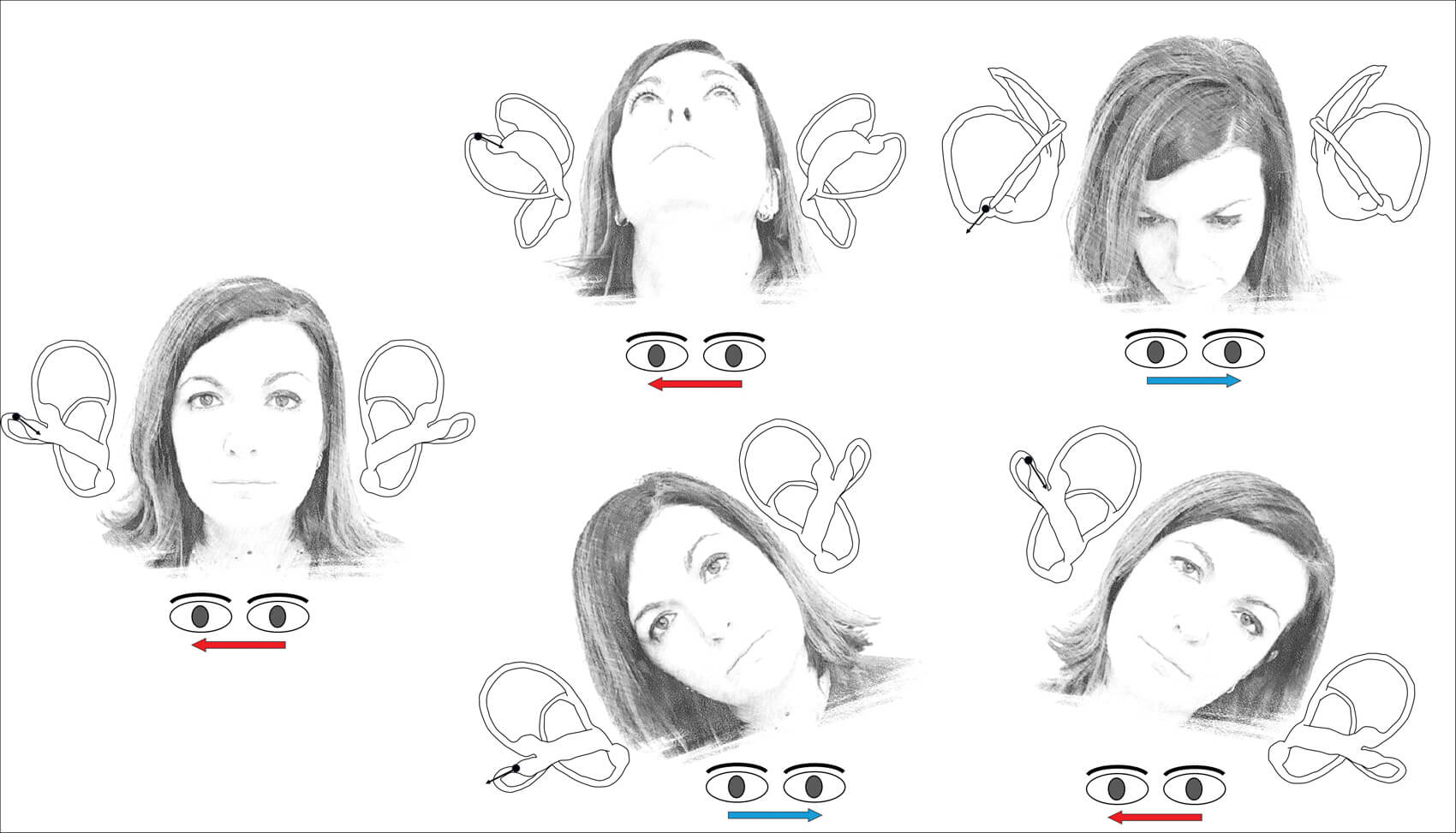
Figure 3: UBP for right apogeotropic HSC-BPPV. Arrows within the canal represent the direction of endolymphatic flows, whereas arrows beneath the eyes represent the direction of the nystagmus.
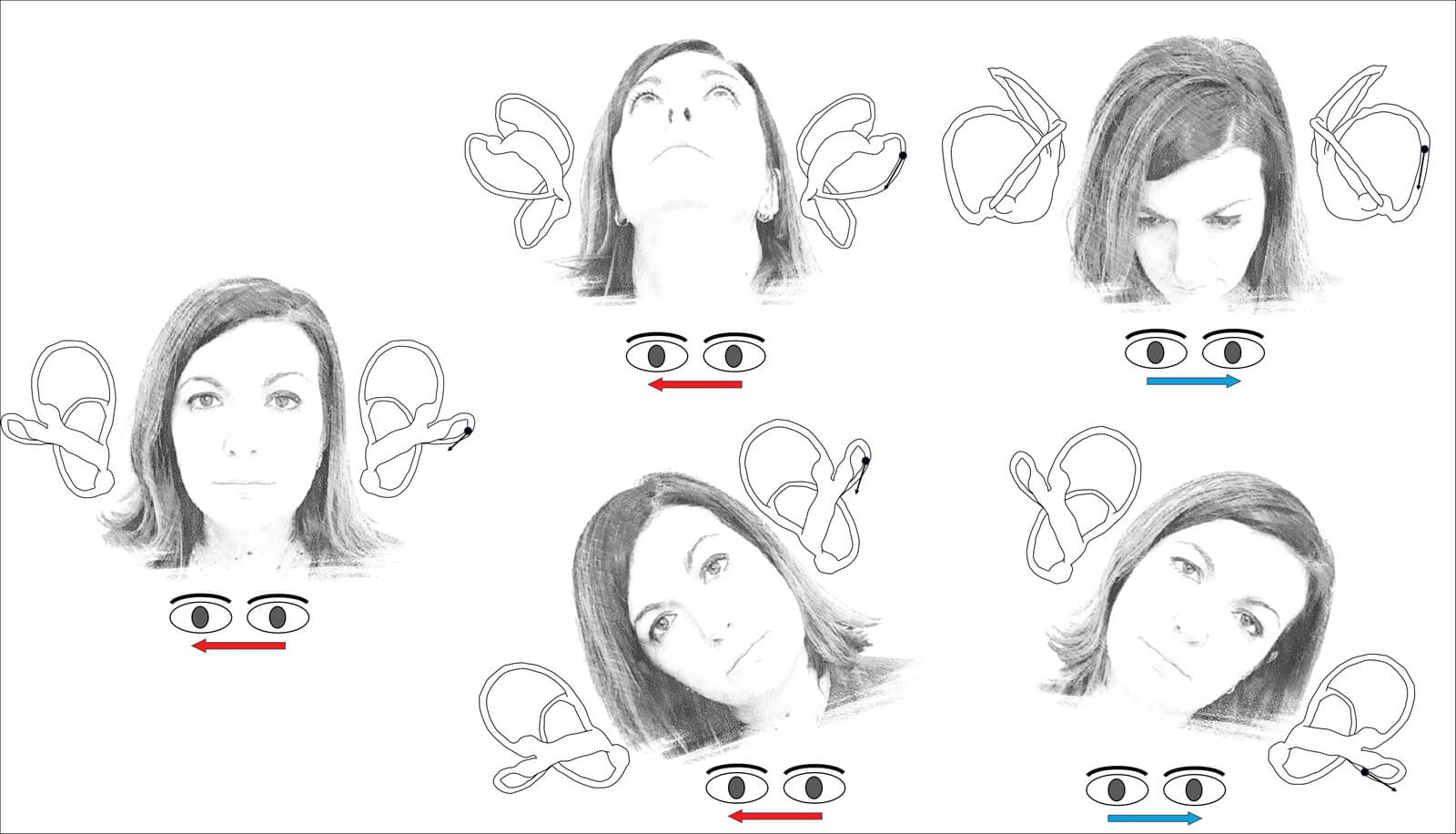
Figure 4: UBP for left geotropic HSC-BPPV. Arrows within the canal represent the direction of endolymphatic flows, whereas arrows beneath the eyes represent the direction of the nystagmus.
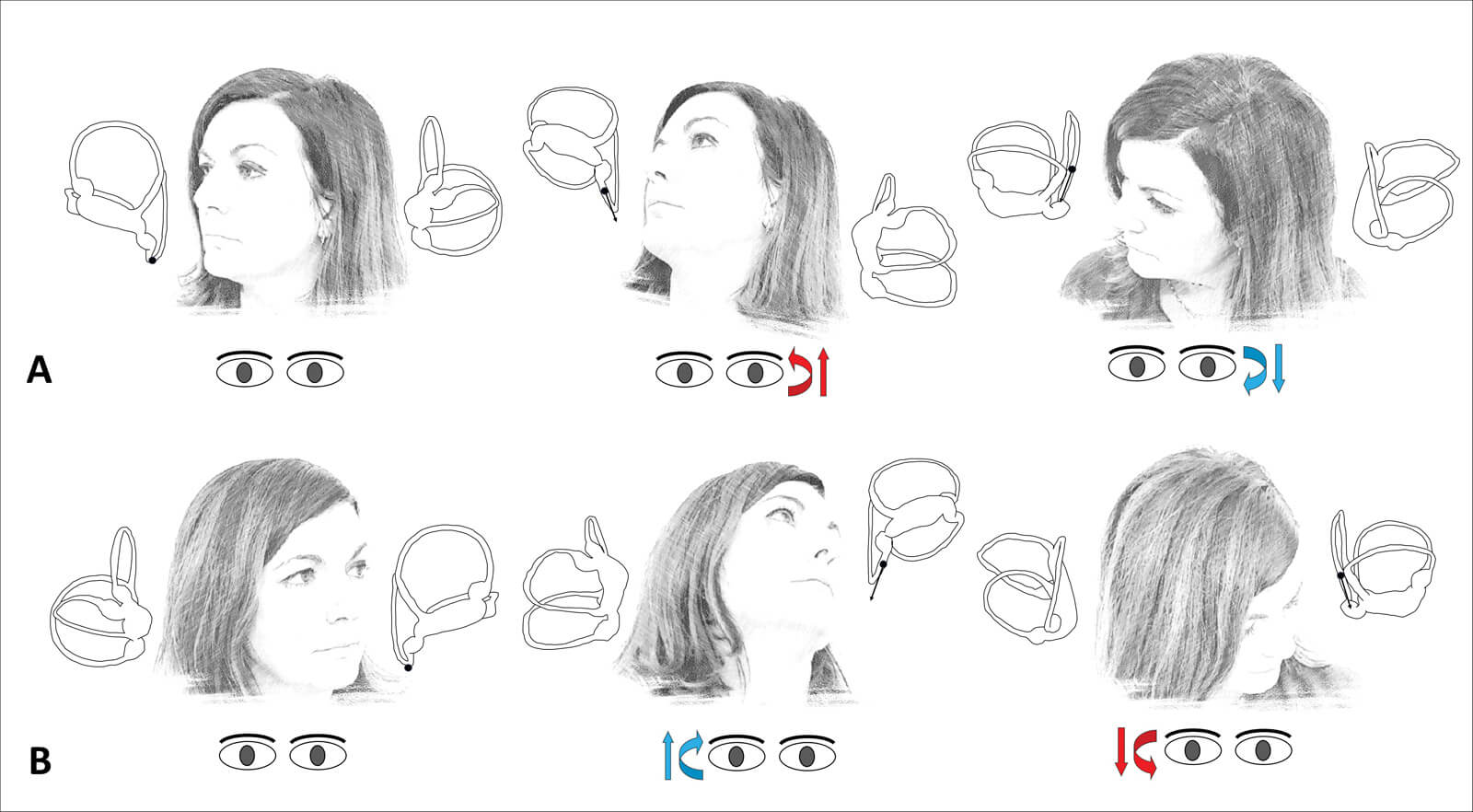
Figure 5: A) uLARP test for right PSC-BPPV. b) uRALP test for left PSC-BPPV. The arrows within the canal represent the direction of endolymphatic flows, whereas the arrows beneath the eyes represent the direction of the nystagmus.
If horizontal PSN is detected and / or horizontal nystagmus is evoked by the uHPT, the next test is the upright head roll test (uHRT) (Figure 2b). The patient’s head is tilted 30° to the left and the to the right, rotating around the X-axis along the roll plane, to identify geotropic or apogeotropic horizontal nystagmus. These upright tests can diagnose more than 90% of HSC-BPPV cases, making them an effective first-line diagnostic approach. If the results are inconclusive, additional tests such as the sitting-supine positioning test (SSPT) and the sHRT should be performed [4]. Figure 3 shows the expected eye movements in case of right HSC-BPPV in apogeotropic form and Figure 4 shows the expected eye movements in case of left HSC-BPPV in geotropic form.
In PSC-BPPV, nystagmus is typically up-beating and torsional towards the affected ear in backward uHPT (when the head is extended), as otoconia floats away from the ampulla, exciting the PSC afferents. In forward uHPT (when the head is flexed), it is down-beating with opposite torsional components due to an ampullopetal (inhibitory) endolymphatic flow generated by otoliths. For PSC-BPPV, the MSS approach enhances the diagnostic sensitivity by aligning the head with the plane of the affected canal using the upright LARP and upright RALP tests, depending on whether the right or left PSC is affected, respectively. The head rotates around two new Y axes (the YRALP / YLARP axes) and along the RALP and LARP planes (Figure 2c). These manoeuvres improve the diagnostic accuracy, particularly in cases where the uHPT alone is not conclusive.
"MSS offers a more patient-friendly approach that still ensures high diagnostic accuracy"
Following the identification of the affected canal, the ipsilateral Dix-Hallpike or Semont procedures can be used to confirm the correct diagnosis before the therapeutic manoeuvres are carried out. The same manoeuvres should be performed in case none of the aforementioned upright tests led to detectable nystagmus [5]. Figure 5 shows the expected eye movements in case of right and left PSC-BPPV.
This article highlights that MSS using the UBP procedure can provide a quicker, less invasive way to diagnose BPPV and initiate treatment, while traditional diagnostic tests like the Dix-Hallpike manoeuvre and the sHRT are still important in cases with inconclusive and uncertain data. Additionally, the use of video-Frenzel goggles during testing ensures continuous monitoring of nystagmus, providing real-time feedback to the clinician.
Conclusion
The minimum stimulus strategy, particularly the upright BPPV protocol, represents a significant advancement in the diagnosis of BPPV. By reducing the need for unpleasant supine tests and limiting the number of diagnostic manoeuvres, MSS offers a more patient-friendly approach that still ensures high diagnostic accuracy. The UBP procedure has been shown to accurately diagnose the affected ear and canal in the majority of cases, particularly in the first days from the onset of symptoms when debris is thought to be still aggregated in a clot that could be easily moved with gentle head bending. While it can be more challenging in cases of central vestibular disorders or unusual clinical presentations (like PSC-cupulolithiasis, BPPV involving the anterior canal and apogeotropic variants of PSC-BPPV), MSS remains a valuable tool for diagnosing and treating BPPV quickly and effectively. In summary, the UBP procedure simplifies the diagnostic process, reduces patient discomfort, and speeds up the initiation of treatment. Its application in clinical practice holds great promise in improving the overall management of BPPV in acute patients. However, for cases where the MSS is not sufficient, traditional supine positioning tests should be used as a secondary approach to confirm the diagnosis.
References
1. Asprella Libonati G. Benign Paroxysmal Positional Vertigo and Positional Vertigo Variants. Int J Otorhinolaryngol Clin 2012;4(1):25–40.
2. Asprella Libonati G, Martellucci S, Castellucci A, Malara P. Minimum Stimulus Strategy: A step-by-step diagnostic approach to BPPV. J Neurol Sci 2022;434:120158.
3. Asprella Libonati G. Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital 2008;28(2):73–8.
4. Martellucci S, Malara P, Castellucci A, et al. Upright BPPV protocol: feasibility of a new diagnostic paradigm for lateral semicircular canal benign paroxysmal positional vertigo compared to standard diagnostic manoeuvres. Front Neurol 2020;11:578305.
5. Martellucci S, Castellucci A, Malara P, et al. Is it possible to diagnose Posterior Semicircular Canal BPPV from the sitting position? The role of the Head Pitch Test and the upright tests along the RALP and LARP planes. Am J Otolaryngol 2022;43(4):103474.
Declaration of competing interests: None declared.












