Hearing aid validation requires that speech discrimination be measured, yet there are no validated methods of measuring speech discrimination in infants and toddlers. Prof Uhler describes two related approaches that are showing promise.
Speech discrimination is the gold standard for validating hearing aids in older children and adults. It has been documented in older children that there is a relationship between speech discrimination and expressive language abilities. Yet, there is not a clinical tool for assessing speech discrimination in infants and toddlers.
This gap in knowledge and the potential clinical impact on hearing aid validation and later language outcomes motivates our work. Our research focuses on developing a tool to assess speech discrimination shortly after infants are fit with hearing aids, and we then examine how early speech discrimination relates to later language outcomes.
Background
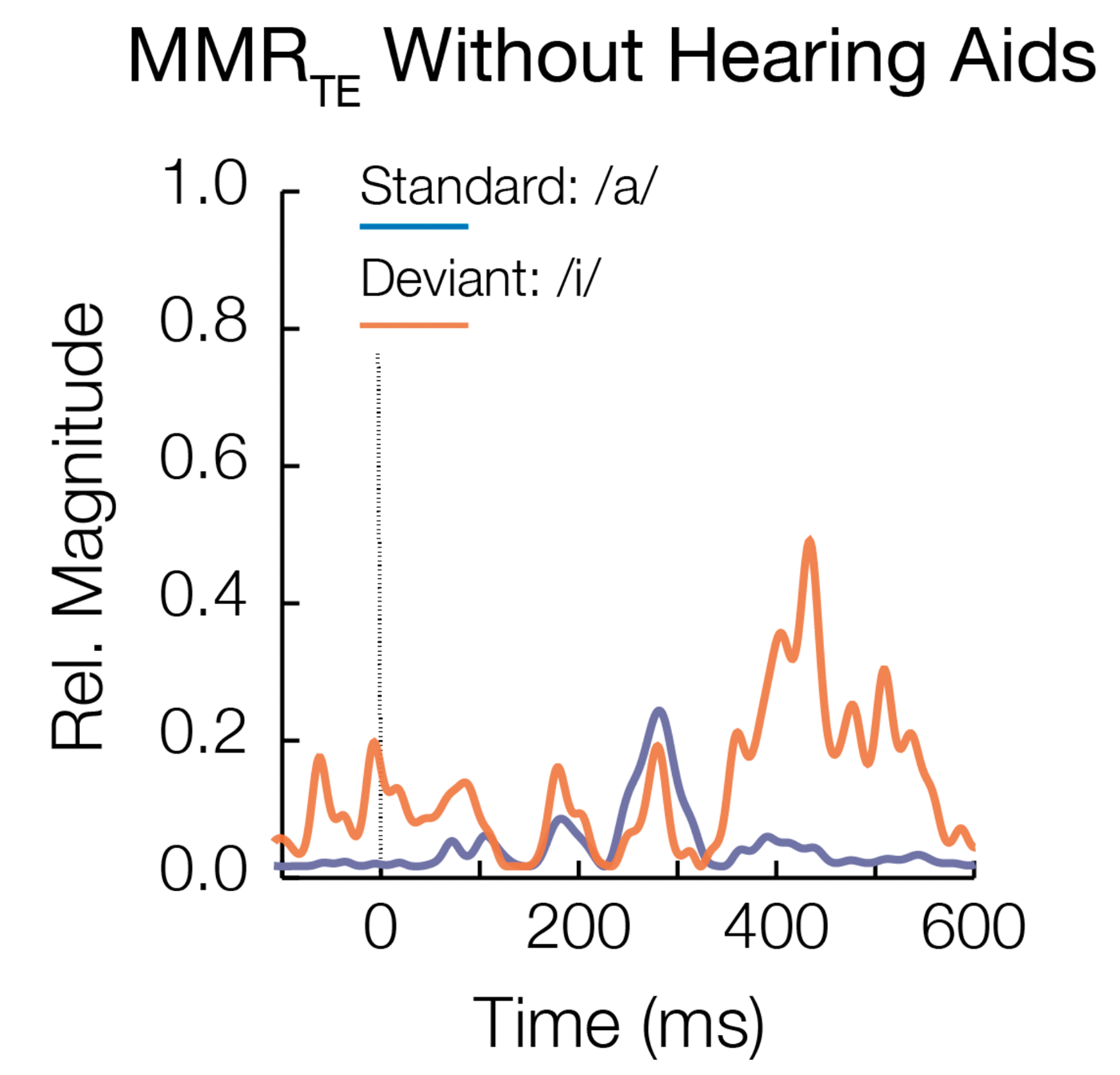
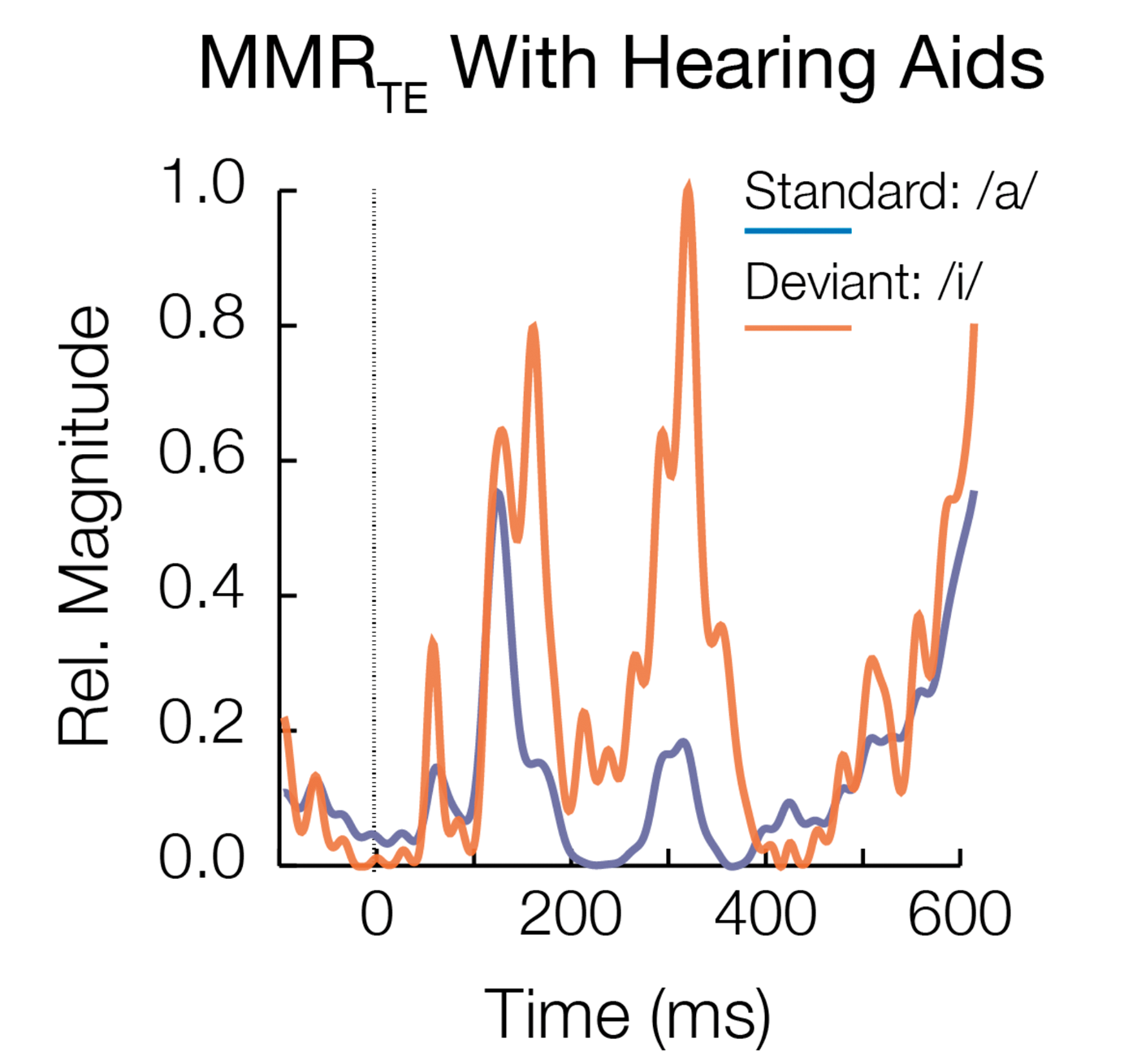
Discrimination of speech sounds is the foundation for development of spoken language. The knowledge gained from being able to objectively document that an infant can discriminate speech while wearing their hearing aids is twofold: 1) over time it could improve paediatric hearing aid fittings and 2) it could improve counselling provided to families. Currently, once hearing aids are fit, there is a wait and see approach to validation, and much of what is used clinically is subjective parent report measures [1]. The use of an objective measure of speech discrimination may increase parental understanding of their child’s hearing loss and the importance of hearing aid use. Specifically, if a parent can see differences in how their infant’s brain responds to speech sounds with versus without hearing aids (see Figure 1), it may lead to improved acceptance and hearing aid use.
Figure 1. Aided versus unaided individual results.
Note. Results for an individual subject with hearing loss illustrating response differences without (left) and with (right) hearing aids. The standard stimulus /a/ illustrated in blue was presented 85% of the time and the deviant stimulus /i/ was presented 15% of the time. In the aided condition the response amplitudes are larger and earlier in latency.
It is critical to assess speech discrimination as quickly as possible after a hearing aid fitting.
Assessing speech discrimination in older children and adults in quiet and in noise is commonly done within the first month of a hearing aid fitting. This starkly contrasts to typical clinical standards for infants. This gap is due to the lack of clinically available tools to assess speech discrimination in infants under six months of age. While protocols exist for assessing speech discrimination in the paediatric population in infants ≥7 months of age, clinical acceptance is currently limited. Most commonly, speech discrimination is not assessed until at least two years of age. This delay in evaluation may lead to two years of auditory input that is inaccurately encoded at the level of the auditory cortex. The addition of a validation tool to the test battery allows clinicians to move beyond using audibility towards a determination of the patient’s ability to detect a difference between different audible speech sounds.
“If a parent can see differences in how their infant’s brain responds to speech sounds with versus without hearing aids, it may lead to improved acceptance and hearing aid use.”
It is possible to assess speech discrimination even in very young infants
The execution of newborn hearing screening has been broadly accepted and implemented for over 20 years in the United States and Territories. The impact has led to significantly improved outcomes in children with hearing loss compared to outcomes before newborn hearing screening. This evolution has brought about new challenges to audiologists and ENTs. While gains have been made, significant variability in language outcomes still exist in children with hearing loss well into later childhood. It is possible that poorly fitted hearing aids early in life may contribute to poorer language outcomes later in life [2]. The gap in how to assess speech discrimination and the ability of clinicians to benchmark outcomes leads to challenges in clinician expectations and counselling parents.
Our research has focused on addressing this gap in knowledge by developing a tool to validate hearing aids to ensure infants cannot only detect sound, but also discriminate speech sounds, leading to improved outcomes regarding spoken language. While the use of an auditory evoked measure of speech discrimination is not yet ready for clinical use, we have taken several steps to identify and validate a tool in infants with and without hearing loss. With the aim of clinical utility, all testing is done in sleeping infants and can be completed in a similar amount of time to a diagnostic auditory evoked potential evaluation used to diagnose hearing loss.
“The gap in how to assess speech discrimination and the ability of clinicians to benchmark outcomes leads to challenges in clinician expectations and counselling parents.”
To date, we have used two different paradigms (acoustic change complex; ACC and a modified approach to mismatched response; MMR) to assess infant speech discrimination. These paradigms are non-invasive auditory evoked potential measures that have been evaluated in infants (≤5 months of age) to assess speech discrimination for two different speech contrasts (/ba-da/ and /a-i/). The development of this measure of infant speech discrimination is part of a longitudinal study, examining the relationships between speech discrimination and later language development. Due to the eventual aim of clinical utility, the ideal tool will need to have robust responses within individual sleeping infants and be efficient; we have examined different speech stimuli, different filter settings, and analysis methods (i.e. filter settings, signal averaging versus principal component analysis).
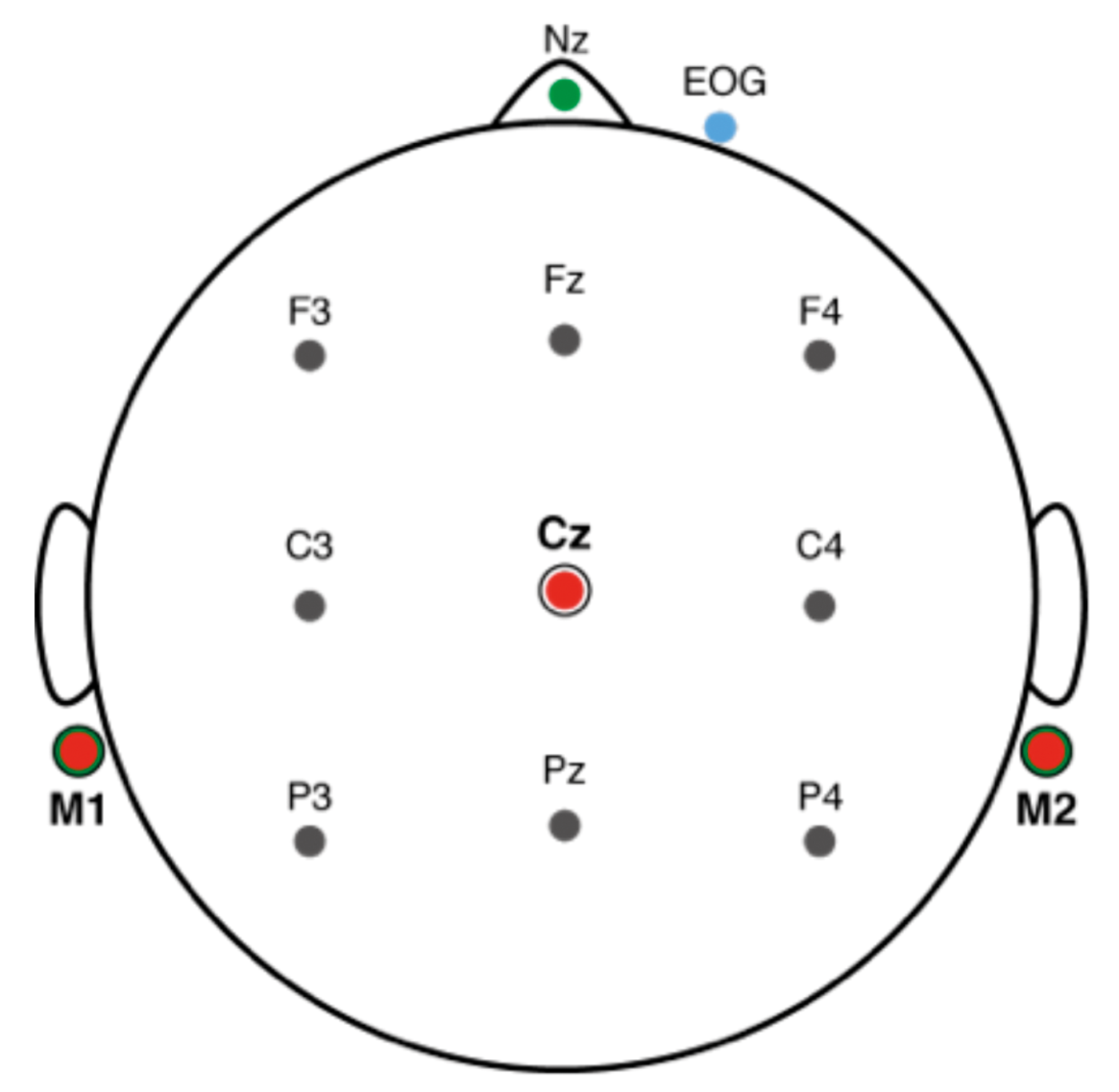
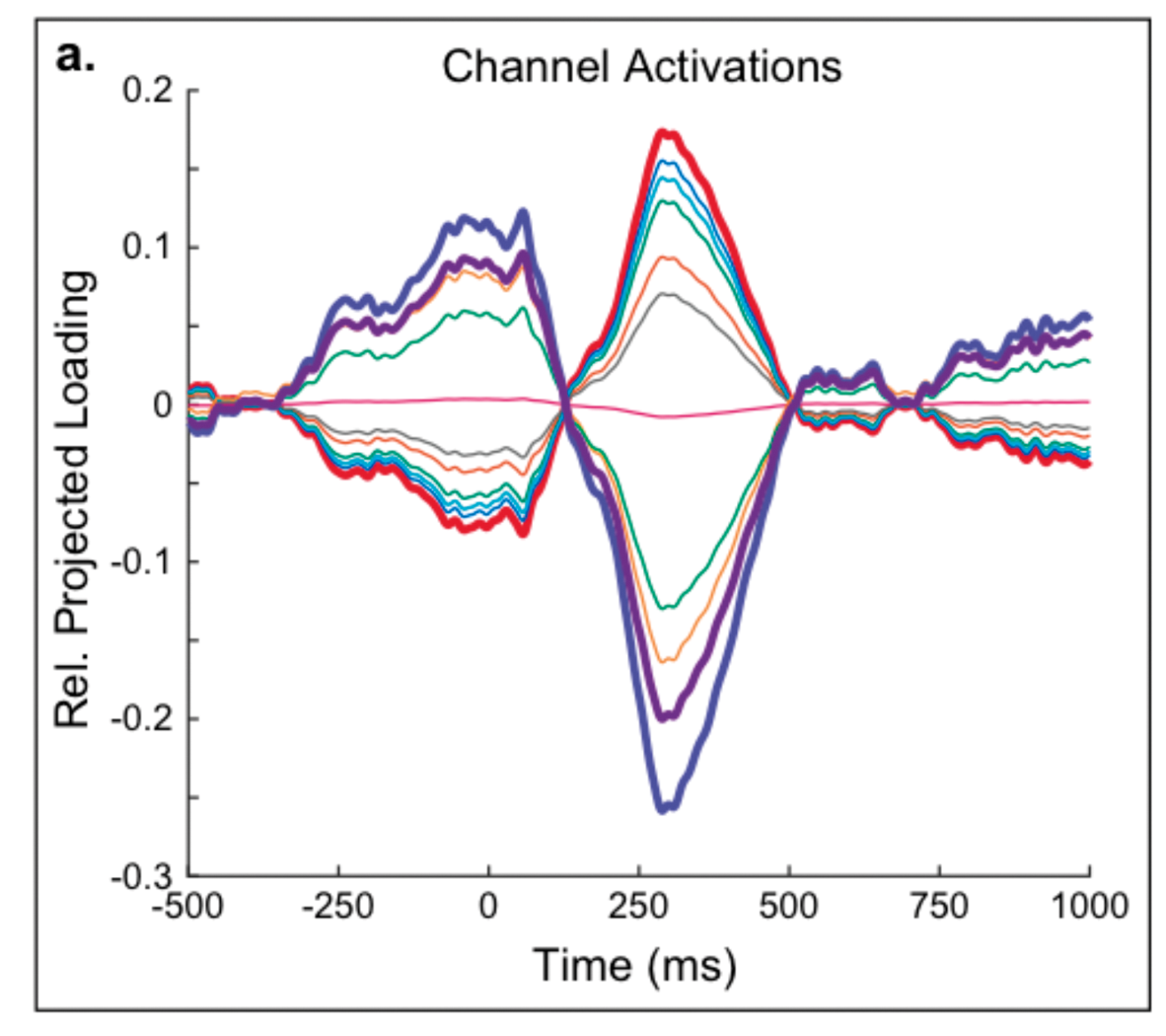
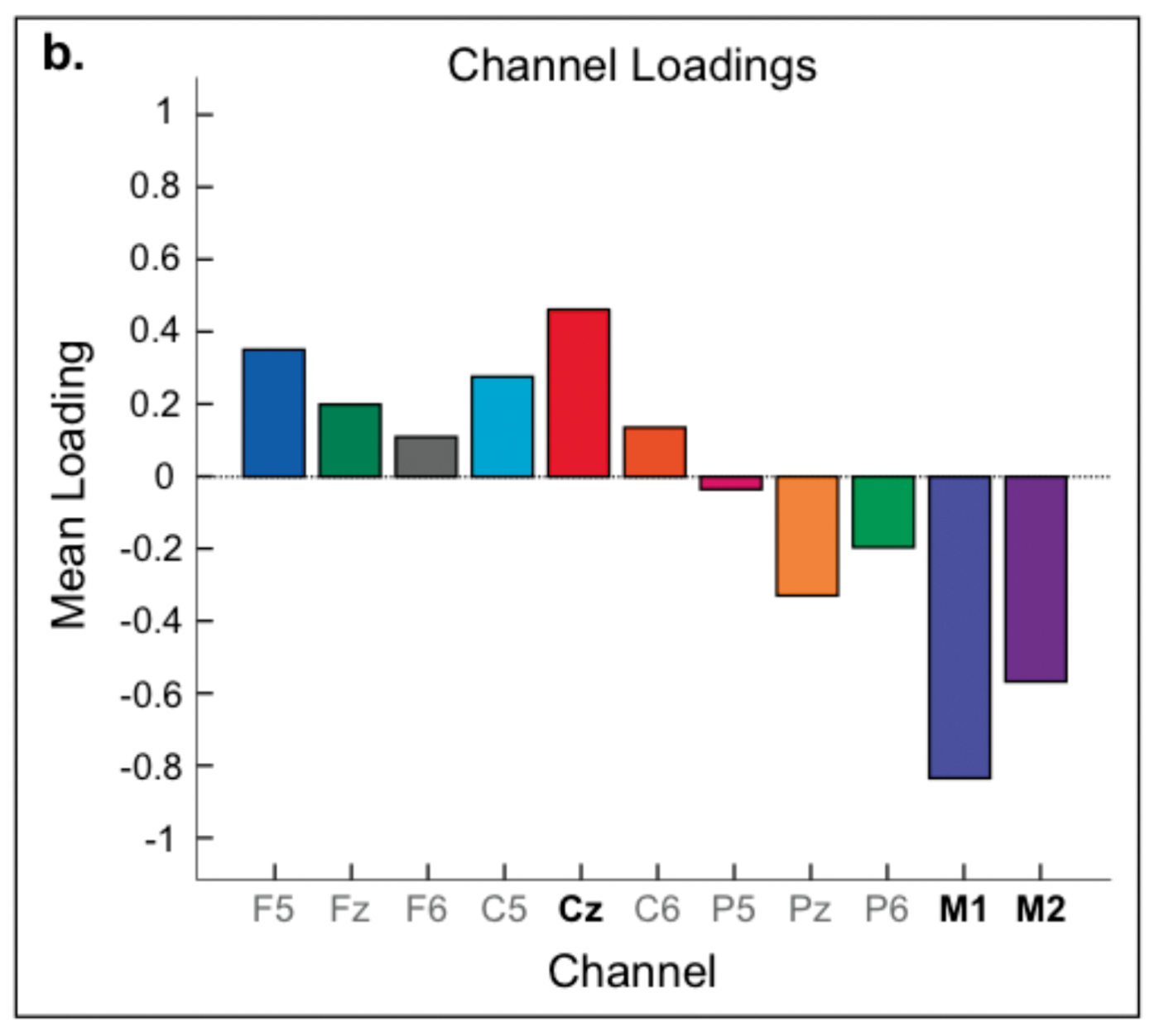
Figure 2. Channel loading to determine if number of electrodes could be reduced.
Results
Using an electrode montage that is similar to that used in clinic based on channel loadings (M1, M2, Cz; see Figure 2) we gathered results in normal hearing infants during a natural sleep state. Our findings in normal hearing infants concur with previous findings for MMR: 1) infants can and do process speech information during sleep; 2) these processes include speech discrimination; and 3) we can observe these processes using advanced EEG analyses [3]. Similar trends have been observed in the infants with hearing loss as well. Recently, we compared two different speech-evoked paradigms, ACC and MMR, again in sleeping infants (n=44). This study examined if speech discrimination results could be obtained in individual infants using ACC and MMR, for different filter settings (i.e. 1-18, 1-30, and 1-40Hz). For each filter setting, we conducted planned comparisons of age, sex, sleep state and randomisation, and there were no significant differences. We found that MMR was present in all individuals for the 1-18Hz filter settings, but the same was not true for ACC. To summarise the results of this study, ACC and MMR can be assessed during sleep, ACC is not sensitive to measuring speech discrimination in sleeping infants, and MMR is sensitive to measuring speech discrimination in individual sleeping infants [4].
Speech discrimination in the first few months of life shows promise for predicting later language outcomes
This physiologic measure of speech discrimination is being validated with a behavioural measure of infant speech discrimination at seven months of age using the same speech contrasts. Additionally, language outcomes are assessed at 16, 24, 30, and 33 months using a combination of parent report and formal measures of language development. Preliminarily, our results suggest a stronger relationship between MMR and VRISD for consonant-vowel contrasts than for vowel contrasts in infants with normal hearing. There are measurable differences between the aided and unaided responses in infants with hearing loss using the same speech contrast. Additionally, early analyses of parent questionnaires suggest a positive relationship for MMR and later language outcomes.
References
1. Baggato MP, Moodie ST, Seewald RC, et al. A critical review of audiological outcome measures for infants and children. Trends in amplification 2011;15:23-33.
2. Choudhury N, Benasich AA. Maturation of auditory evoked potentials from 6 to 48 months: prediction to 3 and 4 year language and cognitive abilities. Clin Neurophysiol 2011;122(2):320-38.
3. Gilley PM, Uhler KM, Watson K, Yoshinaga-Itano C. Spectral-temporal EEG dynamics of speech discrimination processing in infants during sleep. BMC Neuroscience 2017;18:34.
4. Uhler KM, Hunter SK, Tierney E, Gilley PM. The relationship between mismatch response and the acoustic change complex in normal hearing infants. Clinical Neurophysiology 2018;129:1148-60.
Declaration of Competing Interests: None declared.
TAKE HOME MESSAGE
-
There are many steps needed before implementing MMR in a clinical setting; however, MMR has the potential to validate hearing aid fittings using speech stimuli.
-
Speech stimuli are easier for families to understand than the pure tones that are used during the diagnostic evaluation process to diagnose hearing loss.
-
Speech discrimination assessed through MMR is related to behavioral speech discrimination visual reinforcement infant speech discrimination (VRISD).
-
Preliminary data suggests a significant relationship between MMR and later expressive language abilities.