Laryngeal paralysis remains very difficult to treat, but reinnervation offers many attractions.
Laryngeal paralysis presents a unique and varied problem that requires a patient centred approach and a range of treatment options depending on laryngeal and patient factors. There is increasing evidence to support the use of laryngeal reinnervation techniques in the rehabilitation of selected patients with both unilateral and bilateral palsy [1,2].
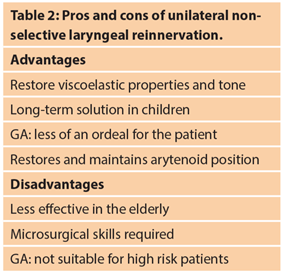
In unilateral vocal fold paralysis (UVFP) the goals of treatment are to improve voice, reduce aspiration and facilitate a more effective cough. The rehabilitative approach depends on the requirements of the patient, the fitness for surgery and likely best outcome. Non-selective reinnervation is a technique that aims to restore muscle tone and bulk to the paralysed hemilarynx, although movement coordinate with respiration and phonation is not achieved. The technique involves the anastomosis of a branch of the ansa cervicalis to the distal stump of the recurrent laryngeal nerve (Figure 1). It is an alternative to medialisation thyroplasty (+/- arytenoid adduction) where an implant is used to push the flaccid vocal fold into a more favourable position to facilitate glottic closure.
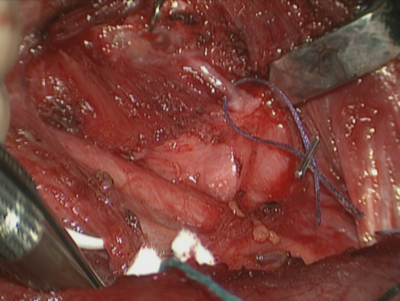
Figure 1. Identification of the RLN as it enters the larynx. A skin hook is used to rotate the larynx and fibres
of the inferior constrictor are dissected off the posterior border of the thyroid cartilage to expose the nerve.
Non-selective reinnervation offers several unique opportunities not covered by other procedures:
- In patients undergoing thyroidectomy with a pre-dating palsy or an intraoperative transection of the nerve, the reinnervation can be performed at the same time as the thyroid surgery. This spares the patient further surgery to deal with the palsy at a later date.
- There is significant evidence to suggest that early injection augmentation (within three months of palsy) reduces the need for any further intervention [3]. There is also evidence that silent aspiration from untreated UVFP carries a significant mortality and morbidity rate [4]. This would suggest that glottic competence should be maintained at all times. In order to perform a thyroplasty there must be no injectable substance present in the larynx in order to appropriately size the implant. For reinnervation however, the patient can be kept safe with injection augmentations prior to the procedure and until the reinnervation takes effect.
- Reinnervation offers a solution in children in whom UVFP may be idiopathic, but is also a common complication of ligation of a patent ductus arteriosus as well as other thoracic and neck surgery. Many of these children have aspiration requiring NG or PEG feeding with a risk of developing oral aversion. Thyroplasty is not an option and injection augmentation must be done under general anaesthetic and is temporary. Non-selective reinnervation offers a lifelong solution by improving tone in the hemilarynx to achieve glottic closure, thus allowing oral intake and facilitating voice. The importance of restoring voice is often overlooked in pre-verbal children but the future implications of significant dysphonia and glottic incompetence should not be underestimated. In Wessex a pathway of assessment and treatment for these children has been developed (Figure 2).

Figure 2. The Wessex Pathway for UVFP in Children.
In an elderly patient, axonal regrowth will be less vigorous and the risk of general anaesthetic greater. In this situation, a local anaesthetic injection augmentation or thyroplasty is probably a better option than reinnervation, keeping in mind that speech therapy input to minimise aspiration during any period of glottic incompetence is critically important in this vulnerable age group.
In bilateral palsy (BVFP), selective reinnervation is the only way to re-establish inspiratory abduction of the vocal folds whilst preserving voice. The alternative is a glottic enlargement procedure, which always impacts negatively on glottic competence with a degradation of voice and a risk of aspiration. The aim of glottic enlargement is solely to improve the airway but this improvement is, by necessity, only marginal and not adequate to sustain significant levels of physical activity. A tracheostomy provides an optimum airway whilst preserving glottic competence, but comes with much inconvenience and discomfort. For younger, active patients selective reinnervation is a potentially transformative option in that voice is maintained and it is possible to achieve significant glottic opening on inspiration allowing increased levels of activity.
“The technique of selective reinnervation has been refined over decades by the likes of Roger Crumley in the USA and has been modified and honed by Prof Marie into a surgical procedure that has the potential to be globally disseminated.”
The technique of selective reinnervation has been refined over decades by the likes of Roger Crumley in the USA and has been modified and honed by Prof Marie into a surgical procedure that has the potential to be globally disseminated. Over 60 bilateral selective reinnervations have now been performed in Rouen University Hospital in France. It involves a single surgical procedure and requires no expensive implants or ongoing medical involvement. If the patient does not already have a tracheostomy, one is fashioned at the time of surgery but removed after five days. Speech and language therapy input is required and potentially a period of NG feeding if aspiration is an issue in the postoperative period when there will be laryngeal relaxation and an increased glottic gap. Inspiratory abduction may be observed from about six months after the procedure but may take 12 to 24 months to fully develop.
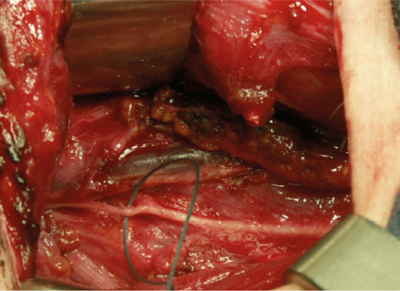
Figure 3. Upper root of phrenic nerve identified and to be ligated to provide inspiratory firing to the PCA muscles.
The technique involves utilising the upper root of the phrenic nerve on one side (Figure 3) to provide inspiratory innervation to both posterior cricoarytenoid (PCA) muscles via a Y-shaped cable graft. Phonatory closure is achieved by using the nerve to the thyroid hyoid muscle to supply motor fibres to the distal stump of the recurrent laryngeal nerve (via an interposition graft) bilaterally. These fibres are not active on respiration and so do not counteract the effect of the phrenic fibres now responsible for inspiratory contraction of the PCAs (Figure 4).
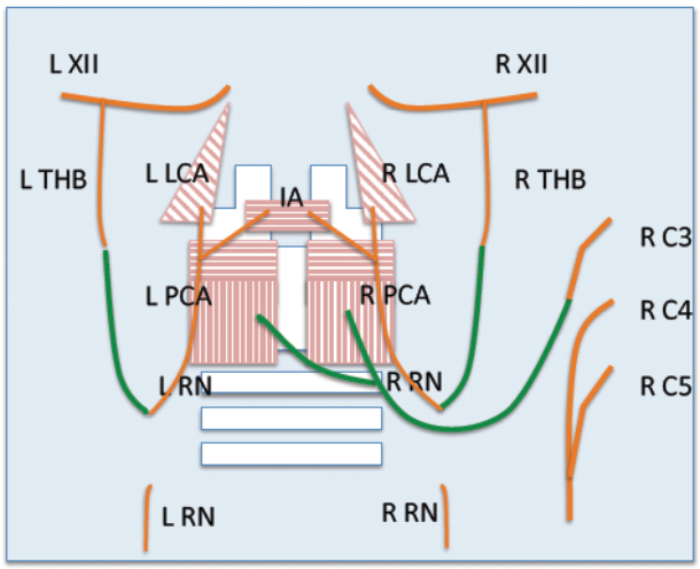
Figure 4. A schematic representation of selective laryngeal reinnervation for treating bilateral vocal palsy. RN: recurrent nerve; PCA: posterior cricoarytenoid; THB: thyrohyoid branch; LCA: lateral cricoarytenoid; IA: interarytenoid muscle; XII: hypoglossal nerve; C3-5: cervical nerve roots.
Careful patient selection is essential. The patient must be fit for the long surgical procedure and have no underlying respiratory conditions. The larynx is assessed under anaesthetic to confirm that the cricoarytenoid joints are fully mobile and that the immobility observed is not due to scarring. Laryngeal electromyography (LEMG) is also essential in this regard and to confirm the palsy and exclude complete muscle atrophy.
“The UK team, under the guidance of Prof Marie, are now offering bilateral selective reinnervation in adults.”
Forty cases performed in Rouen now have greater than one year follow-up and of these 35 were decannulated and 30 have evidence of improved respiratory parameters with voice preservation or recovery. These results include a number of patients with previous glottic enlargement surgery but preserved mobility in at least one cricoarytenoid joint. In these cases, if there is adequate inspiratory glottic opening, then a medialisation procedure may be performed later to improve voice. Diaphragmatic function has been shown to be preserved by utilising only the upper phrenic nerve root [5].
Bilateral selective reinnervation has been performed in three children under the age of three in Rouen. All three have been decannulated but final results are awaited in one. We have devised an assessment and treatment pathway for these children in Wessex (Figure 5).
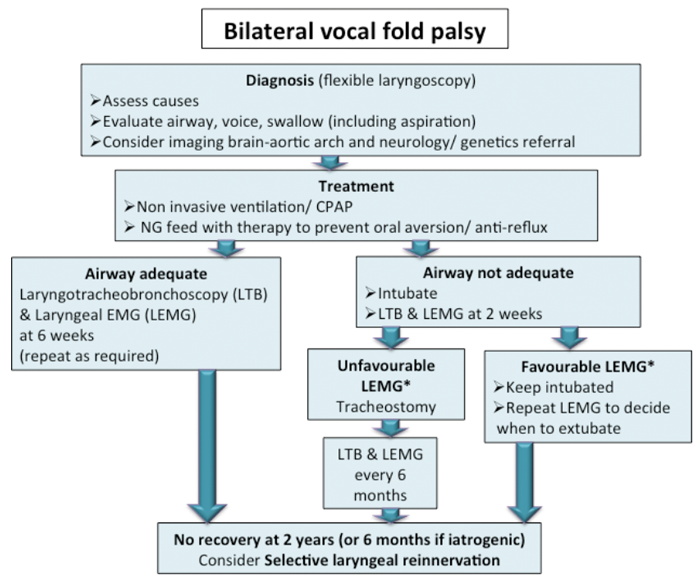
Figure 5. The Wessex Pathway for BVFP in Children. *Unfavourable and favourable LEMG refer to whether
the LEMG results indicate the laryngeal nerve function is unlikely to recover or recovery is likely respectively.
The UK team, under the guidance of Prof Marie, are now offering bilateral selective reinnervation in adults and look forward to keeping you updated with results and to undertaking our first paediatric cases.
References
1. Fancello V, Nouraei SAR, Heathcote K. Role of reinnervation in the management of recurrent laryngeal nerve injury: current state and advances. Current Opinion in Otolaryngology 2017;25(6):480-5.
2. Marie JP. Reinnervation: new frontiers. In: Rubin JS, Sataloff RT, Korovin GS, (Eds.). Diagnosis and Treatment of Voice Disorders. San Diego, USA; Plural Publishing; 2014:548.
3. Alghonaim Y, Roskies M, Kost K, Young J. Evaluating the timing of injection laryngoplasty for vocal fold paralysis in an attempt to avoid future type 1 thyroplasty. Journal of Otolaryngology - Head & Neck Surgery 2013;42:24.
4. Nouraei SAR, Allen J, Kaddour H, et al. Vocal palsy increases the risk of lower respiratory tract infection in low-risk, low-morbidity patients undergoing thyroidectomy for benign disease: A big data analysis. Clin Otolaryngol 2017;42(6):1259-66.
5. Verin E, Marie JP, Similowski T. Cartography of human diaphragmatic innervation: preliminary data. Respir Physiol Neurobiol 2011;176(1-2):68-71.
Acknowledgements:
We thank the following people for their contributions. Reza Nouraei, Virginia Fancello and Penny Scott from the Robert White Centre for Airway, Voice and Swallow, Poole Hospital NHS Trust, UK. Aude Lagier from Liège University Hospital, Belgium. Yakubu Karagama from Manchester University Hospital NHS Trust, UK. Martin Birchall from the Royal National Throat, Nose and Ear Hospital, London, UK. Andrea Burgess from Southampton Children’s Hospital, UK. Eleanor Sproson from Queen Alexandra Hospital, Portsmouth, UK.







