Can workers from the local community plug the workforce gap in providing ear and hearing care?
Bringing ear and hearing care services closer to the community remains a key component of reducing the burden of ear and hearing conditions across low- and middle-income countries (LMICs). Yet, despite the majority of disabling hearing loss occurring in LMICs, there remains a shortage of trained health professionals to recognise, treat and prevent hearing loss [1].
In a 2013 report published by the World Health Organization (WHO), it was revealed that 64% of participating countries from the African region had fewer than one ENT surgical specialist available per million people [2]. In contrast, all 12 high-income countries included in the survey had more than one ENT specialist available per million people. Similarly, 88% of high-income countries reported availability of more than one audiologist per million population, compared with only 5% in low-income countries [2].
Given this dire shortage of ENT and audiology professionals, a pragmatic approach needs to be explored to address the shortage in human resources for ear and hearing health. One suggestion to address the workforce crisis has been to take a ‘task shifting approach’ by training primary healthcare workers (PHWs), such as community health workers, nurse practitioners and general physicians, in recognition, treatment and management roles.
“CHWs also helped community members navigate the barriers in accessing specialist care by advocating for, and facilitating, community based ‘ear camps’”
In this article, we outline our personal experiences of working with PHWs to develop ear and hearing care services across LMICs, and highlight the opportunities and challenges of such an approach.
Opportunities
Our first-hand experiences across Uganda, Fiji, and Central and South America affirm that PHWs, as well as teachers, health planners and NGO programme coordinators, have an important role to play in the delivery of ear and hearing care services. For example, over a period of six years (2006-2012), a total of 96 courses on primary ear and hearing care were delivered in nine countries of the region of the Americas, with a total of 2330 persons trained. This training was facilitated by using the WHO Primary Ear and Hearing Care training resources, which have been divided into Basic, Intermediate and Advanced manuals. Figure 1 demonstrates the broad range of participants’ backgrounds from training conducted in Bolivia by Dr Santana.
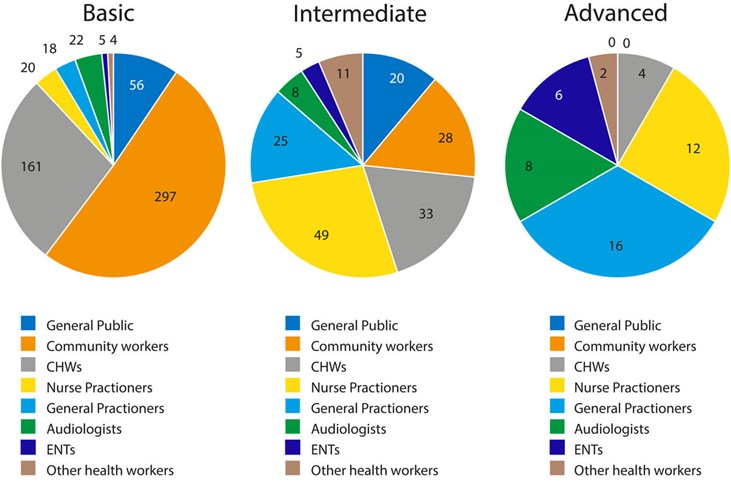
Figure 1. Proportional comparative of participants’ backgrounds by level of training in 51 courses
delivered in Bolivia for a total of 810 participants in PEHC courses.
This training has resulted in PHWs carrying out activities such as raising awareness, early diagnosis, prompt referral to specialist services and strengthening local health services and systems, as well as being an active advocate for accessible Universal Health Coverage and inclusive ear and hearing care services for all, particularly persons with disabilities. Similarly, in Fiji, Dr Oh Chungyeon has been involved in the training of health workers in every district of the country meaning that there is now widespread awareness of ear and hearing care services across the country.
In Sub-Saharan Africa, one particular cadre that has an important role to play in increasing awareness and access to ear and hearing care services is community health workers (CHWs) who operate at the interface of community and formal health service. In a recent project in Uganda, Drs O’Donovan and Nakku trained 14 CHWs to take audiological histories (Figure 2), perform otoscopic examinations and basic whispered hearing tests and deliver treatment, such as dry mopping and instillation of antibiotic ear drops.

Figure 2. A Community Health Worker Team take a history from a member of the community
(blue shirt) at his home regarding his symptoms of hearing loss.
CHWs also helped community members navigate the barriers in accessing specialist care by advocating for, and facilitating, community based ‘ear camps’. These were held every two months at the local health centre by local ENT surgeons. Cases were reviewed and those which could be managed conservatively in the community were discussed with the CHWs and an appropriate follow-up plan was formulated. It is therefore clear that there are several opportunities for PHWs to be involved in awareness raising, as well as basic management of ear disease in the community.
Challenges
Taking such an approach is not without its challenges however, including sociocultural barriers, the ongoing need for onward referral to specialists, lack of equipment and poorly developed local infrastructure for managing advanced disease, and unidentified long-term outcomes from training.
For example, in Uganda, there is commonly a distrust of formal sector health providers due to the ‘informal fees’ that are requested from patients when seeking care. Furthermore, it is often difficult for individuals living in remote or rural regions to access specialists who are located in major urban centres, due to the high costs of transport. There is therefore a need to consider bringing specialist services direct to the community in order to reduce access barriers to these services; for example, through regular outreach camps where ENT surgeons travel to host clinics and surgeries in the community. This is a model which has been used in Nepal for several years with success [4].
Training PHWs can be beneficial for raising awareness and providing basic treatment, however it does not negate the need for the continued recruitment and training of specialists, such as ENT surgeons and audiologists. In Fiji, Dr Oh Chungyeon is the only ENT specialist, and in Uganda there are fewer than 40 ENT surgeons for a population of over 42 million. Training and retention of specialist providers is therefore essential in order to ensure complex problems identified by the PHWs can be addressed. Likewise, PHWs and ear care specialists need to be appropriately supported in order to provide the best possible care. For example, one of the major regional referral hospitals with ENT services in Uganda was unable to accept several of the patients due to the lack of functioning microscopes for several months.
“PHWs must be appropriately supported, financed and trained for maximum impact”
This led to feelings of disappointment amongst the community, which the PHWs ultimately had to manage. In many countries, funding for primary ear and hearing care services remains challenging given the competing interests with other programmes aimed at addressing sizeable disease burdens such as HIV and TB. We therefore advocate for an integrated approach to ear and hearing care services by embedding these as part of a wider health systems strengthening approach, rather than viewing it as a vertical intervention.
Conclusion
In conclusion, it is important to note the potential and important roles that PHWs can have in strengthening primary ear and hearing care in LMIC settings. For maximum impact it must be seen as a ‘systems strengthening approach’. This means taking a holistic approach to improving tertiary referral services, strengthening the capacity of ENT and audiology, and raising awareness at a local, national, and international level.
Finally, it is important that PHWs, should not be viewed as a low-cost alternative to ENT surgeons or audiologists. They must be viewed as vitally important workers in their own right, with a significant role to play in bringing much needed ear and hearing services to marginalised, remote and underserved populations. To make it clear, PHWs must be appropriately supported, financed and trained for maximum impact [5]. We have witnessed first-hand the impactful and important roles they can play in resource constrained settings around the world and therefore implore governments, policy makers and NGOs to continue to invest in them in order to bring ear and hearing services to the hardest to reach.
References
1. Mulwafu W, Ensink R, Kuper H, Fagan J. Survey of ENT services in sub-Saharan Africa: little progress between 2009 and 2015. Global Health Action 2017;10(1):1289736.
2. The World Health Organization, Multi-country Assessment of National Capacity To Provide Hearing Care. The World Health Organization. Geneva, Switzerland. 2013.
3. O’Donovan J, Verkerk M, Winters N, et al. The role of community health workers in addressing the global burden of ear disease and hearing loss: a systematic scoping review of the literature. BMJ Global Health 2019;4(2):e001141.
4. Clark M. Surgical ear camp in Nepal. The Tinnitus Clinic.
www.thetinnitusclinic.co.uk/tinnitus-news/
surgical-ear-camp-in-nepal
Last accessed April 2021.
5. Cometto G, Ford N, Pfaffman-Zambruni J, et al. Health policy and system support to optimise community health worker programmes: an abridged WHO guideline. The Lancet Global Health 2018;6(12):e1397-e404.
Acknowledgements:
We wish to acknowledge the primary healthcare workers we work with in Uganda, Fiji, Bolivia, Peru, Paraguay, Guatemala, El Salvador, Nicaragua, Cuba, Dominican Republic and Mexico for their tireless work and dedication. We wish to extend our thanks to Dr Esther Nagasakka and Dr Daniel Nyanzi for their work in leading the ear camps referred to in this article in Uganda. We also wish to thank Dr Oh Chungyeon for sharing his experiences from Fiji.






