The field of cochlear implants in children has expanded remarkably over 40 years. Elizabeth Tyszkiewicz reflects on success and current challenges and calls for a national review of outcomes for young adults who received their implants in childhood.
Aleena is 12 years old, successfully negotiating Year 7 at her local secondary school, with a full family, academic and social life. Joshua is six. He has multiple physical and learning disabilities, and attends a specialised school programme for children with severe difficulties. Susannah is eight, attends her neighbourhood primary school and has suddenly become profoundly deaf, having been a typically hearing child until she had meningococcal meningitis three months ago. All these children are cochlear implant users, and each of them represents a familiar case example to any member of a UK cochlear implant team.
The sheer variety and complexity of paediatric cochlear implant work could not have been foreseen when the first multidisciplinary teams were recruited to support this exciting new hearing technology. Hearing is the portal to the spoken language-learning brain, and a large group of previously excluded young individuals gained the opportunity to fulfil their hearing and speaking potential. Forty years on, those who were there at the outset celebrate success, but also reflect on the complex and intriguing questions that arise from the work done so far: while there are some robust data to account for the astonishing achievement of the most successful users, how do we explain the remaining immense variability of spoken language, educational, and social outcomes [1]?
Once the cochlear implant system has been fitted, the question of how to proceed has filled many hours of discussion, and many pages of text. Is sign language a crucial part of learning, or a hindrance to spoken language development? Is intervention needed, or can a child simply develop in the hearing environment? What are the outcomes of specific therapy and education programmes? Many of these questions existed before the advent of cochlear implants, of course, but the complexity and sophistication of the technology, the expertise and resources it attracted, and the observed results, brought them into sharp focus.
“Now, with many years of experience behind us, we can take a measured view of the situation, celebrate success, and think about where the areas of difficulty lie.”
In the early days of paediatric cochlear implant work, professionals often felt it was their duty to lower the expectations of families, for fear that the technology would not live up to its promise, resulting in disappointment and blame. At the same time, conferences were awash with bar charts and other graphic representations of the immense improvement in auditory perception and speech provided to paediatric populations. Families became increasingly ambitious for their children, teachers saw new potential, and therapists developed innovative ways of working to exploit the possibilities that were opening up. Now, with many years of experience behind us, we can take a measured view of the situation, celebrate success, and think about where the areas of difficulty lie [2].
As the cases presented above show, cochlear implant teams in the UK support children with a bewildering variety of attainment, need, social environment, or conditions additional to hearing loss. We have clear and stringent guidelines from NICE (National Institute for Health and Care Excellence) to define the patient group who, on the basis of the evidence, are thought to benefit most [3]. We have generally well-resourced departments. Yet, in day to day work, clinical and ethical questions such as these are commonplace:
- Should we offer cochlear implant surgery when years of experience of similar cases to this one tell us that we should have severe doubts about the outcome?
- What is the place of auditory brainstem implant (ABI) in a paediatric service?
- Is it ethical to work strictly within the NICE guidelines in the case of children who, our experience and observation tell us, would benefit more from a cochlear implant system than from their hearing aids, but who fall outside the NICE criteria?
For example, the two-year old child whose audiogram is shown in Figure 1 is likely to struggle with spoken language development using hearing aids, but the current guidelines do not allow her to be offered a cochlear implant system.
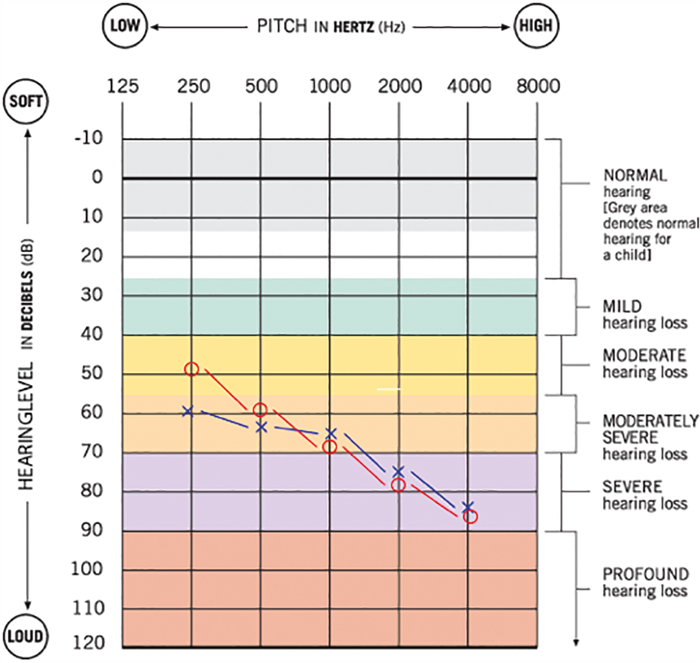
Figure 1. Paediatric borderline candidate.
Despite, or perhaps because of questions such as these, paediatric cochlear implants continue to be a fascinating and compelling field to work in, and those who have that privilege are usually enthusiastic about their part in it. There have been astounding results, with children and their families embracing the new technology, and making it a part of every aspect of learning and development.
Auditory verbal therapy, which specifically targets the auditory potential of each individual, and works to the strengths of the family, has gone from a minority preference to a mainstream option.
We have university students, young professionals, musicians, and sports enthusiasts among the many young people now growing to adulthood as the first cohort of born-deaf children to use cochlear implants. There are also severely disabled young people whose experience of the world, and contact with their family and friends, has been enhanced by access to hearing. On the other hand, we may have as much, or more to learn from those who are disappointed, or disaffected, or who have become non-users of their devices. Review of these cases plays a crucial part in our gradual establishment of a long-term knowledge base for auditory implant technologies. For example, we now know that some children with congenital profound deafness who began using cochlear implants when they were already well beyond the pre-school years, struggled to gain any appreciable benefit, and sometimes abandoned the use of their devices [4].
“There is a strong case for a national review of outcomes in today’s young adults, with both objective measurements and patient views of their life as cochlear implant users.”
Taking into account this early experience, most cochlear implant teams in the UK are now extremely cautious about proceeding with cochlear implant surgery in such cases. On the other hand, children with severe to profound hearing loss, who did not initially fall within the criteria for benefit, may come forward for re-assessment, and go on to be satisfied cochlear implant users. The message is clear: every year of experience, every methodical review of the available data, and every set of well-documented outcomes consolidates practice, and allows us to make the best possible decisions on behalf of our paediatric patients.
It will be fascinating to hear from all of them what their experience has been, and what advice they have for the next generation of cochlear implant users, manufacturers and clinicians. There is a strong case for a national review of outcomes in today’s young adults, with both objective measurements and patient views of their life as cochlear implant users. The tradition of collaborative working and data collection that is characteristic of cochlear implant practice in the UK makes it a favourable choice for such a study. The results would provide a rich resource for professionals, academics and patients in the next 40 years of hearing technology development.
References
1. Geers AE, Mitchell CM, Warner-Czyz A, Wang N-Y, Eisenberg LS, CDaCI Investigative Team. Early sign language exposure and cochlear implantation benefits. Paediatrics 2017;140(1).
2. Maggs J, Ambler M, Hanvey K. Cochlear implantation – which child when? Paediatrics and Child Health Journal 2017; [Epub ahead of print]
https://doi.org/10.1016/j.paed.2017.06.002
3. NICE. Cochlear implants for children and adults with severe to profound deafness. 2009; https://www.nice.org.uk/guidance/ta166
4. Archbold S, Nikolopoulos TP, Lloyd-Richmond H. (2009), Long-term use of cochlear implant systems in paediatric recipients and factors contributing to non-use. Cochlear Implants International 2009;10(1):25-40.




