The philosophy of endoscopic ear surgery presents surgeons with a tricky concept – does the magnificent view make up for the fact I need to operate with one hand? In this article, Jane Lea discusses the advantages of operating transcanal on middle ear disease, and suggests methods of improving one handed surgery.
Overview
While the general principles of ear surgery have remained relatively constant over time, mainly to eradicate disease while preserving hearing, balance and facial nerve function, the modalities used to accomplish this goal have evolved, largely in parallel with technologic advancements. Recent endoscopic and optical advancements have brought minimally invasive endoscopic ear surgery (EES) to the forefront in the 21st Century.
“Ear surgery is traditionally performed using a microscope, but the endoscopic view offers specific advantages owing to the greater field of view and ease of access to ‘hidden areas.’”
Ear surgery has seen many paradigm shifts throughout history, from the era of trephination in the 16th-18th Centuries, to ‘chisel and gouge’ in the 19th Century, to the ‘electrical drill and microscope’ in the 20th Century. EES has roots dating back to the 1960s [1], but it is only within the last decade that the technique has grown in popularity, with an exponential increase in publications, presentations and training courses on EES [2].
The surgical approach with EES differs from traditional microscopic surgery and adjustments are necessary owing to the one-handed technique and alterations in depth perception that come with endoscopic surgery. The inherent advantages of the technique, specifically the wide field of view, affords the ability to see and dissect around corners, thereby exposing ‘hidden recesses’ that standard microscopic ear surgery cannot provide. The wide field of view provided by the endoscope offers additional downstream benefits including improved patient outcome / satisfaction, and greater healthy tissue preservation.
One-handed technique
The one-handed technique of EES is perceived as one of its major limitations, especially among those who favour microscopic techniques. Similar to functional endoscopic sinus surgery (FESS), the non-dominant hand holds the endoscope, and surgery is performed using the dominant hand, resulting in a one-handed technique (Figure 1).

Figure 1: EES operative positioning.
The endoscopic technique is performed transcanal using the external auditory canal as a natural pathway to the middle ear, thereby limiting healthy tissue removal.
The main function of the non-dominant hand in microscopic ear surgery is to suction the operative field of blood, while the dominant hand performs the vast majority of the important surgical dissection [3]. Haemostasis is therefore essential in the setting of one-handed surgical techniques. The minimally invasive nature of EES fosters a reduction in local tissue trauma (less dissection, minimal incisions required) and hence reduces troublesome bleeding.
Suggestions for overcoming the limitations of a one-handed surgical technique
- Take a hands-on course on EES or visit an International Working Group of Endoscopic Ear Surgery member (www.iwgees.org) to gain experience.
- Start with a graded approach to case complexity (start with cerumen debridement, tubes, myringoplasty, and advance to tympanoplasty and cholesteatoma surgery over time).
- Initial cases should be selected with favourable anatomy (i.e. widely patent ear canal, absence of infection / granulation tissue).
- Start with a zero degree endoscope, and advance to angled scopes as experience increases.
- Proper operative positioning with arm rests to provide support for both elbows throughout the case (Figure 1) to avoid fatigue and improve manual dexterity.
- Proper positioning of the monitor in a “neck neutral” position to avoid fatigue.
- Trimming the ear canal hairs can limit repeated smearing of the endoscope.
- Ensure you have the proper equipment. To start with the technique, a 3CCD camera, FESS endoscopy equipment, and a basic otologic set including angled / curved instruments traditionally used with the microscopic approach are sufficient.
- Pearls to improve haemostasis
- Inject the ear canal before scrubbing to provide time for the epinephrine to work. Apply neuro-patties soaked in topical epinephrine to the bony ear canal.
- Advocate for hypotensive anesthesia and slightly elevate the head of the bed.
- Acknowledge that the most difficult step in EES is the elevation of the tympanomeatal flap as this causes the most bleeding. - Once the middle ear is entered the bleeding is typically minimal.
- If necessary when starting with the technique for the first time elevate the tympanomeatal flap with the microscope and then switch to the endoscope upon entering the middle ear.
- Use neuro-patties or gelfoam soaked with topical epinephrine throughout the flap elevation. Irrigate with saline, remove blood from the field before application of topical epinephrine, and be patient and wait for the topical epinephrine to take effect before proceeding.
- Consider having an experienced colleague assist with suctioning when learning EES (Figure 2).
- Consider purchasing a suction round knife, an instrument that permits dissection and suction simultaneously.
“Technical adjustments in technique can help to overcome the one-handed technique and depth perception challenges afforded with the endoscopic technique, and allow the plethora of endoscopic advantages to come to fruition: improved visualisation, greater healthy tissue preservation, decreased residual / recurrent disease rates, and improved patient satisfaction.”
Figure 2: Three-handed technique.
Lack of depth perception
Another perceived disadvantage of EES is the two-dimensional nature of the operative image that limits depth perception. However, this has been overcome in FESS, and thus we can learn from the experiences of our sinus colleagues by accommodating for the lack of depth perception by acknowledging the following key points:
- Small movements of the scope result in subtle changes in the field of view, which when processed jointly allows us to configure a three-dimensional understanding of the operative field despite the two-dimensional nature of the image. In other words, it is important to continually move the endoscope to accurately judge the depth of field.
- The endoscope creates a ‘fish-eye’ optical distortion whereby the periphery of the operative field is more magnified than the centre. The optical distortion created by the endoscope predisposes surgeons to misjudge distances and make the tympanomeatal flap too short. Using a surgical tool (i.e. round knife) to measure distance assists with overcoming this when getting started with EES.
Wide field of view
During microscopic surgery, the field of view is limited by the narrowest segment of the ear canal. The use of an endoscope allows one to easily bypass the narrow segment and look beyond without excising healthy tissue for exposure (Figure 3). An anterior perforation can therefore be repaired entirely transcanal with an endoscope, without the postauricular incision and canaloplasty often required with microscopic techniques.

Figure 3: Narrow microscopic (top) versus wide endoscopic (bottom) view.
Cholesteatoma can be removed without extensive bony removal (often avoiding a mastoidectomy) and without external incisions even with disease extension beyond the antrum (as long as disease does not extend beyond the limits of the lateral canal).
“Endoscopic and optical technologic advancements have pushed us toward yet another possible paradigm shift, and as we move into the 21st Century we continue to explore and define the role of the endoscope in ear surgery.”
Only a small amount of bony scutum needs to be removed to greatly improve visualisation. A few millimetres of exposure is of exponential benefit in endoscopic approaches.
The greatest benefit of the endoscope lies in exposing previously hidden areas or blind spots such as the retrotympanum, hypotympanum, anterior mesotypanum, epitympanum and antrum (Figure 4).
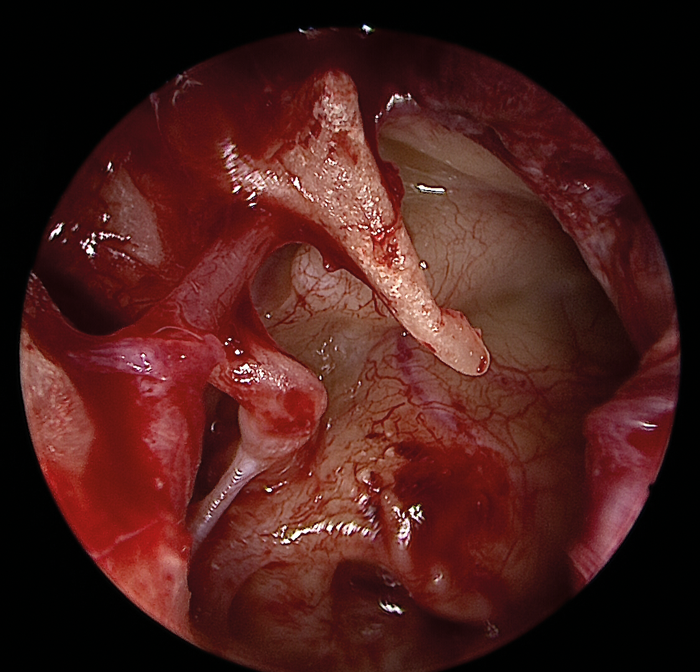
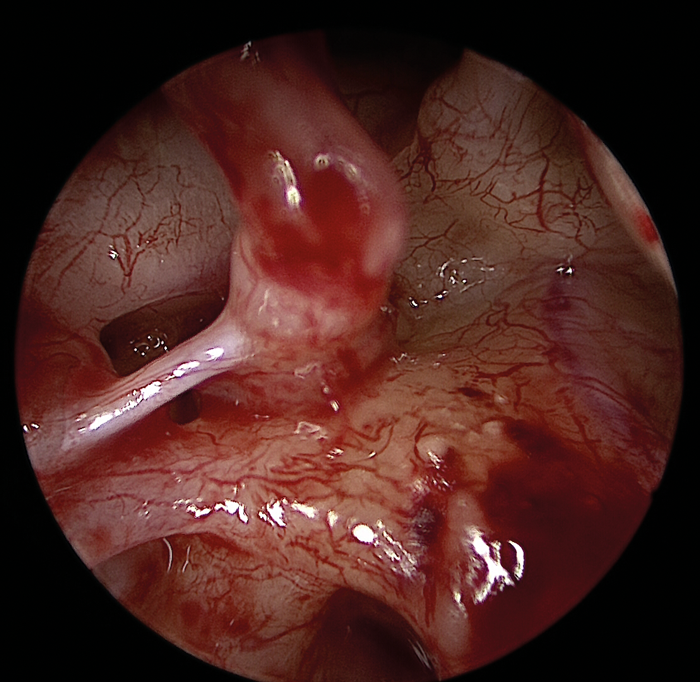
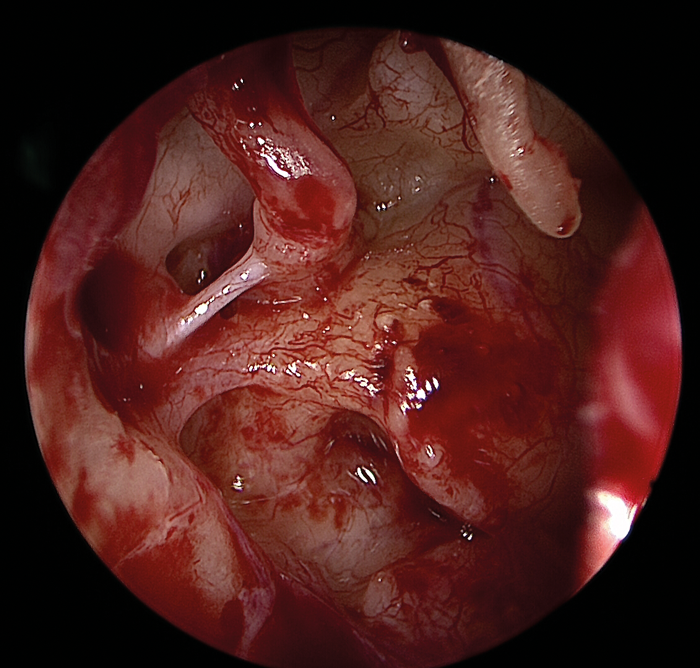
Figure 4 (Top, middle and bottom): Endoscopic view of the middle ear with an intact ossicular chain.
The improved visualisation of hidden structures in a minimally invasive fashion results in a reduction in residual and recurrent disease rates [4,5], less postoperative pain, quicker recovery, no external incisions, no need for bulky mastoid dressings.
Conclusion
The endoscopic benefit of exposing ‘hidden recesses’ and ‘blind spots’ in ear surgery is the primary rationale for the growing support of EES over the last decade. The minimally invasive nature of the endoscopic approach affords greater healthy tissue preservation and results in patient benefits that cannot be ignored. EES is likely here to stay, until of course the next major paradigm shift in ear surgery bursts onto the scene, likely paralleling another major technologic advancement in surgical instrumentation.
References
1. Mer SB, Derbyshire AJ, Brushenko A, Pontarelli DA. Fiberoptic endotoscopes for examining the middle ear. Archives of Otolaryngology 1967;85(4):387-93.
2. Mijovic T, Lea J. Training and Education in Endoscopic Ear Surgery. Current Otorhinolaryngology Reports 2015;3:193-9.
3. Pothier DD. Introducing endoscopic ear surgery into practice. Otolaryngologic Clinics of North America 2013;46(2):245-55.
4. Migirov L, Shapira Y, Horowitz Z, Wolf M. Exclusive endoscopic ear surgery for acquired cholesteatoma: preliminary results. Otology and Neurotology 2011;32(3):433-
5. Ayache S, Tramier B, Strunski V. Otoendoscopy in cholesteatoma surgery of the middle ear: what benefits can be expected? Otology and Neurotology 2008;29(8):1085-90.
Declaration of Competing Interests: None declared.





