Introduction
Over the past 150 years, military personnel wounded in action had a survival rate of approximately 80% [1]. During the current conflicts in Iraq and Afghanistan, those servicemen wounded in action have a 90.4% survival rate [2].
During the past 10 years in Iraq and Afghanistan, greater than 7000 American military personnel have been treated for head and neck injuries at American medical facilities in both war zones [3]. The multispecialty head and neck surgical teams treating the maxillofacial injury (MFI) patients include neurosurgeons, otolaryngologists-head and neck surgeons, oral maxillofacial surgeons, and ophthalmologists [4]. Valuable head and neck trauma lessons applicable to military and civilian practice were learned in Iraq and Afghanistan.
Acute surgery for MFI
Lessons learned in Iraq and Afghanistan can be categorised according to the surgical procedures performed: soft tissue repair of facial lacerations, traumatic airway management, mandibular / midface open reduction and internal fixation (ORIF), penetrating neck trauma exploration, laryngotracheal repair, and otologic trauma management [4, 5].
Preoperative planning
Multislice helical computed tomography angiography (MCTA) is essential in the preoperative evaluation of a MFI patient in the combat zone. MCTA will demonstrate the projectile tract with associated injuries to include bony fractures, vascular injury, and aerodigestive tract injury [6]. MFI patients presenting with Zone 1 or Zone 2 penetrating neck trauma need additional studies to rule out esophageal injury. Panendoscopy, to include flexible and rigid esophagoscopy, is the most sensitive technique to rule out esophageal perforation. Lastly, 3-dimensional CT (3D-CT) scans are critically important in the planning of facial fracture repair [5].
Surgical procedures
Soft Tissue Repair
Facial laceration repair with soft tissue approximation was the most common head and neck operation performed in both Iraq and Afghanistan. The first lesson learned with traumatic soft tissue repair, typically due to high-velocity missile trauma, is that the soft tissue can be closed immediately after extensive irrigation and conservative debridement.

Figure 1: Soft tissue damage by IED.
The most important lesson learned is that the ‘home run’ surgery should be avoided. After high-velocity injury to the facial soft tissues, the temporary cavity that results from the high kinetic energy of the missile may partially devitalise a large area of soft tissue extending up to 30 times the missile cross section (Figure 1) [7]. Even with the great blood supply to the face, ‘doing too much too soon’ with extensive soft tissue undermining and flap rotation may result in dead tissue. The goal of soft tissue repair should be primary closure of the soft tissue defect with coverage of the plates and bone [5].
Airway management
Airway compromise is the third leading cause of potentially survivable death on the battlefield behind compressible haemorrhage and tension pneumothorax [8]. Ten percent of patients in Iraq with high-velocity MFI necessitating traumatic airway intervention required immediate intubation or emergent cricothyroidotomy / tracheotomy by surgeons after initial airway management failed (red or emergent airway) [9]. The best method to assess airway patency during the primary trauma survey is to ask the patient to talk [9]. If the patient can give an intelligible and appropriate reply, then he or she has a patent airway, adequate ventilation to vibrate the true vocal cords and generate voice, and a Glasgow Coma Scale of greater than 8 indicating brain perfusion [9]. The key to airway management is to prevent a yellow (urgent) or green (elective) airway from becoming more unstable and transitioning to a red airway [9]. Trauma patients with a yellow airway and abnormal anatomy distorting airway landmarks will typically be managed with awake tracheotomy under local anesthesia.
Bony repair
Mandible
The three most important goals of mandibular fracture repair are occlusion, occlusion, occlusion! The establishment of premorbid occlusion with Erich arch bars or intermaxillary fixation (IMF) screws is the single most important step in mandibular repair. If there is severe comminution and displacement, the surgeon should proceed with exploring the wound with special attention to preserving all bony mandibular fragments and preserving any soft tissue attachments to these fragments [5]. Then a mandibular reconstruction plate, such as the 2.4 mm locking plate, is secured from the stable bone to the opposite stable bone on both sides of the intact mandible. The largest mandibular fragments, typically comprised of bone from the inferior border of the mandible with soft tissue still attached, are secured with screws into the reconstruction plate with every effort made to achieve bone-to-bone contact and to preserve soft tissue attachments (Figure 2). After the mandibular body and symphysis are reconstructed, smaller mandibular fragments, typically from the occlusal surface of the mandible near the teeth, are replaced and fixed with smaller mandibular or craniofacial plates to the larger inferior bony segments. Finally, soft tissue coverage is achieved following the principles previously discussed.
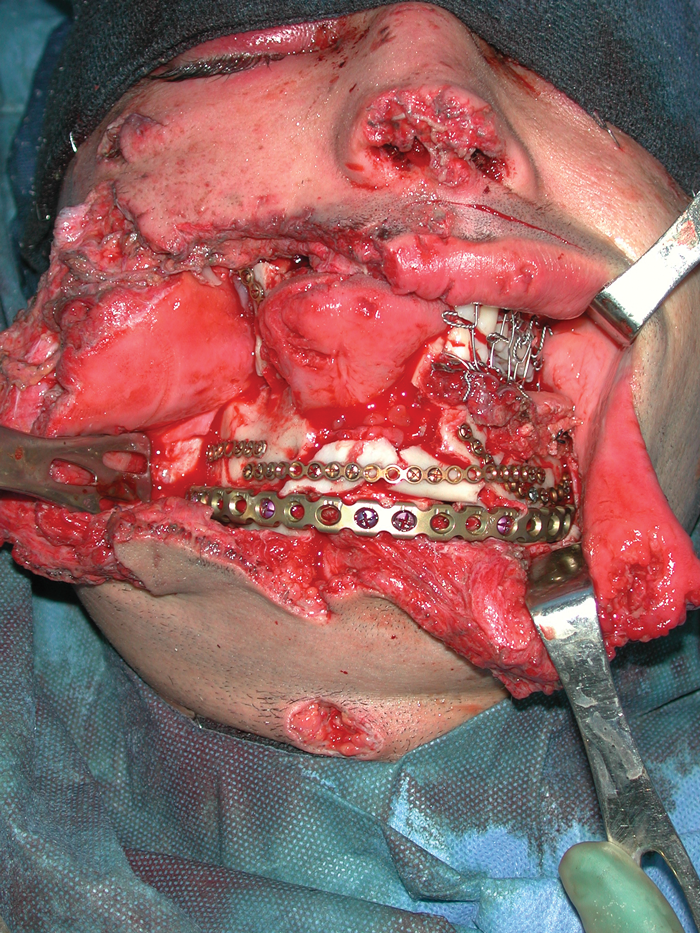
Figure 2: ORIF Mandible-Midface Fractures.
Panfacial fractures
The first step in the management of panfacial fractures is airway and haemorrhage control. The next step is to ‘set the base’ for the panfacial repair. Since the ‘base’ is the mandible, IMF and ORIF of mandible fractures, if indicated, are performed first. IMF alone in patients without mandibular fractures may be needed to stabilise and set the ‘base’ in patients with severely comminuted and displaced midface fractures with a mobile upper jaw. After the appropriate surgical approaches are made and the bony fractures exposed, the bony segments should be reduced and positioned into their premorbid position ensuring that the midface height and projection are preserved. The malar eminence (ME) is the key to adequate midface ORIF. After fracture reduction, the midface needs to be built from stable points to unstable points [5].
“The hope is that these costly lessons learned in the combat zone can be applied to the civilian practice of MFI and improve the current quality of care in civilian institutions.”
Neck / Skull base exploration
Since World War two, high-velocity penetrating neck trauma (PNT) has been treated with mandatory neck exploration by military surgeons. However, in Iraq and Afghanistan, selective neck exploration is the current practice [10].
PNT patients are divided into two categories: asymptomatic and symptomatic patients [10]. Asymptomatic PNT patients need to be evaluated with a MCTA and panendoscopy if indicated. If the work-up is negative, then these patients can be closely observed. However, PNT patients who are symptomatic or who are asymptomatic but found to have significant findings on diagnostic testing will undergo neck exploration.
Laryngotracheal repair
The indications for laryngotracheal exploration and repair include large mucosal lacerations, exposed cartilage, displaced fractures, and vocal cord immobility [11]. All patients with high-velocity laryngotracheal trauma require direct laryngoscopy to assess the extent of laryngeal trauma and hypopharyngeal disruption [11] During exploration, the principles of laryngotracheal repair include reduction and stabilisation of fractures, mucosa-to-mucosa closure of respiratory tract defects, and use of endolaryngeal stents as indicated [11].
Otologic / vestibular trauma
Traumatic hearing loss is the most common reason for outpatient visits to the otolaryngology clinics in the combat zone [4]. In addition, tympanic membrane perforation is the most common primary blast injury in OIF and OEF, and occurs in approximately 10% of patients wounded by combat explosions [12]. Hearing protection, to include the use of combat ear plugs, is rarely used by the infantry soldiers and marines [4].
Conclusions
The surgical advances and lessons learned in the treatment of maxillofacial injuries have been identified. The hope is that these costly lessons learned in the combat zone can be applied to the civilian practice of MFI and improve the current quality of care in civilian institutions.
References
1. Champion HR, Bellamy RF, Roberts P, Leppaniemi A. A profile of combat injury. J Trauma 2003;54(5):S13-S19.
2. Gawande A. Casualties of war – military care for the wounded from Iraq and Afghanistan. N Eng J Med 2004;351(24):2471-5.
3. Feldt, BA, Salinas NL, Rasmussen TE, Brennan J. The Joint Facial and Invasive Neck Trauma (J-FAINT) Project, Iraq and Afghanistan 2003-2011. Otolaryngol Head Neck Surg 2013;148(3):403-8.
4. Brennan J. Experience of first deployed otolaryngology team in Operation Iraq Freedom: changing face of combat injuries. Otolaryngol Head Neck Surg 2006;134(1):100-5.
5. Brennan J. Head and neck trauma in Iraq and Afghanistan: different war, different surgery, lessons learned. Laryngoscope 2013;123:2411-7.
6. Inaba K, Munera F, McKenney M, et al. Prospective evaluation of screening multislice helical computed tomography angiography in the initial evaluation of penetrating neck injuries. J Trauma 2006;61:144-9.
7. Holt GR, Kostohryz G Jr. Wound ballistics of gunshot injuries to the head and neck. Arch Otolaryngol 1983;109:313-8.
8. Mabry RL, Edens JW, Pearse L, et al. Fatal airway injuries during Operation Enduring Freedom and Operation Iraqi Freedom. Prehospital Emergency Care 2010;14:272-7.
9. Brennan J, Gibbons MD, Lopez M, et al. Traumatic airway management in Operation Iraqi Freedom. Otolaryngol Head Neck Surg 2011;144(3):376-80.
10. Brennan J, Lopez M, Gibbons MD, et al. Penetrating neck trauma in Operation Iraqi Freedom. Otolaryngol Head Neck Surg 2011;144(2):180-5.
11. Schaefer SD. The treatment of acute external laryngeal injuries. Arch Otolaryngol Head Neck Surg 1991;117:35-9.
12. Ritenour AE, Wickley A, Ritenour JS, et al. Tympanic membrane perforation and hearing loss from blast overpressure in Operation Enduring Freedom and Operation Iraqi Freedom wounded. J Trauma 2008;64:S174-S178.
Disclaimer
The views of the author do not necessarily reflect those of the US Army and the US Department of Defense.
Declaration of Competing Interests: None declared.




