Migraine is one of the commonest conditions an otologist will have to manage with up to half of migraineurs displaying vestibular symptoms. David Selvadurai provides an overview and management plan for this increasingly well recognised disorder.
Migraine is a common condition in which headache occurs with other neurological symptoms. The condition is episodic and chronic, with the tendency to develop migrainous symptoms persisting throughout an individual’s lifetime.
Dizziness and vertigo have long been recognised as common neurological manifestations of migraine in association with headache. There are a wide variety of manifestations of the condition and this combined with difficulties around nomenclature have hindered its management.
A large number of terms have been applied to this condition: migrainous vertigo (MV), vestibular migraine (VM), migraine associated dizziness and migraine related vestibulopathy. The International Headache Society (IHS) define only one subtype of migraine related vertigo – basilar migraine, but this very specific diagnosis represents only a small subgroup of the patients where migraine is considered the underlying pathology of their dizziness.
The IHS classification [1] classifies migraine into headache with aura and without. Basilar migraine falls into the first category and both the vertigo and tinnitus are considered types of aura. Within balance clinics it has become clear that many patients have balance disorder without clear headache at the time, and do not fit the IHS classification but still demonstrate many migrainous features and benefit from anti migrainous treatment.
“Migrainous headache does not have to occur with the vertigo, it can precede it by many years or occur before or during the vertigo.”
Migraine and dizziness are both very common in the general population with migraine prevalence estimates ranging from 5% in men to 20% in women between ages 30-49. However vertigo symptoms are unexpectedly common in migraineurs, with up to 50% of migrainous headache sufferers displaying vestibular symptoms. This far exceeds those who fit the criteria for basilar migraine. Similarly the incidence of migraine in patients attending balance clinics is higher than in the general population, perhaps three times the expected prevalence [2]. It has been estimated that MV has a lifetime prevalence of approximately 1% [3].
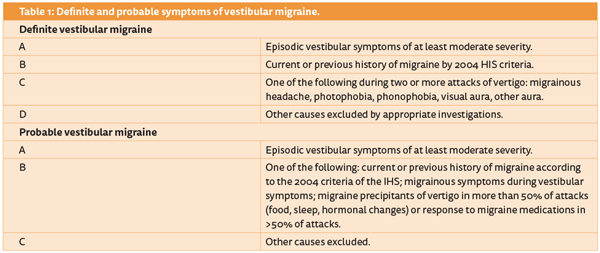
Based on these findings Neuhauser [2] proposed a more liberal classification for MV splitting symptoms into definite and probable categories (Table 1).
Pathophysiology
This is unclear. Spreading cortical depression is thought to underlie the causation of migraine but this is inadequate to explain the peripheral changes seen in MV [2, 4]. Theories including “crosstalk” between trigeminal and vestibular nuclei, or dysfunctional ion channel and neurotransmitter release have also been suggested [4].
Childhood vestibular migraine
It should be noted that the IHS do recognise childhood vertigo in the form of benign paroxysmal vertigo of childhood. It is most probably a precursor to VM. Many of these children go on to develop migraine, and have a strong FH for migraine [4].
Clinical presentation
The clinical features of MV are highly variable. In addition MV is associated with BBPV and has an overlap with Ménières disease (MD) [5]. However there are many common features which point towards this diagnosis when a high index of suspicion is present.
As with all patients presenting to our clinics it is important to distinguish vertigo from dizziness of non-vestibular origin. The key finding is the illusion of movement, rotational or otherwise.
The rotational vertigo in MV can vary from a few minutes to many hours, overlapping with the characteristics of MD. These symptoms are often spontaneous, but may be preceded by an aura. Unlike the majority of MD patients the attacks can occur every consecutive day, or more than once during a day.
Some patients also describe positional symptoms and it should be noted that these conditions co-exist in many. The attacks may be many weeks or months apart and recovery is also variable. Some patients feel off balance for days or weeks after an attack, distinctive from the MD patients who usually feel better the day after an attack than the day before.
Migrainous headache does not have to occur with the vertigo, it can precede it by many years or occur before or during the vertigo. Other migrainous aura symptoms should however be present in association with the vestibular symptoms when headache is absent. Specific enquiry for photo, phono, osmophobia or visual disturbance is necessary [2, 4].
Fluctuating hearing loss and tinnitus are sometimes seen, but probably relate to the overlap of this diagnosis with MD. Progressive hearing loss is not considered a feature of MV [4].
Migraine sufferers are often aware of trigger factors and this may apply to MV too.
Examination findings
This will often be normal at presentation. Some patients will demonstrate directional preponderance or caloric hypoexcitability. Nystagmus may be demonstrated when the patient is symptomatic, and may have both positional and central features [2]. Testing shortly after an attack may reveal significant asymmetries, but small deficits may be persistent [6].
Treatment
Treatment involves lifestyle changes, dietary modification and medication. Over 50% of patients are aware of specific trigger factors. Lifestyle triggers include poor sleep patterns, exhaustion, stress, hormonal changes and motion sensitivity. These factors should be addressed as best as possible.
Dietary modification has been more successful in treatment of MV than of headache per se. The common trigger food stuffs: cheese, chocolate, caffeine, red wine, citrus fruit and yoghurt together with very high salt food stuffs should be avoided for a period of a few weeks. They can gradually be reintroduced, ideally individually.
Medical therapy for migraine is a complex area and interested readers should consult Eggers [3] for a more detailed consideration. Prophylaxis is the aim, taking anti-migrainous treatment to abort vertigo is not usually successful.
The most commonly used prophylaxis drugs are [3, 7]:
- Beta- blockers. Propranolol in doses from 20mg BD to 80mg BD.
- Amityiptyline starting at a low dose of 10mg nocte. Most patients can be managed at 10-20mg nocte, but higher doses may be used.
- Pizotifen starting at 500mcg per day rising to 1.5mcg per day.
- Calcium channel blockers.
- Anti-epileptics, especially Lamotrigine.
- Topiramate.
As otolaryngologists we may wish to liaise with our neurology colleagues for the more unusual treatments, but the majority of patients are well controlled with low doses of the more commonly used medications.
Conclusion
With a lifetime prevalence of 1% migrainous vertigo is one of the most common conditions that an otologist will see. Most patients will seek specialist medical advice so it is necessary for us to be aware of the diagnosis and be able to manage the majority of cases within our clinics. Patients with difficult migraine will benefit from joint care with a migraine clinic where novel and new therapies may be used, but this is rarely necessary. Response to treatment is very good and this patient group are universally very grateful for having their disrupted lives returned to normal.
References
1. HIS Classification ICHD-II. Available from
http://ihs-classification.org/en/02
_klassifikation/02_teil1/01.00.00_migraine.html
(last accessed 7 October 2015).
2. Neuhauser H, Lempert T. Vestibular migraine. Neurol Clin 2009;27:379-91.
3. Neuhauser HK, Radtke A, von Brevern M, et al. Migrainous vertigo: Prevalance and impact on quality of life. Neurology 2006;67:1028-33.
4. Eggers SDZ. Migraine-related vertigo: Diagnosis and treatment. Current Neurology and Neuroscience Reports 2006;6:106-15.
5. Murofushi T, Ozeki H, Inoue A, Sakata A. Does Migraine-Associated Vertigo Share a Common Pathophysiology With Meniere’s Disease? Study With Vestibular-Evoked Myogenic Potential. Cephalalgia 2009;29:1259-66.
6. Çelebisoy N, Gökçay F, Şirin H, Biçak N. Migrainous Vertigo: clinical, oculographic and posturographic findings. Cephalalgia 2007;28:72-7.
7. Baier B, Winkenwerder E, Dieterich M. “Vestibular migraine”: effects of prophylactic therapy with various drugs. Journal of Neurology 2009;256(3):436-42.
Further reading
Practical Management of the Dizzy Patient , Joel Goebel , Lippincott Williams & Wilkins; 2008.
Declaration of competing interests: None declared.