Less than 4% of doctors on the UK’s medical register describe their ethnicity as African or part African, yet there are myriad driving forces behind the migration of medical trainees from Africa to the UK and other developed countries. Ekpemi Irune tells us about her experience as a British surgeon of Nigerian descent.
Introduction
Of the 288,507 doctors registered with the General Medical Council here in the UK, only 9,946 describe their ethnicity as Black African or mixed race with White and Black African heritage. This equates to about 3.45 %. Without taking into consideration the potential for dual nationality, the GMC register holds 3653 Nigerians; 2642 South Africans; 2330 Egyptians and 1086 Sudanese doctors amongst several other nationalities of the world.
It is however worth mentioning that over 77,000 doctors registered are of an unspecified nationality [1]. The numbers above shed some light on the current state of the medically trained African migrant work force within the UK. I share with you my perspective on migration in medical training as a British surgeon of Nigerian descent.
The historical phenomenon of Africans (and individuals of other nationalities) emigrating to the UK to undertake some form of medical training and / or practise is well documented. The creation of the West African College of Surgeons in the early 1960s was a stimulant for collaboration between the Western world and a developing nation to bring high quality medical training within touching distance of young, talented and eager Nigerian doctors. Through arrangements between the African College and the Royal College of Surgeons at the time, local doctors could travel to the UK to partake in a structured post graduate residency training programme.
Some individuals were awarded bursaries which mitigated the financial burden of the travelling doctor. Anecdotal evidence from speaking to practitioners in Nigeria who experienced this journey suggests that the majority of doctors returned to complete higher surgical training and / or went on to become qualified consultants, contributing to the Nigerian health economy and health education system. More sombre reasons for migration of medics out of Nigeria are explained by the civil war (also known as the Biafra war) which raged between 1967 and 1970.

Figure 1. Operating with my colleague on a West African College of Surgeons Outreach Mission
trip to Lomé, Togo, March 2013. (Centre Hospitalier Universitaire, Sylvanus Olympio.)
In the 1980s, the prevalence of military rule in Nigeria, plagued with multiple coups d’etat, civil disruptions and stunted fiscal growth acted as an unchecked drive for even more migration. In the early 1990s, the migration of skilled medical professionals was economically overwhelming with major institutions in the country losing their finest physicians and surgeons to the United States, the UK and also the United Arab Emirates. This ‘brain drain’ significantly damaged a once thriving and evolving healthcare system. Some of these doctors emigrated with families and others left loved ones behind. All were united in a desire to work unencumbered by politics, sparse resources and nepotism. The rewards were numerous and the financial gains immense.
As recently as the early 1990s, standards of medical training in Nigeria were thought to be high enough such that doctors that had completed their Junior Housemanship year, could immediately transition and commence working within the British healthcare system as trainees. This was contingent on being able to provide valid certification and satisfactory references. These very advantageous circumstances were gradually replaced by the mandatory Professional and Linguistic Assessments Board (PLAB) examinations by the mid-1990s. These were a test of medical knowledge as well as written English that served to standardise the quality of immigrant doctors being assimilated into the British healthcare system.
It takes about seven years to complete an undergraduate medical degree in Nigeria. This schedule is made even more protracted by disruption to the university and school calendars as a result of political unrest, employee strikes, economic turmoil, etc. During such incidents, universities are essentially shut-down, lectures are unable to proceed, examinations are suspended and in some cases, newly matriculated students experience delays in starting medical school. A paucity of qualified lecturers and teaching aids, and delays in remuneration of bursaries and salaries also adversely affect the ability of the universities to provide medical education to willing students.
Another group of migrants stemmed from upper and middle class parents seeking a more predictable and coherent university education for their children. This resulted in hoards of young 17+ year olds being bundled off to the UK and the USA to attend boarding schools, sixth form colleges and then on to medical school. Sure enough, I found myself being shipped off to the UK to join my sisters who were already at university only a week after graduating from high school. I spent the summer holidays in blissful ignorance of what lay ahead: the gruelling task and utter injustice (to my mind at the time) of A’ levels, having already suffered the trials of O’level examinations back in Nigeria.
On healthcare in Africa
The 2014 African regional health report states the following as being crucial for a functioning health system: leadership and governance, human resources, health financing, information and research, access to medicine and health technologies and service delivery [2]. These key components are somewhat lacking in Nigeria. In actuality, the availability and quality of healthcare varies vastly across the continent. Countries such as South Africa are capable of providing high quality trauma, emergency and elective care within hospitals located in the major cities such as Johannesburg.
In comparison, Nigeria still struggles to provide robust healthcare to its over 182 million inhabitants [3], though it continues to make inroads into the expansion and improvement of the healthcare sector. A significant proportion of these advances are being propelled by a multitude of doctors, nurses and allied professionals returning to the country. Some return on a recurrent, intermittent, short-term basis while others have taken the plunge; relocating mind, body, family and all material possessions to the large bustling cities of Lagos and Abuja, for example. “More grease to their elbows,” I say!
The very slow recovery of the health sector in Nigeria breeds a trepidation at the thought of returning harboured by most migrant doctors living overseas. In addition, I and others like me in the UK have settled into society and form an integral part of the National Health Service, contributing to medical education, health policy, etc. Some have families, private practices, other business interests and / or pursue public office. Some of us have dual nationality and over the years our roots have taken firmly in the fertile ground of the UK and thus, we are unlikely to return without considerable thought. In short, the UK has become ‘home’.
One cannot overstate the daunting reality of relocating from an orderly, structured and functioning health system such as the NHS (for all its faults) to a chaotic, poorly resourced environment such as the Nigerian healthcare system. This begins with the personal cost of relocating: ENT practice does not lend itself easily to this endeavour. The infrastructure and equipment required necessitates an immense capital investment in addition to the support team and specialist medical service industry that shore up the practice of any surgeon.
In essence, one requires access to a fully functional hospital with critical care facilities, trained nursing and administrative staff, diagnostic and interventional radiology – high quality CT, MRI and ultrasound services, anaesthetists, pathologist, radiologists, endoscopic solutions, complex microscope devices, powered instruments and consumables, surgical sets with appropriate sterile support services, drugs, and other professionals allied to medicine that constitute the multidisciplinary team essential to delivering robust clinical care.
Unfortunately, Nigeria is lacking a number of the above prerequisites. Furthermore, one mustn’t forget the bureaucracy associated with the day-to-day running of any business in a developing country, which is further complicated by corruption. Despite these challenges, our colleagues present ‘on the ground’ in Nigeria continue to do battle with the powers that be, making strides as best possible to overcome these issues. From these efforts have sprung multiple diagnostic centres, clinics, hospitals, unique standalone ambulatory and critical care units with outreach services to partner hospitals, surgical and medical training seminars and programmes, etc.
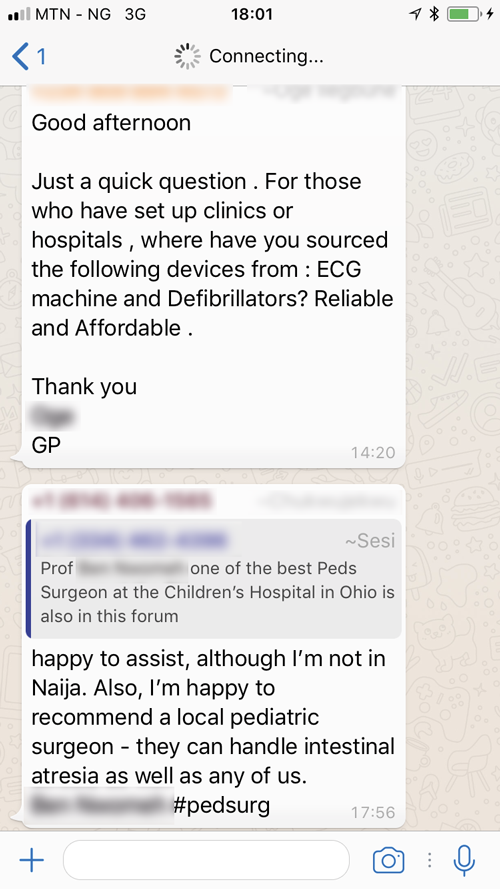
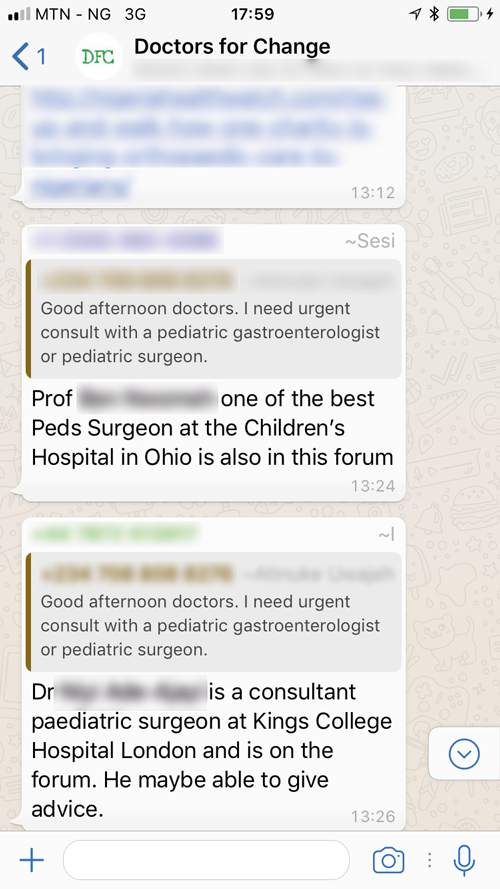
Figure 2. Doctors for Change Forum. Using social media to further medical care.
Technology has also contributed to these and other skill improvements in the health sector. For example, the use of mobile phone technology to contact and spread crucial health alerts, messages, advice to citizens and personnel across the country, especially during epidemiological disasters has been priceless. This application is best referenced by the expedient containment of the Ebola virus outbreak in Nigeria between 20 July (when the first index case was identified) and 20 October 2014 (when Nigeria was declared free of Ebola virus transmission) [4]. The ubiquitous use of social media to promote high quality healthcare is fantastically demonstrated by the workings of a WhatsApp group, of which I am privileged to be part. Aptly named ‘Doctors for Change’, it was started in 2017 by Dr Seyi Oyesola, a Nigerian born British trained consultant anaesthetist who emigrated to the UK in 1990 under a programme between the WACS and the then RCS (he reminds me that he didn’t need to sit the PLAB exams).
Now fully resident in Lagos, Nigeria, Dr Oyesola oversees this multi-specialty group consisting of over 150 overseas trained Nigerian medical doctors either still in the diaspora, partially or entirely stationed in Nigeria. Through this medium, doctors can link each other with a wide array of skilled practitioners to facilitate the management of patients in the country. Clinical cases are discussed without compromising patient confidentiality and a multitude of recommendations, referrals and advisory comments are exchanged to optimise patient care, access to the limited resources in the country and to shed light on those facilities that remain obscure. This forum has inspired many a discussion on how the Nigerian healthcare system can be improved upon, from developing and supporting health initiatives, influencing policy, providing training to local doctors, the organisation of conferences and even charitable surgical missions.
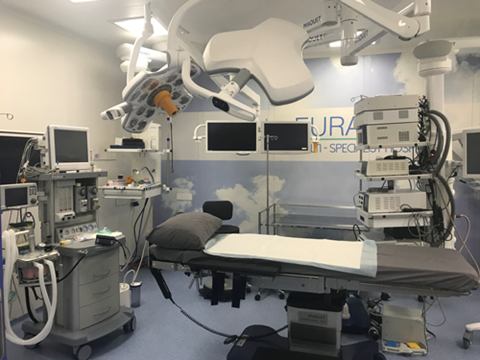
Figure 3. Theatre at the Euracare specialist facility in Lagos, Nigeria, January 2018.
The fact remains that the hostility of the Nigerian healthcare and economic landscape makes it difficult for one to wholly invest in the African dream of “(quality) health care for all”, yet I see that the brave among us prodigal sons (and home-grown physicians) are taking on the mantle to bring this ideology to reality. Indeed, it makes me proud to call myself British as well as Nigerian.
References
1. General Medical Council. List of Registered Medical Practitioners – statistics. Available at
https://www.gmc-uk.org/
doctors/register/search_stats.asp
(last accessed 26 January 2018).
2. Sambo LG, Harris M, Beveridge M. The health of the people: what works. African Regional Health report. 2014; Brazzaville, Republic of Congo, World Health Organization, Regional Office for Africa.
3. United Nations. World Population Prospects: Key findings and advance tables. 2015 Revision. 2016; United Nations Department of Economic and Social Affairs / Population Division. Available at:
https://esa.un.org/unpd/
wpp/publications/files/key_findings_wpp_2015.pdf
(last accessed 26 January 2018).
4. World Health Organization. One year into the Ebola epidemic: a deadly, tenacious and unforgiving virus. 2015; Geneva, Switzerland, World Health Organization. Available at
http://www.who.int/csr/disease/
ebola/one-year-report/introduction/en/
(last accessed 26 January 2018).
Summary
-
The main driving force behind the migration of medical trainees to the UK or other
developed countries is the inability of the local country to provide timely, robust medical training under favourable economic circumstances.
-
The main hindrance to qualified individuals returning permanently to their native land is the lack of a functioning heathcare system within which to practise and an aversion to ‘getting stung’ whilst trying to help shore it up.
-
Some of us have dual nationality, and over the years have put down roots in the UK and thus, are unlikely to return without considerable thought.




