Robotic technology in ENT surgery has been used in certain areas of head and neck cancer care but, in this article, we hear of an exciting development from the team at Guy’s & St Thomas’.
Advances in surgical robotic technology have the potential to enhance surgical precision and control in order to improve clinical outcomes. Robotic applications still remain limited to certain specialties such as urology, gynaecology, thoracic surgery and head and neck surgery.
In addition, due to the high cost and complexity of training surgical teams, these systems have not yet disseminated to a wider audience. In orbital surgery, this is even more apparent, as robotic applications have not been developed and current established robotic systems are not specifically designed for orbital work.
Orbital surgery presents a unique challenge for robotic surgical innovation. The orbit is a small, highly vascularised, cone-shaped cavity with close relations to the skull base and paranasal sinuses. For advanced tumours invading the orbit, achieving clear margins has shown a survival benefit for all cases. Orbital exenteration, a radical clearance of the orbital cavity and contents, remains the main oncological surgical procedure of choice. Orbital exenteration for advanced cancer is a highly morbid treatment and, as such, there is significant potential to develop orbit-sparing cancer surgery in this area and also reduce associated morbidity and complications.
The head and neck surgical oncology team at Guy’s & St Thomas’ (GSTT) Hospital London and Moorfields Eye Hospital (MEH the National Eye Hospital, London) have developed a large ocular oncology practice and have performed over 100 orbital exenterations for primary ocular malignancies. Our results show a five-year overall survival rate of 65% for advanced stage cancers [1].

Figure 1: Dry lab initial setup with skull to determine configuration.

Figure 2: Console display showing HD enhanced surgeon view.
Guy’s & St Thomas’ Hospital has one the largest robotic programmes in the UK, utilising seven robots across several different surgical specialties. This project also collaborates with the surgical and interventional engineering department of King’s College London. The purpose of this research project is to develop the feasibility of robotic assisted orbital surgery (RAOS) in clinical practice and develop an optimised surgical configuration. The initial dry lab experiments involved a skull, and we deployed the da Vinci XI system (Intuitive Surgical, California, USA) in order to see if robotic surgery could be carried out successfully around the orbit. We optimised the setup and instrument orientation and determined feasibility of the project (Figures 1 and 2). The next step involved a series of wet lab cadaveric dissections in which we then utilised the Versius (CMR Surgical, Cambridge, UK), a next-generation CE marked robotic surgical system, in order to further determine feasibility and understand the possibility of application to periorbital surgery [2].
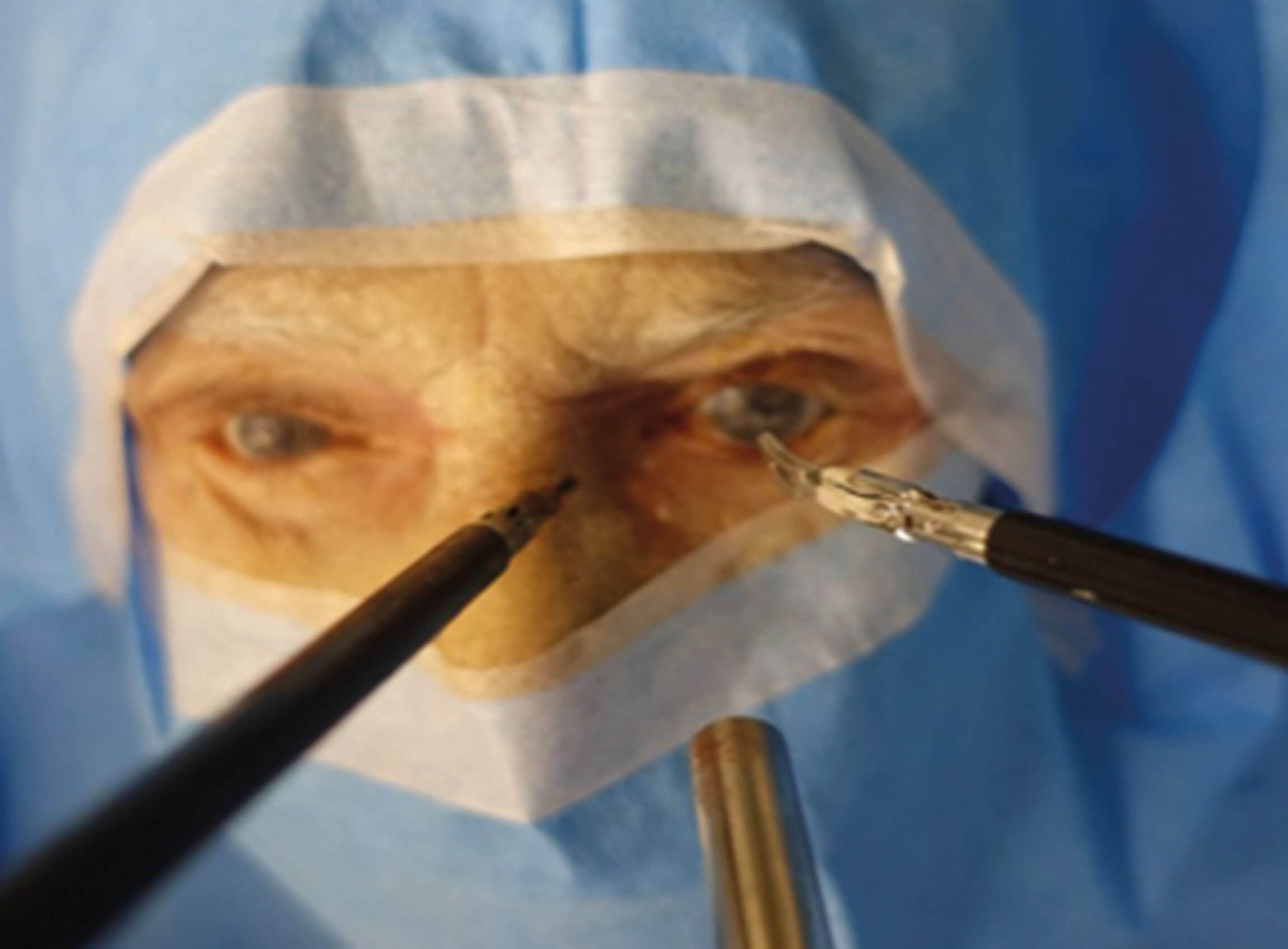
Figure 3: Wet lab using CMR robot to perform RAOS on cadaver.
We determined three index procedures: medial canthus dissection, lateral canthus dissection (including excision of lacrimal gland) and orbital exenteration. All three procedures were successfully carried out and instrument optimisation was developed (Figure 3).
Having successfully carried out these experiments, our aim was to translate this into clinical practice and perform the first clinical RAOS. This long and complex process involved detailed applications through ethics, governance and, finally, approval by the Trust Risk and Assurance Committees. Approval was granted last year, and we generated patient information leaflets and specialised research consent forms in order to provide potential patients with appropriate information. We then had to seek a suitable candidate for this first case. This was set up as a pilot study clinical evaluation rather than a phase 1 clinical trial. Suitable patients would be those with periorbital cancers selected for orbital exenteration whereby RAOS could potentially remove the tumour, preserving the eye.
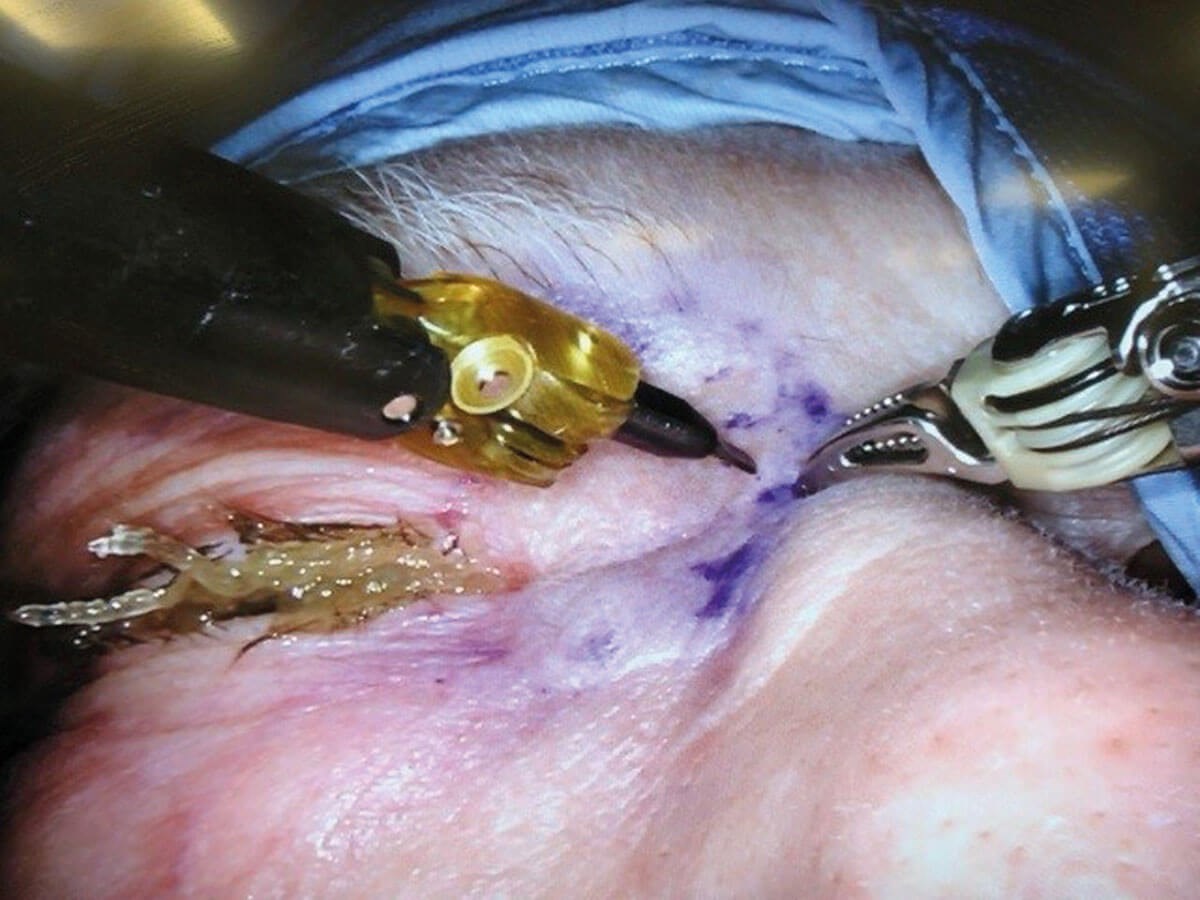
Figure 4: RAOS first in man case on 85-year-old woman with recurrent BCC of medial canthus.
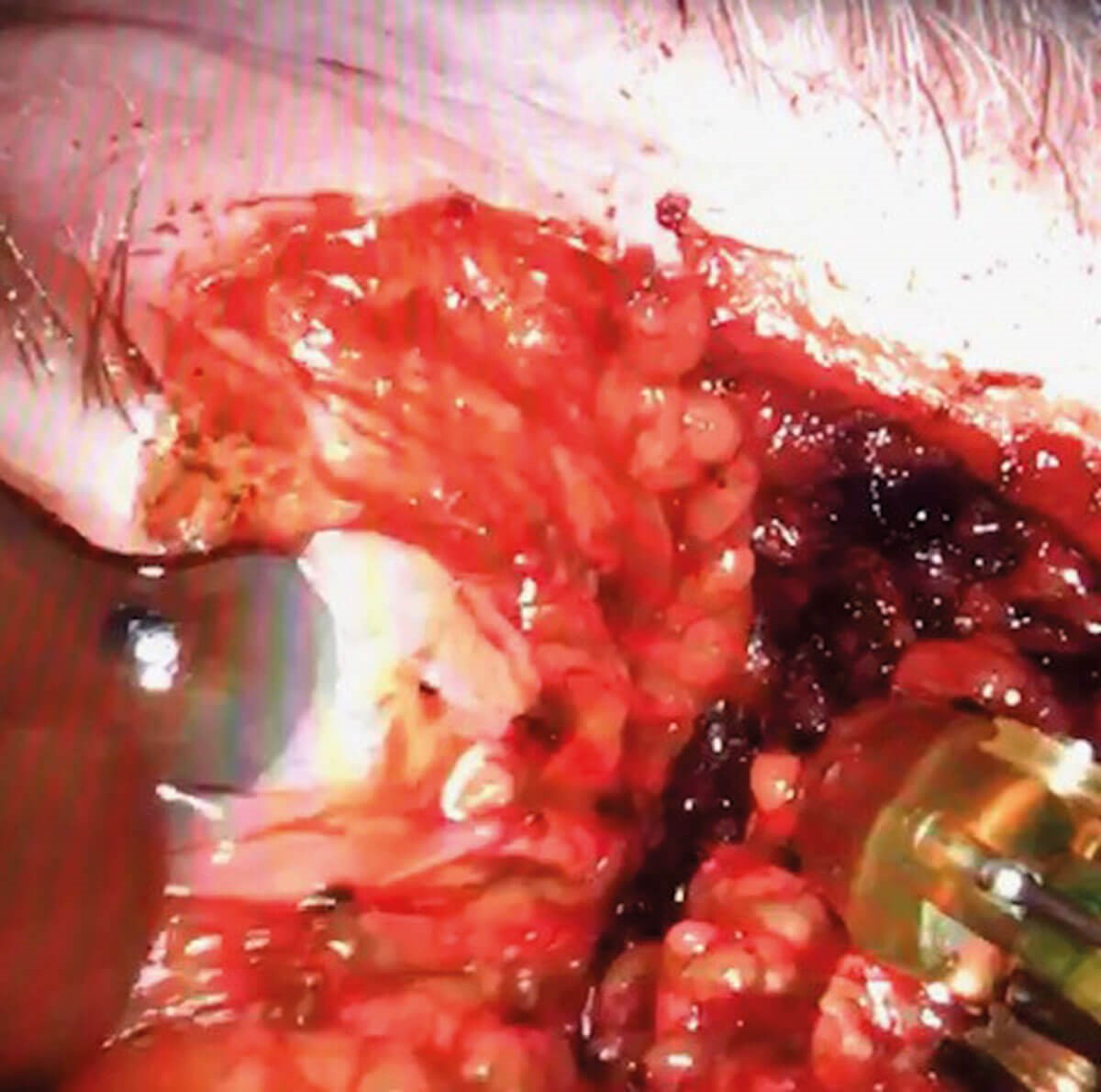
Figure 5: RAOS first in man case showing surgeon’s console view.
Mrs IM is an 85-year-old woman who presented with a recurrent infiltrative basal cell carcinoma (BCC) of the medial canthus of the right eye. She had previously undergone a wide local excision with close excision margins, followed by Mohs micrographic procedure and radiotherapy. The MDT at MEH had recommended orbital exenteration. We offered RAOS as a novel alternative to excise the tumour and preserve the eye.
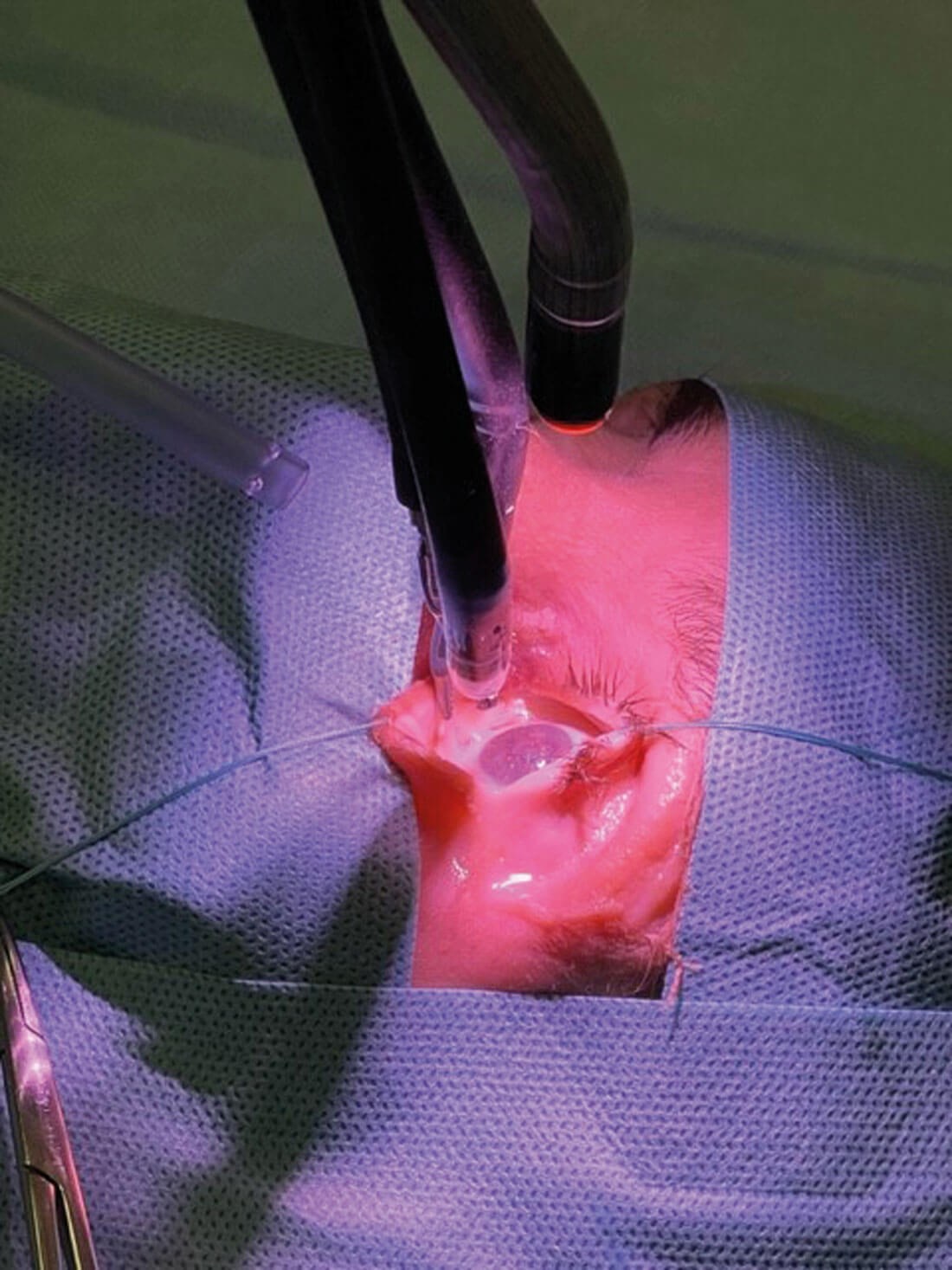
Figure 6: Wet lab cadaveric experiments using da Vinci Single Port System to perform RAOS.
We used the da Vinci Xi system to clear the tumour whilst preserving the orbit. The procedure was performed with the Xi system. A wide local excision was performed using the robot, a skin incision was made, the medial canthal ligament was divided and dissection was taken down to the medial orbital wall with exposure of the lacrimal crest. An en-bloc resection of the specimen was performed. During the surgery we did not detect any arm clashing or any orbital trauma as a result of the robotic arms. The patient made an uneventful recovery and was discharged on the next postoperative day. We understand that this is the first time that the da Vinci robotic system has been applied for orbital malignancy surgery.
Since then, we have successfully carried out RAOS in three more patients. In all cases, orbital preservation was achieved when they were initially selected for orbital exenteration.
As part of ongoing research to develop this surgery, we have worked with Intuitive Surgical to utilise the next generation single port (SP) to perform ROAS successfully in a wet lab. This new system shows significant improvements on existing systems as it allows an even greater degree to operate around corners. In our opinion, the da Vinci SP system offers improved capabilities when applied to the orbit.
Recently we have secured £250,000 from Guy’s & St Thomas’ Charity to fund a PhD project to formally explore the possible applications of RAOS in order to understand the applications and limitations of existing robotic platforms to orbital surgery and to devise what would be the optimal robotic system for orbital surgery. This project has been a collaborative effort between expert clinical groups working across different NHS and academic organisations (GSTT, KCL and MEH) along with industry partners (Intuitive and CMR). We have demonstrated proof of concept that RAOS can be performed to treat orbital tumours and potentially avoid exenteration, but significant product technological development is needed in order to facilitate a wider adoption of robotics to orbital surgery.
Robotic assisted orbital surgery represents an exciting new development and a cutting-edge innovation in surgical research in the field of orbital surgery. We feel that robotics could be applied to skull base surgery, neurosurgery, otology and rhinology to improve access and improve outcomes in the future.
References
1. Fleming JC, Morley I, Malik M, et al. Orbital exenteration and reconstruction in a tertiary UK institution: a 5-year experience. Orbit 2021;40(4):306–15.
2. Faulkner J, Naidoo R, Arora A, et al. Combined robotic transorbital and trans nasal approach to the nasopharynx and anterior skull base: Feasibility study. Clin Otolaryngology 2020;45(4):630–3.
3. Jeannon JP, Faulkner J, Uddin J, et al. Robotic assisted orbital surgery (RAOS)—A novel approach to orbital oncology surgery. Eye (Lond) 2023;37(5):1040–1.
Declaration of competing interests: None declared.
Acknowledgements
This work has been supported by a grant from the Guy’s & St Thomas' Head and Neck Research Fund.The PhD study grant has been supported by The Charles Wilson and Rowena Williams Research Foundation.
We would like to thank Dr Mark Slack from Cambridge Medical Robotics (CMR) who supported some of the wet lab research.
GSTT/MEH RAOS ocular oncology research team also includes:
Asit Arora, Claire Daniel, Jimmy Uddin, Jack Faulkner, Moshan Malik, and Hubert Stein.









