In this article, Hannah North and Simon Lloyd give us an overview of the complex condition of superior semicircular canal dehiscence (SSCD) syndrome, including diagnosis, treatment and management.
Superior semicircular canal dehiscence (SSCD) is a bony defect of the otic capsule at the apex of the superior semicircular canal (SSC). Whilst such a defect is identifiable in up to 9% of temporal bones on CT, it is estimated that only 0.1% of the general population and 0.6% of patients in a specialist otology centre have symptoms or signs related to it.
The true aetiology remains unknown; originally it was thought to be triggered by trauma or barotrauma but it is now thought to be related to gradual thinning of bone of the middle cranial fossa over the SSC, although in most patients there is no definite date of onset [1, 2].
The constellation of clinical features associated with SSCD were only described for the first time in 1998 by Minor et al. [3]. The vestibular and auditory symptoms and signs are related to both the creation of a ‘pathologic third window’ in the otic capsule and the contact between middle cranial fossa dura and the inner membranous tissue of the SSC.
“Only when patients are severely affected by disabling vestibular symptoms should surgery be contemplated.”
Vestibular manifestations are most likely the result of a lowered impedence in the vestibular system allowing for stimulation following pressure and sound transmission, most commonly seen as oscillopsia or true vertigo following loud noises (Tullio phenomenon) or pressure in the ear canal (Hennebert’s sign). Some patients present with a chronic dysequilibrium that does not appear to be the result of sound or pressure. Auditory manifestations are the result of dissipation of acoustic energy into the cranial cavity producing a relative conductive hearing loss.
The detection of self-generated body sounds via bone is facilitated by the dehiscence and is called autophony [4]. The middle cranial fossa dura in contact with the membranous SSC can produce pulsatile tinnitus. Clinical examination reveals normal otoscopy. Valsalva may increase intracranial pressure thereby exacerbating the middle cranial fossa contact with the dehiscent SSC causing excitatory stimulation (ampullifugal) resulting in nystagmus and acute vertigo. Minor has followed a series of patients in detail. Of 60 patients, 90% had vestibular symptoms induced by sound, 73% had vestibular symptoms induced by pressure, and 67% by both [2]. Fifty-two percent had CHL and 60% had autophony. Eight percent presented with only audiological symptoms. Identification requires a high index of suspicion as symptoms may be subtle and poorly characterised by patients.
“SSCD is a rare clinical entity that classically produces pressure or sound induced vertigo, autophony and a conductive hearing loss.”
Investigations should include an audiogram, often with a low frequency conductive hearing loss (CHL) but without the nadir at 2kHz seen in middle ear causes of CHL. Stapedial reflexes are normal helping to exclude otosclerosis. Vestibular investigations including calorics and electronystagmography (ENG) may help to exclude other differential diagnoses such as Ménière’s disease. Pressure and sound can produce nystagmus, easier to visualise with Frenzel glasses. This is usually in the direction of stimulation of the SSC and is usually torsional and in an upwards direction [5].
Cervical VEMP (cVEMP) and ocular VEMP (oVEMP) studies are very helpful. Traditionally cVEMP has been used. This is a short latency reflex following sound stimulation of the saccule via the medial vestibulospinal tract causing inhibition of the contraction of the ipsilateral sternocleidomastoid muscle (SCM). Tone bursts at 500Hz are applied for 7msec repeated at five per second. This is repeated 100-200 times and an average of the action potential of the tonic contraction of SCM in measured. Normally, at a 13msec and 23msec, a positive and negative waveform (p13 and n23) are seen above a threshold of about 90dB.
This usually has an amplitude of approximately 70mV. In patients with SSCD, the effect of the third window causes the fluid dynamics in the ipsilateral ear to produce a larger amplitude of the wave form on the cVEMP. The relative conductive bony hyperacusis causes the cVEMP to occur at a much lower threshold at about 70dB (Figure 1) [5]. Interestingly when the cVEMP is performed by bone stimulation directly on the skull and bypassing the middle ear, it is normal in appearance. This is in keeping with the third window effect. The contralateral ear, if clinically unaffected, will be normal.
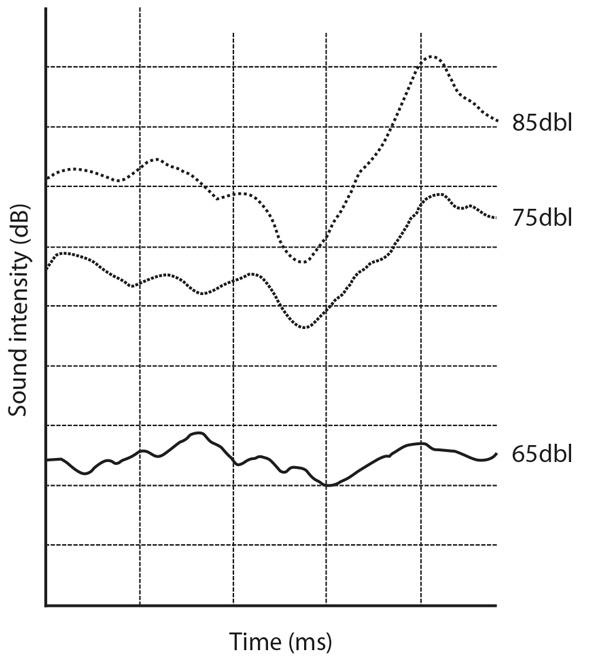
Figure 1: Abnormal cVEMP showing a reduced threshold of 70dB.
More recently the oVEMP has been studied [5]. This is an excitatory stimulus of the contralateral inferior oblique muscle measured using electromyelography of the muscle following sound stimuli. The pathway is via the otolith organs to the vestibulocular pathway, rather than via the saccule to the vestibulospinal pathway. Normally a negative waveform is seen at 10msec and a positive waveform is seen at 16msec (n10 and p16 respectively). At 500Hz, an n10 amplitude of ≥ 8.25µV has been shown to be 100% sensitive and 100% specific for SSCD demonstrated intraoperatively.
Computed tomography (CT) is the imaging modality of choice and is able to identify dehiscence, particularly if 0.5mm slices with reconstruction in Poschel and Stenver’s view (parallel and orthogonal to the direction of the SSC) are used (Figure 2). Scan findings must, however, be assessed in conjunction with clinical features because of the presence of dehiscence in asymptomatic individuals.
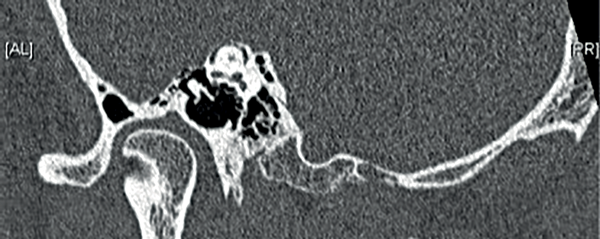
Figure 2: A high resolution oblique coronal reconstruction CT scan of the temporal bone
clearly demonstrating dehiscence of the superior semicircular canal.
Management depends on the type of symptoms and their severity. Most patients have mild symptoms and may be managed conservatively in the knowledge that there is no sinister pathology present [2]. Even in specialised otology centres, the reported rate of conservative management is between 48% to 86% [6]. In patients with disequilibrium related to loud sounds, avoidance and the use of earplugs is recommended. For patients with pressure induced vestibular symptoms, myringotomy and ventilation tube insertion may be sufficient to control their symptoms [2]. Only when patients are severely affected by disabling vestibular symptoms should surgery be contemplated.
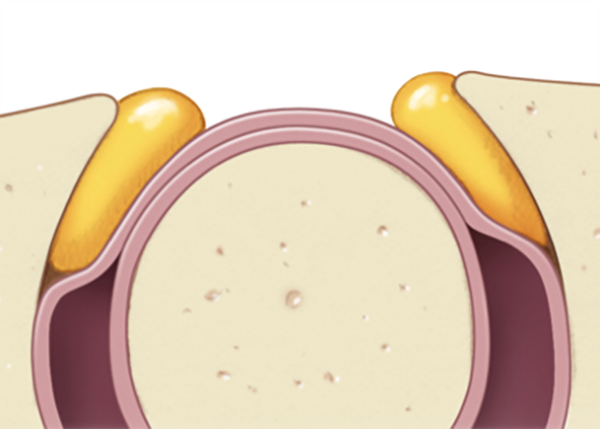

Figure 3: Top) Obliteration of the superior semicircular canal.
Bottom) Resurfacing of the superior semicircular canal.
The aim of surgery is to either cover the defect or to obliterate the SSC (Figure 3). The approach to the SSC is either through middle cranial fossa or transmastoid. Proponents of middle cranial fossa surgery argue that there is better visualisation of the arcuate eminence to confirm diagnosis and confirm coverage / closure. They also suggest that the risk of neurosurgical complications related to craniotomy and temporal lobe retraction is low. Several groups state that this is their approach of choice [6]. Alternatively, the transmastoid approach is one more familiar to otologists and avoids the risk of intracranial complications. Its main disadvantage is the visualisation of SSC along the tegmen, particularly if the tegmen hangs low. Many groups describe good success with the transmastoid approach [7, 8].
“A high index of suspicion is essential for accurate diagnosis”
Aside from the approach, several different methods of addressing the SSC have been described. There may be a lower rate of recurrence with occlusion and resurfacing compared with resurfacing alone [2]. Some groups have, however, had good success with resurfacing alone particularly when bone pate and fascia are used to create a smooth covering over the length of the dehiscence [6]. Failures of resurfacing alone have been associated with the use of a bone plate that has dislodged with time [2]. It is possible that resurfacing does not obliterate the third window effect completely and hence some symptoms may remain.
Canal occlusion is undertaken in a similar manner to that for posterior semicircular canal occlusion used for intractable benign positional vertigo (Figure 4). The use of bone wax, bone pate and temporalis fascia have all been described although bone wax may be the most effective. The occlusion material is placed either side of the bony defect via a fenestration into the crura of the SSC. This prevents fluid movement inside the canal.
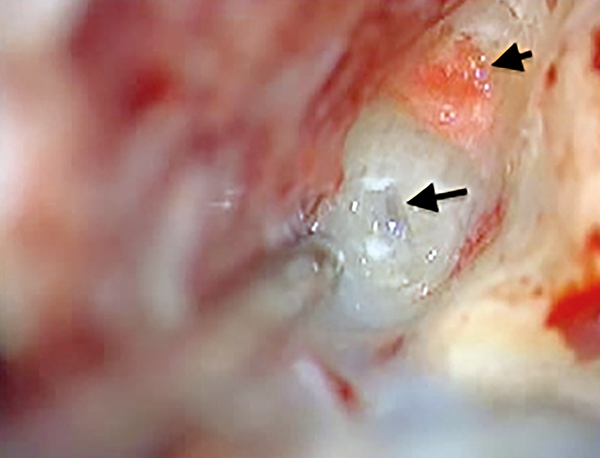
Figure 4: Intra-operative photograph demonstrating obliteration of the anterior crus of the superior semicircular canal (short arrow) and fenestration, prior to obliteration, of the posterior crus of the superior semicircular canal (long arrow).
Symptom control is achieved in 92-94% of cases with no statistical difference between surgical approach [9]. All SSC surgery is associated with a risk of sudden complete sensorineural hearing loss. In a recent systematic review including 150 published operative cases, the risk of this is in the region of 4% [9]. The rate of minor complications including benign positional paroxysmal vertigo, transient disequilibrium and transient hearing loss is in the region of 7% [9]. In summary, SSCD is a rare clinical entity that classically produces pressure or sound induced vertigo, autophony and a conductive hearing loss. A high index of suspicion is essential for accurate diagnosis. Surgical treatment of more severe forms has a high success rate with only a small risk of labyrinthine compromise.
References
1. Elmali M, Polat AV, Kucuk H, Atmaca S, Aksoy A. Semicircular canal dehiscence: frequency and distribution on temporal bone CT and its relationship with the clinical outcomes. Eur J Radiol 2013;82(10):e606-e9.
2. Minor LB. Clinical Manifestations of Superior Semicircular Canal Dehiscence. The Laryngoscope 2005;115(10):1717-27.
3. Minor LB, Solomon D, Zinreich JS, Zee DS. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg 1998;124(3):249-58.
4. Merchant SN, Rosowski JJ. Conductive Hearing Loss Caused by Third-Window Lesions of the Inner Ear. Otology and Neurology 2008;29(3):282-9.
5. Janky KL, Nguyen KD, Welgampola MS, Zuniga MG, Carey JP. Air-conducted oVEMPs provide the best separation between intact and superior canal dehiscent labyrinths. Otology and Neurology 2013;34(1):127-34.
6. Hillman T, Kertesz T, Hadley K, Shelton C. Reversible Peripheral Vestibulopathy: The Treatment of Superior Canal Dehiscence. Otolaryngology-Head and Neck Surgery 2006;134(3):431-6.
7. Crovetto M, Areitio E, Elexpuru J, Aguayo F. Transmastoid approach for resurfacing of Superior Semicircular Canal dehiscence. Auris Nasus Larynx 2008;35(2):247-9.
8. Shaia WT, Diaz RC. Evolution in surgical management of superior canal dehiscence syndrome. Current Opinion Otolaryngology Head and Neck Surgery 2013;21:497-502.
9. Gioacchini FM, Alicandri-Ciufelli M, Kaleci S, Scarpa A, Cassandro E, Re M. Outcomes and complications in superior semicircular canal dehiscence surgery: A systematic review. The Laryngoscope 2015; [Epub ahead of print] doi:10.1002/lary.25662.
Declaration of competing interests: None declared.





