Introduction
Temporal bone injuries represent one of the more complex management problems presenting to the otolaryngologist. This is largely due to difficulties in assessment and the frequent delays in referral, often as a result of other injuries demanding more immediate attention.
With the ongoing involvement of UK forces in overseas operations, as well as the increase in knife and gun crime, the type of temporal bone injury presenting to our unit has changed, and although blunt injuries still predominate, we have witnessed an increase in the proportion with penetrating trauma.
The purpose of this review is to present an overview of the presentation, assessment and management of temporal bone injuries, and their associated complications.
Epidemiology
Approximately 50% of all temporal bone fractures are a result of road traffic accidents, with the majority of the remainder due to falls, gunshot wounds or other head injury [1]. By comparison, 88.6% of craniofacial injuries in active US armed forces personnel were due to explosions, with only 1.7% due to road accident [2]. Alcohol and / or recreational drug use may also play a part in the aetiology and may further complicate the initial assessment.
Types of temporal bone injury
Temporal bone injuries can be classified into blunt or penetrating, and the pattern of injury and associated features varies between them. There exists an overlap between the two types, as many high-velocity penetrating injuries will also cause an associated blunt-pattern effect.
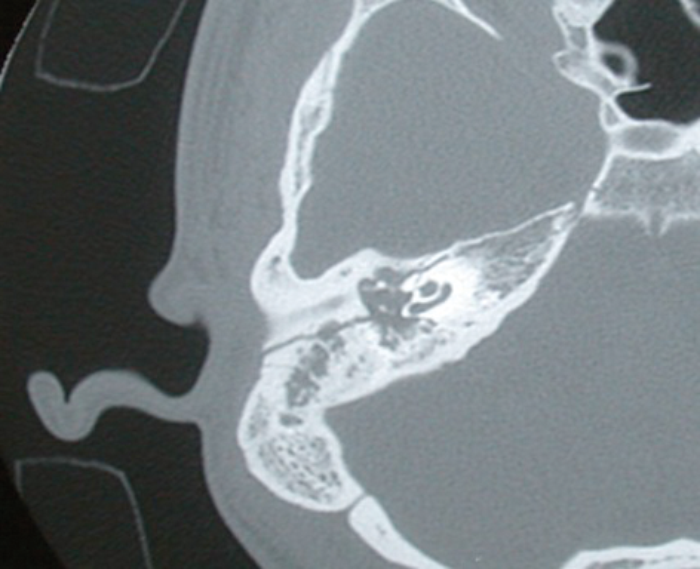
Figure1: Axial CT scan showing a longitudinally orientated fracture line running postero-superior
to the EAC and causing a haemotympanum and disruption to the ossicular chain.
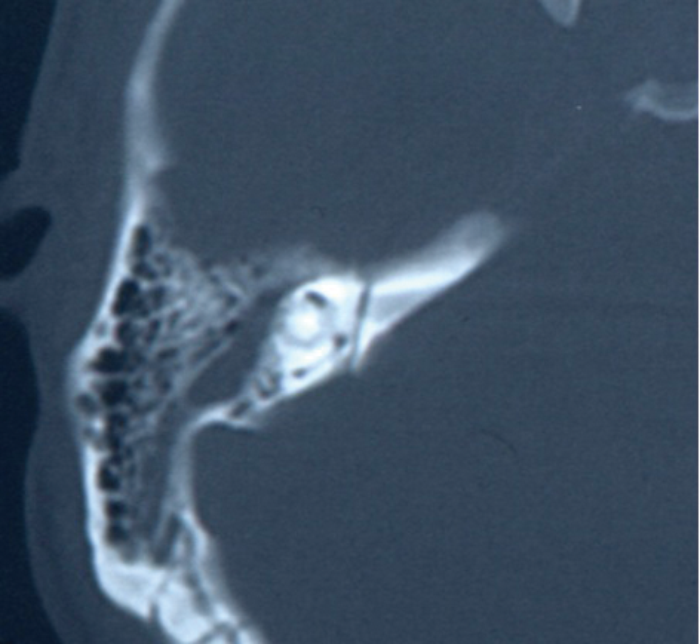
Figure 2: Axial CT scan showing a transverse fracture line running from the posterior
petrous bone across the internal auditory canal (IAC) and medial to the inner ear structures.
Traditionally, fractures have been divided into transverse or longitudinal (Figures 1 and 2). Longitudinal fractures usually arise from lateral blows to the head, with the fracture line following the path of least resistance. Transverse fractures arise from blows to the occipital region. However, numerous studies demonstrated no prognostic value in this classification, with the incidence of true longitudinal fractures rarely occurring, rather an oblique fracture with features of both. More recently, the involvement of the otic capsule (more common in transverse fractures) has been used as a more relevant clinical descriptor, as this allows for the more accurate prediction of associated complications [3, 4].
While this classification is still valid for blunt injuries, the complex injury pattern of penetrating wounds, especially gunshots, requires more detailed description. The complications of bullet (or other penetrating missile) injuries will depend to an extent on the velocity of the projectile. High velocity weapons generally travel in a straight line, and cause the majority of damage via direct injury, cavity formation, heat or bone fragments. Low velocity bullets, however, may be more easily deflected by bone and therefore travel a more unpredictable path, causing extensive damage to soft tissue structures (Figure 3).
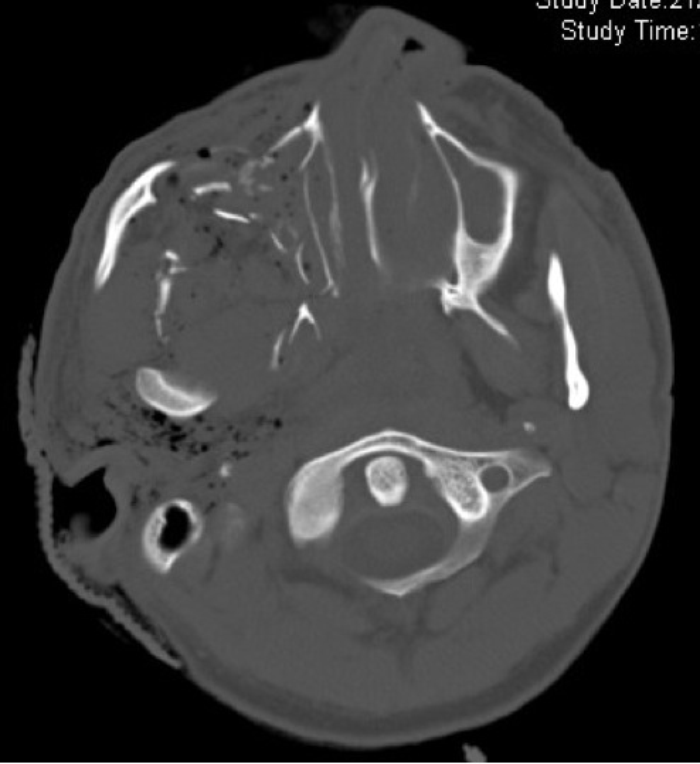
Figure 3: Axial CT scan illustrating a penetrating injury involving the maxilla and temporal bone.
Extensive soft tissue injury, typical of penetrating trauma, below the skull base and associated surgical emphysema is seen.
Presentation
Patients will commonly present acutely, via the Emergency Department or trauma service, following an assault or accident, where the head injury may be the primary insult. Delayed referrals are not infrequent, usually in cases of polytrauma, where the extent of the patient’s injuries require multi-specialty input and stabilisation, and the temporal bone fracture is only picked up on subsequent scanning. In military servicemen / women, the referral may again be delayed due to the need to stabilise the patient from their potentially serious co-morbidities.
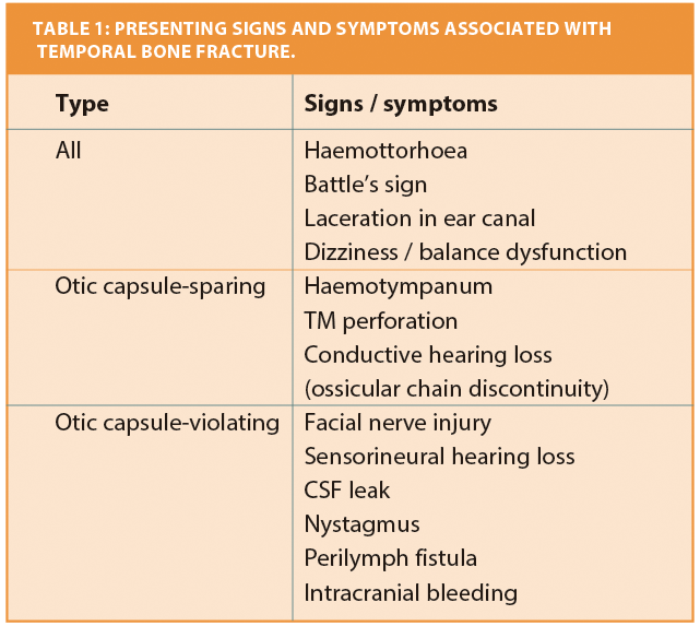
Figure 3: Axial CT scan illustrating a penetrating injury involving the maxilla and temporal bone.
Extensive soft tissue injury, typical of penetrating trauma, below the skull base and associated surgical emphysema is seen.
The common presenting symptoms and signs are shown in Table 1. Generally, a full cranial nerve assessment should be undertaken and documented as soon as possible after the injury. Gunshot wounds are more likely to be associated with non-temporal injuries, such as intracranial or vascular complications, or mandibular fracture [5], and may demand further assessment from other specialist teams.
Investigations
Following stabilisation, all patients should have cross sectional imaging; if possible this should include a high resolution, 0.5 mm slice computed tomography scan of their temporal bones. Fractures are often clearly seen and identification of the fracture pattern may guide the clinician towards specific injuries, particularly in the unconscious or uncooperative patient. Retained foreign bodies may also be visible and guide the surgical approach if necessary.
Magnetic resonance imaging (MRI) is not routinely performed in the case of blunt temporal bone injury, as a computerised tomography (CT) will provide the information regarding the post injury anatomy to allow surgical planning. MRI may be useful, however, in identifying temporal lobe contusions, injuries to cranial nerves, inner ear haematoma and other intracranial injuries for penetrating wounds. Angiography should be considered in all cases of penetrating injury due to the higher risk of injury to the internal carotid artery.
While tuning fork tests may have been done as part of the more acute work-up, formal pure tone audiometry will help differentiate between a purely conductive hearing loss and one with a sensorineural component. This may not be possible, however, often due to the patient’s ability to tolerate the test and indeed travel to the audiology centre. Electrophysiology, looking for neural degeneration may be of value in the later assessment of these cases, beyond 7-10 days, but has little to add in the acute setting.
Management
For the majority of temporal bone fractures, no immediate specific intervention will be required. In a patient with an otic-capsule sparing fracture, with no obvious complications, a conservative management strategy alone is indicated. However, all cases must be assessed individually, with consideration given to the extent of concurrent injuries and the stability of the patient. There are a number of factors and controversies that exist in the management of these patients:
Antibiotics
Antibiotics are not routinely recommended for temporal bone fractures. A recent Cochrane review found no difference in both meningitis rates and all cause mortality in patients receiving prophylactic antibiotics versus no antibiotics / placebo in patients with a basilar skull fracture, either with or without cerebrospinal fluid (CSF) leak [6]. For contaminated penetrating wounds, however, broad spectrum antibiotic prophylaxis may be administered, although there is no high quality evidence to support this.
Hearing loss
Hearing loss following temporal bone injury may be conductive, sensorineural, or mixed. A conductive hearing loss is most commonly due to haemotympanum secondary to fracture line bleeding. There is no role for the drainage of the middle ear in these cases, as the blood will resorb over time. Dried blood within the external auditory canal is a common occurrence and usually due to laceration of the skin of the external auditory canal and may also give rise to a conductive hearing loss, but more commonly will serve to obscure a view of the tympanic membrane. Care must be taken if this blood is removed and it is the authors’ policy typically not to perform microsuction in these cases. The presence of significant haemorrhage from the external canal may signify injury to the jugular bulb or internal carotid artery and should therefore be treated with caution until excluded. Ossicular dislocation / injury may also give rise to a conductive hearing loss (CHL), however this may not be discovered until much later, when any associated haemotympanum has resorbed, and certainly does not require immediate intervention. The most common site is incus dislocation, followed by injury to the stapes superstructure and good results are possible with surgical repair at a later date. CHLs due to penetrating injuries are often more problematic, due to the more destructive nature of the injury and therefore complex injury pattern. Full ossicular chain reconstruction is more often needed, with a lower success rate than for blunt injuries.
For non-penetrating fractures, sensori-neural loss is more commonly associated with a transverse fracture involving the otic capsule, and may be due either to injury to the cochlear itself or cochlea nerve. It is thought that up to 50% of patients with a temporal bone fracture will have an element of sensorineural hearing loss (SNHL), and that this will be persistent. There is no effective active management for this, although in patients with associated vertigo and tinnitus, bed rest, avoidance of straining and head elevation may be advised in case of potential peri-lymph fistula, which may require surgical exploration if symptoms do not settle.
A number of options exist for the long-term rehabilitation of unilateral SNHL following a temporal bone fracture and these include cross aids and bone anchored hearing aids. Currently there is increasing evidence to suggest that cochlear implants provide benefits to these patients and represent the only approach that can restore binaural hearing.
Facial nerve injury
Facial nerve palsy occurs in around 7% of all temporal bone injuries, although this figure rises to around 50% in penetrating fractures [7, 8]. The prompt and accurate grading of any facial nerve injury is essential in order to carry out the most effective treatment. The conscious level of the patient may hamper this, especially if intubation has occurred before a full neurological assessment can be made. Ideally a House-Brackmann score should be assigned, but often for the purposes of decision-making, the grade of injury can be divided into partial or complete, and delayed or immediate.
A partial or delayed onset weakness carries a good prognosis and conservative management is recommended. Immediate onset paralysis is more often associated with a nerve transection or major disruption to the fallopian canal and may warrant early exploration assuming the patient is otherwise stable. Imaging can be critical in determining the status of the fallopian canal in these cases and electrophysiology con-firming degeneration can also be useful.
The difficulty arises when the time of onset is unknown and in these cases other factors such as the status of the inner ear, the co-existence of CSF leakage, the imaging features and electrophysiology are taken into consideration. The sensitivity and specificity of CT in identifying the site and presence of temporal bone fractures is 77.5% and 77.7% respectively, and although this remains the most accurate technique for assessing the anatomic status of the facial nerve any decision regarding exploration must be made taking into account the full clinical picture [9].
In our experience only a very small proportion of blunt injures involving the facial nerve benefit from exploration, however we consider that all or almost all penetrating injuries with immediate or indeterminate onset paralysis should be explored.
The facial nerve may be injured at more than one site, especially in penetrating trauma. Gunshot wounds in particular may be associated with more widespread soft tissue trauma in addition to the bone injury. Any surgeon exploring these cases should be prepared to explore from the internal auditory meatus to within the parotid gland. A translabyrinthine approach is indicated if clinical and radiological evidence suggests cochlea-vestibular injury, while transmastoid or middle cranial fossa approaches are more appropriate where there is no apparent damage to the inner ear.
Intra-operatively, once the site of injury is identified, the nerve can be examined for evidence of retained foreign body, stretching, bruising or transection. If intact, the nerve can be decompressed by widely removing the bone of the fallopian canal and opening the epineurium. Partial transections up to 50% may be repaired by direct suture. Larger transections should be repaired by re-routing and primary anastomosis where possible and by interposition graft, usually from the greater auricular nerve, in instances where primary anastomosis is not possible.
CSF otorrhoea / rhinorrhea
CSF leak complicates up to a third of patients with temporal bone fracture, although in the majority the leak will resolve within five days therefore a conservative approach is warranted at first. In patients with a continued leak, a lumbar drain may reduce the output and aid resolution, although there will be some in whom this is not successful and will require further treatment. If surgery is considered, fluorescein cisternography may aid identification of the site of leak and therefore direct the approach and technique used.
Foreign body
These may take the form of retained bullets, fragments of clothing, or other shrapnel in the case of explosive injuries. These should be removed where possible, and indeed may be a contributing factor to, for example, facial nerve palsy. Implantation chol-esteatoma is a potential sequalae where there is the risk of implanted squames within the middle ear cleft, and in these cases a radical mastoidectomy should be performed.
Summary
Temporal bone injury is a condition associated with significant morbidity, the prompt recognition of which may aid recovery. While many blunt injuries may be managed conservatively, penetrating fractures, such as gunshot wounds, warrant a lower threshold for surgical intervention.
References
1. Ishman SL, Friedland DR. Temporal bone fractures: traditional classification and clinical relevance. Laryngoscope 2004;114(10):1734-41.
2. Chan RK, Siller-Jackson A, Verrett AJ, et al. Ten years of war: a characterization of craniomaxillofacial injuries incurred during operations Enduring Freedom and Iraqi Freedom. J Trauma Acute Care Surg 2012;73(6 Suppl 5):S453-8.
3. Little SC, Kesser BW. Radiographic classification of temporal bone fractures: clinical predictability using a new system. Arch Otolaryngol Head Neck Surg 2006;132(12):1300-4.
4. Brodie HA, Thompson TC. Management of complicaions from 820 temporal bone fractures. Am J Otol 1997;18(2):188-97.
5. Shindo ML, Fetterman BL, Shih L, et al. Gunshot wounds of the temporal bone: a rational approach to evaluation and management. Otolaryngol Head Neck Surg 1995;112(4):533-9.
6. Ratilal BO, Costa J, Sampaio C, Pappamikail L. Antibiotic prophylaxis for preventing meningitis in patients with basilar skull fractures. Cochrane Database Syst Rev 2011;10(8):CD004884.
7. Moore PL, Selby G, Irving RM. Gunshot injuries to the temporal bone. J Laryngol Otol 2003;117(1):71-4.
8. Duncan NO, Coker NJ, Jenkins HA, Canalis RF. Gunshot injuries of the temporal bone. Otolaryngol Head Neck Surg 1986;94(1):47-5.
9. Rajati M, Pezeshki Rad M, Irani S, et al. Accuracy of high-resolution computed tomography in locating facial nerve injury sites in temporal bone trauma. Eur Arch Otorhinolaryngol 2013 Oct 1 (Epub ahead of print).
Declaration of Competing Interests: None declared.





