At a time of unprecedented technological advances, Taran Tatla and Jonathan Fishman gaze into the laryngological crystal ball…
Introduction
The recent explosion in science, technology and innovation takes us into a new era, with the opportunity and capability to transform the field of laryngology. A wealth of new imaging and treatment strategies, underpinned by huge jumps in information technology, data management, artificial intelligence, stem cells and augmented robotics applications are poised to improve our understanding of the pathophysiology and management of both benign and malignant laryngeal diseases.
Earlier, more accurate, diagnostic and targeted treatment strategies offer the potential to maximise functional and survival outcomes, leading to improved patient care. In tandem, the development of sustainable service delivery models will allow reductions in currently spiralling global health care expenditure.
“Earlier, more accurate, diagnostic and targeted treatment strategies offer the potential to maximise functional and survival outcomes, leading to improved patient care.”
In this review, we provide our opinion on the ‘top 10’ most significant developments that are likely to impact upon the field of laryngology over the next decade. Human genome project, tissue engineering, to name just a few examples!
Optical biopsy for mucosal disease screening, surveillance, stratification, prognostication and management
Various properties of light may be exploited to allow more detailed examination and interrogation of tissue, beyond that seen with white light illumination. High resolution, commercial camera systems already incorporate relatively simple light filtering techniques to allow narrow band-imaging in the green and blue wavelengths; this provides greater contrast of mucosal and submucosal vascular supply to tissue. Manufacturers and proponents champion the added benefit this provides to the ‘expert eye’ in making diagnostic decisions as to what requires more traditional invasive tissue biopsy and what does not. Narrow band imaging (NBI) is reported to add sensitivity and accuracy to clinician interpretation with regular use. However, its lack of specificity requires tissue still to be excised for formal histopathological interpretation.
Other optical modalities based on different optical principles have been developed and have been increasingly validated in animal and human models. Optical coherence tomography (OCT), utilising infra-red light to non-invasively contrast tissue morphology at micron-level up to 2-3mm into a tissue, has transformed ophthalmic retinal diagnostics over the last 20 years. Its potential is now being realised for commercialisation in endoscopy and topical/hollow-organ systems, particularly as a hybrid optical biopsy tool coupled with other optical imaging modalities, such as fluorescence lifetime imaging (FLIM)/spectroscopy (this provides spectral contrast that relates to molecular and other functional differences in the tissue).
The impact of optical biopsy will undoubtedly have major implications for disease screening and surveillance of dysplasia and cancer of the laryngo-pharynx, as well as for stratifying treatment based on endogenous tumour markers (e.g. HPV infection contrasted in vivo in real-time within a suspect lesion, without tissue removal and external tissue processing required). It follows that prognosis too may also be determined based on biomolecular ‘optical tissue-typing’ and ready/prompt decision-making for the chosen treatment modality. ‘Seeing genes’ in this manner in vivo has major implications for cost-savings and avoidance of patient morbidity and delays in traditional care pathways. The outcomes from the ‘100,000 Genomes Project’ will have a huge impact upon the management of head and neck cancers and other mucosal diseases of the upper aerodigestive tract (Figure 1) [1].
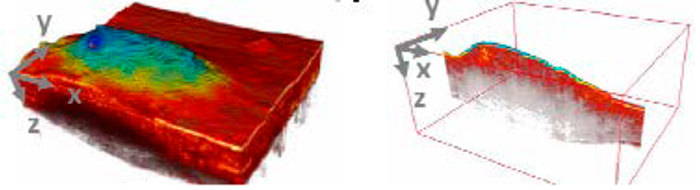
Figure 1. 3D multi-modal OCT images and FLIM maps of in vivo cancerous hamster cheek pouch, clearly contrasting and demarcating SCC from surrounding normal mucosa through high resolution mucosal tissue architectural and spectral detail.Reproduced with permission from Park et al. [1].
High speed digital imaging and sensing for objective assessment of laryngo-pharynx function
Endoscopic camera systems continue to evolve, allowing high-resolution digital data capture, archive and predictive diagnostics based on defined quantitative measurements. Video strobokymograms provide quantitative measures of motion and geometry of vocal folds, superseding more qualitative methods and videostroboscopy.
More advanced and hybrid camera systems capable of more detailed examination still are on the horizon, allowing objective quantitative measurements of voice quality, vocal cord, airway and pharyngeal swallow function, as well as adjunctive diagnostic information on tissue structure and nature. The inter-observer variability and subjectivity seen through human observation and interpretation, shall be replaced by hard objective measures defined and calculated autonomous to the operator, allowing diagnostic algorithms and software to be developed for automation in diagnostics. These developments bypass the limitations of the human eye and time-acquired experience, facilitating artificial intelligence to assist the diagnostician. The roles of operator and diagnostician may therefore be separated, allowing ‘non-experts’ to be trained in endoscopy tasks, meaning work-force development opportunities for lesser experienced allied health professionals and clinical scientists (Figure 2) [2].

Figure 2. In vivo cross-sectional long-range Doppler OCT imaging of vibrating vocal folds with a high-speed 1310nm swept-source OCT system (interval between each image is 5ms). Reproduced under the Creative Commons CC BY license from Coughlan et al. [2].
Transoral robotic/endoscopic surgery of laryngo-pharynx
Transoral robotic surgery (TORS), despite its high initial and maintenance costs, has been widely adopted over the past decade permitting oncologic margins similar to open surgery and minimising morbidity and deformity.
TORS has relied on rigid instruments and technology primarily designed for abdominopelvic and thoracic surgery. The scale and design of the first-generation platform is not ideally suited to the oral cavity, pharynx and larynx. Intuitive Surgical, Inc. have recently introduced the Da Vinci Sp, a new flexible and fully robotic surgical system deployed through a single arm and cannula, with a flexible camera and three instrument arms. This smaller system routinely allows four arms to be used simultaneously during transoral surgery of the oropharynx. Medrobotics have manufactured a comparable product (Flex® robotic system). Both of these systems allow three-handed surgery within the oropharynx, improving traction – countertraction and thus revealing a more accurate understanding of the complex three-dimensional relationships of the lateral oropharyngeal wall.
Further research and developments are underway combining real-time optical tissue imaging to enhance the functionality of the Da Vinci surgical system for precision surgery. Work is underway on the development of an integral optical diagnostic port to allow multi-spectral time-resolved fluorescence spectroscopy, for real-time (~secs) feedback on functional tissue features during robotic surgical procedures without the administration of exogenous fluorescence contrast. The robotic endo-laryngeal flexible scope (robo-ELF) furthermore offers an intuitive clinically usable robotic system for manipulating flexible endoscopes, particularly in minimally-invasive laryngeal surgery, thereby allowing the surgeon to control a flexible endoscope with only one hand and also to release the controls and perform bimanual surgery if desired.
A number of other collaborative academic-industrial partnerships have closely guarded plans for third generation more versatile, affordable and smart surgical robotics systems (including augmented vision and haptic feedback for the surgeon) which shall appear on the market requiring clinical validation over the next decade (Figure 3) [3].
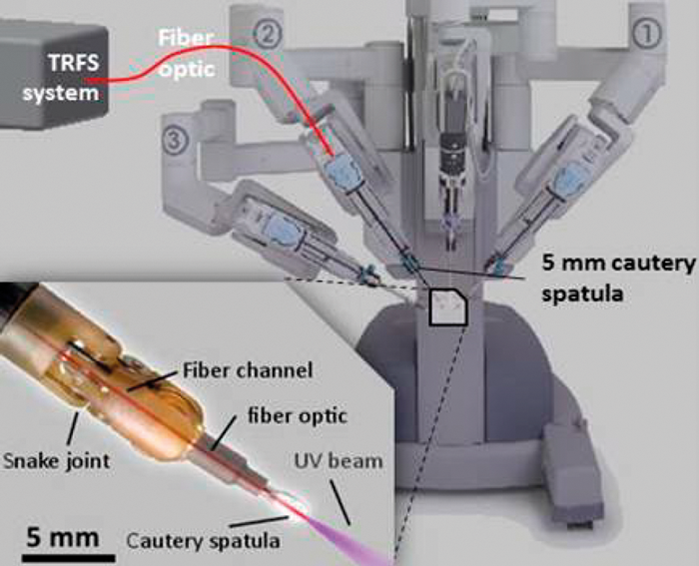
Figure 3. Image-guided robotic interventions. Design for da Vinci surgical robot in conjunction with ms-TRFS (multi-spectral time-resolved fluorescence spectroscopy). Inset: an optical port is integrated in one of the instrument arms to allow real-time, label-free measures of biochemical and functional tissue contrast intraoperatively during TORS. Reproduced with permission of Dr Laura Marcu, University of California Davis, CA, USA [3].
Tissue engineering, regenerative medicine and stem cells
The ability to regenerate tissues through the use of stem cells, biomaterials, growth factors or combinations of these (so-called tissue-engineering) is beginning to permeate into the field of laryngology. Diseases such as vocal fold scarring and sulci vocalis, where existing treatments are suboptimal, will ultimately benefit most from such developments. Stem cells retain the unique ability to differentiate into any tissue of the human body and can be genetically-engineered to express certain molecules, such as neurotrophic factors, which can be instrumental in assisting nerve in-growth in the case of vocal fold paralysis, for example [4].
Transplantation and 3D-bioprinting
As immunosuppressive regimens continue to improve, resulting in less toxic side-effects, laryngo-tracheal allotransplantation becomes a viable option in situations where tissue replacement is required. This will become more commonplace in future healthcare settings. 3D bioprinting offers the possibility to manufacture off-the-shelf organs and tissues (such as vocal folds and airways) to replace diseased ones. In addition, advances in ‘soft’ robotics offers the potential to prototype artificial robotic total laryngeal replacements for the purpose of rehabilitating laryngectomy patients [5].
Electrostimulation and optogenetics (light-based gene therapy)
Laryngeal pacing is a means of providing electrostimulation to the larynx. Such techniques may become widespread in the setting of unilateral and bilateral vocal fold paralysis. Extrapolation of the concept of laryngeal pacing to the pharynx and oesophagus may assist patients with oropharyngeal and oesophageal dysphagia, for example following chemoradiotherapy to the head and neck, or those with ‘neurological’ dysphagia.
In addition, researchers in Bonn are testing gene transfer techniques and optical stimulators for genetically-engineered muscles and targeted light stimulation in treatment of laryngeal and pharyngeal paralysis. Ion channel molecules from green algae called channel rhodopsins open when illuminated. When appropriately packaged and injected into a muscle, they are integrated into individual muscle cells. With light exposure, the channels open and positively charged ions flow into the muscle cell, which then contracts. Laryngeal and pharyngeal skeletal muscles can contract specifically, precisely and separately depending on where the light beam is pointed, surpassing limitations of electrode simulation and laryngeal pacing, allowing new approaches to treatment [6].
Point-of-care tools for community disease screening
The arrival of smartphone communications technology during this millennium has opened up a host of opportunities for community disease screening and monitoring, facilitating more targeted and integrated treatment strategies involving specialist and community service providers. A number of research groups have developed smartphone and software apps to evaluate common airway and sleep disorders, such as obstructive sleep apnoea (OSA) and snoring. Integral smartphone components such as cameras, microphones, accelerometers etc., as well as the software, computing power and telecoms capabilities (wi-fi link to world wide web, blue-tooth link to wireless pulse-oximeter finger sensors) have allowed the development and validation of point-of-care tools as an alternative to the gold-standard of in-laboratory polysomnography. These tools shall play an important role in preventative healthcare and cost-effective disease screening/monitoring, as well as altering attitudes and paradigm shifts towards telemedicine (Figure 4) [7, 8].

Figure 4. SleepAp screenshots. [L-R]: main menu; STOP-BANG questionnaire; recording; analysis. Reproduced under the Creative Commons Attribution Licence 2.5 (CCAL) from Behar et al. [8].
Better insight and understanding of pathophysiology in disease
The traditional model of biopsy (tissue removal) for making bench-top transmitting light microscopic observations (characterising disease and its cellular/molecular elements) is considered by many to be abstract, allowing inferences only on what occurred during life in vivo. It would be more appropriate to observe disease and its pathogenesis in vivo (without biopsy), to visualise relevant cell-cell and cell-matrix/molecular interactions in real-time and real circumstances. Multi-modal optical tools (including OCT, FLIM and Raman spectroscopy) are emerging to allow in vivo characterisation of disease and dynamic real-time optical observation of treatment impacts (e.g. novel ‘magic-bullet’ drugs, or other strategies such as light/photodynamic therapy). The important role of biofilms in the chronicity of ENT disease is slowly being established, and the extent of their involvement in colonisation of airway tubes, causing chronic inflammation and refractory tracheobronchial infections, is gradually being explored and realised [9]. Finally, advances in genomics (study of genes) and proteomics (study of proteins) will allow further insight into the causes and thereby treatment and prevention of particular conditions.
Sensors, smart materials and nanotechnology
Airway tube construction and design are likely to evolve further through emerging research using real-time in vivo optical imaging of biofilms and tracheostomy tubes lying in situ and through the new dawn of nanotechnology-enhanced biomaterials. Advancements in nanomedicine and ‘smart tube’ technology should take advantage of newer, affordable and practical methods for incorporation of tube sensors (cuff pressure, air flow, CO2 level monitoring, etc.) within airway endotracheal and tracheostomy tubes, thereby facilitating objective decision-making and safety during aftercare.
Nanotechnology is a multidisciplinary science that seeks to create and utilise novel materials, devices and systems at the nanometer scale. It has a far reaching potential for both nonmedical and biomedical applications: in the latter for targeted drug delivery, molecular imaging, biomarkers and biosensors.
“In the next decade we can expect to see significant advances in immunotherapy regimens to treat a wide range of conditions such as laryngeal carcinoma and laryngeal papillomatosis.”
Nanotechnology-enhanced biomaterials designed to withstand bacterial/fungal biofilm colonisation and predisposition to early tube failure or other complications (e.g. tracheitis, granulation and scar tissue formation with tracheostomies) are already beginning to emerge and promise a new enlightened era of tracheostomy and airway tube care [10].
The unique optico-electronic-chemical properties of gold and other nano-particles promise a multitude of high technology healthcare applications including sensory probes for disease diagnosis and screening, as well as targeted therapies for conditions including cancer (Figure 5).
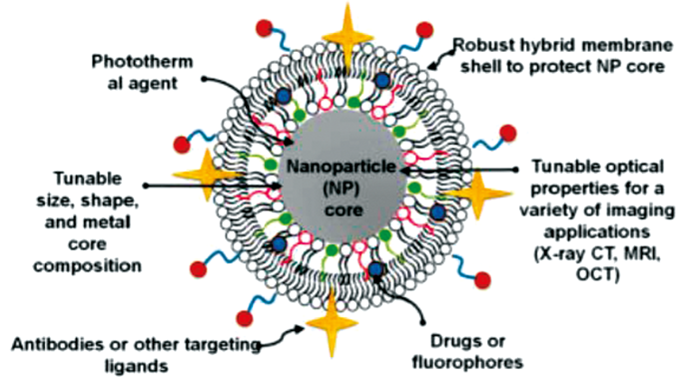
Figure 5. Schematic diagram of hybrid bilayer-membrane-coated gold nanoparticle. Reproduced with permission of Thomas Miesen, Marilyn Mackiewicz lab, Portland State University, OR, USA.
Advances in immunotherapy and vaccination programmes
In the next decade we can expect to see significant advances in immunotherapy regimens to treat a wide range of conditions such as laryngeal carcinoma and laryngeal papillomatosis. Drugs, such as bevacizumab (Avastin®) are already beginning to show promise in the treatment of papillomatosis. As our understanding of disease pathophysiology improves, newer monoclonal antibodies will become available which target particular ligands and receptors responsible for causing disease. In addition, as vaccination programmes continue to advance and become universally available (e.g. extending HPV vaccination in the UK to boys) diseases such as laryngeal papillomatosis and HPV-associated oropharyngeal carcinoma will become obsolete (Figure 6).
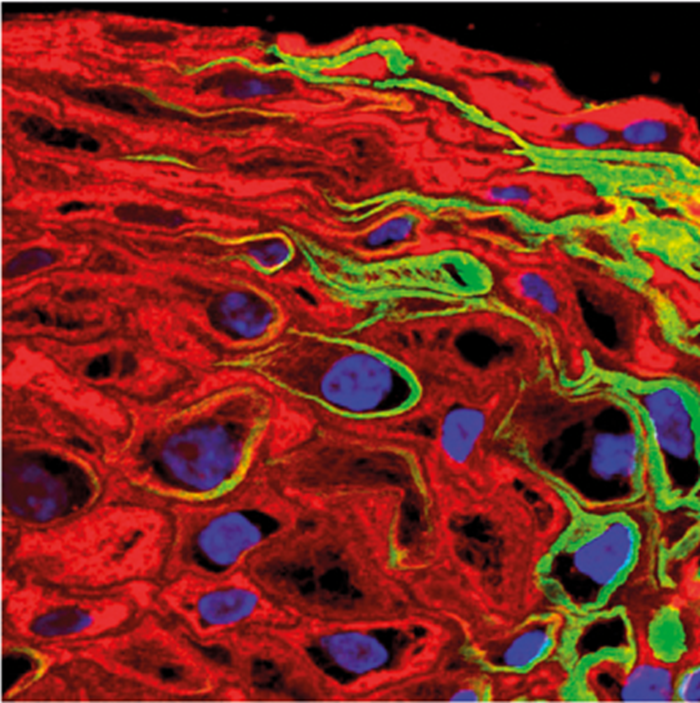
Figure 6. Wellcome collection: HPV in epithelium. Reproduced under the Creative Commons CC BY license from NIMR, Francis Crick Institute (https://wellcomecollection.org/works/zf8f9kee).
Conclusions
In the next 10 years we can anticipate seeing rapid developments in the field of laryngology ranging from improvements in diagnostics (optical imaging, high speed digital imaging, smartphone apps), surgical techniques (robotics), translation of the basic sciences (stem cells, tissue engineering, biomaterials, nanotechnology, immunology) and disease prevention (vaccinations). The future for laryngology looks bright!
References
1. Park J, Jo JA, Shrestha S, et al. A dual-modality optical coherence tomography and fluorescence lifetime imaging microscopy system for simultaneous morphological and biochemical tissue characterization. Biomed Opt Express 2010;1:186-200.
2. Coughlan CA, Chou L, Jing JC, et al. In vivo cross-sectional imaging of the phonating larynx using long-range Doppler optical coherence tomography. Sci Rep 2016;6:22792.
3. UC Davis Biomedical Engineering. Image-Guided Robotic Interventions. Available at
https://bme.ucdavis.edu/
marculab/image-guided-robotic-interventions/
Last accessed 14 January 2018.
4. Fishman JM, Long J, Gugatschka M, et al. Stem cell approaches for vocal fold regeneration. Laryngoscope 2016;126(8):1865-70.
5. Krishnan G, Du C, Fishman JM, et al. The current status of human laryngeal transplantation in 2017: A state of the field review. Laryngoscope 2017;127(8):1861-8.
6. Bruegmann T, van Bremen T, Vogt CC, et al. Optogenetic control of contractile function in skeletal muscle. Nature Communications 2015;6:7153.
7. Ong A, Gillespie MB. Overview of smartphone applications for sleep analysis. World Journal of Otorhinolaryngology-Head and Neck Surgery 2016;2(1):45-9.
8. Behar J, Roebuck A, Shahid M, et al. SleepAp: An automated obstructive sleep apnoea screening application for smartphones. Computing in Cardiology 2013;40:257-60S.
9. Meslemani D, Yaremchuk K, Rontal M. Presence of biofilm on adult tracheostomy tubes. Ear Nose Throat J 2010;89(10):496-504.
10. May RM, Hoffman MG, Sogo MJ, et al. Micro-patterned surfaces reduce bacterial colonization and biofilm formation in vitro: Potential for enhancing endotracheal tube designs. Clin Transl Med 2014;3:8.





