During the COVID pandemic, all our working patterns have changed. One significant impact had been on the management of outpatient consultations and the increase in telephone consultations and enhanced vetting. In this article the authors share their experience of managing dizziness referrals during the pandemic.
Face-to-face (f2f) consultation was initially discontinued during the COVID-19 pandemic lockdown. Unlike much of ENT where examination with a microscope or endoscope is required, the diagnosis of a balance disorder relies more on the history. We report an innovative approach to the management of patients with vestibular disorders using validated questionnaires and telephone consultation.
Methods
All GP-referred patients with a balance problem were contacted to answer a validated questionnaire [1] which showed good predictive accuracies for the common causes of dizziness and is safe for triaging at our centre [2]. Based on the GP letter and questionnaire, the senior author assigned patients for either telephone or f2f appointments. Telephone consultations (TF) were then carried out, leading to a f2f review appointment, reassessment after investigation, or discharge. The clinician recorded the time taken and the diagnosis after each of the following stages: 1. review of the electronic GP letter (e-triage); 2. review of the validated questionnaire; 3. TF ; and/or 4. at follow-up which could be f2f or TF. Two telephone attempts were made after three months to check satisfaction and symptom resolution. Hospital records were also reviewed to check for re-referral with worsening symptoms, presentation to the emergency department or admission to hospital with dizzy symptoms.
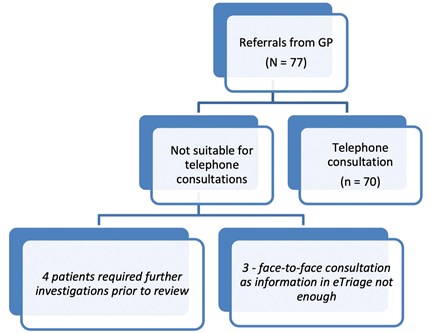
Figure 1: Flowchart of referrals received.
Results
From 1 June 2020 to 11 September 2020, 70 out of 77 patients were considered suitable for TF (see flowchart). The median age was 57 years, with male to female ratio of 3:8. No patients had been re-referred with worsening symptoms, presented to emergency department or been admitted to hospital for dizziness-related symptoms. Of these consultations, 87% were conducted by a consultant otologist. Reading of patient information and GP referrals took less than 10 minutes; 82% of telephone consultations, including dictation and administrative tasks took between 15 and 30 minutes.
Following TF, 29 (38%) were discharged, and 15 (19%) required f2f consultation (Figure 1). Of those that were discharged and responded to the telephone survey, none were dissatisfied with the service but two with benign paroxysmal positional vertigo (BPPV) reported worse symptoms.
The majority of diagnoses at e-triage is unknown (41%), reducing to 30% after questionnaire and 11% after TF (Figure 2). The second commonest diagnosis following e-triage was BPPV (29%) but this became the most common after questionnaire (33%) and TF (42%). The proportion of patients diagnosed with probable Meniere’s disease was halved after TF (16% at e-triage to 8%).
In total, 38/70 patients responded to telephone survey (Figure 3). Overall, patients were very grateful to receive a call: 30 (79%) were satisfied by TF; five out of six diagnosed with BPPV after TF reported worse symptoms. Patients were occasionally unavailable at the appointment time but contactable by the end of the clinic session. A ‘blurring of boundaries’ was noted with some patients calling back repeatedly, expecting to speak directly to the clinician. Some of the reasons for dissatisfaction were “appointments were messed up”, “exercises did not help”, or patients still experienced the same problems.
Of the 70 patients, 34 (49%) had a consistent diagnosis from e-triage to TF. Figure 4 shows that questionnaire and TF diagnoses are most concordant with each other (57%).
Following TF, 45% of patients were considered to require audiological testing, whereas 20% required imaging (Figure 5). Only six out of 77 (8%) of patients were considered to require imaging from the outset of e-triage, where the diagnosis in three of them was ‘unknown’, two ‘Meniere’s’ and one ‘BPPV’.
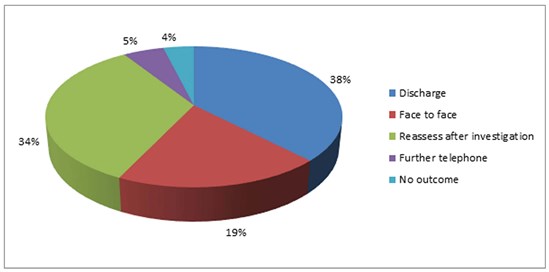
Figure 2. Shows the outcome of patients following telephone consultation.
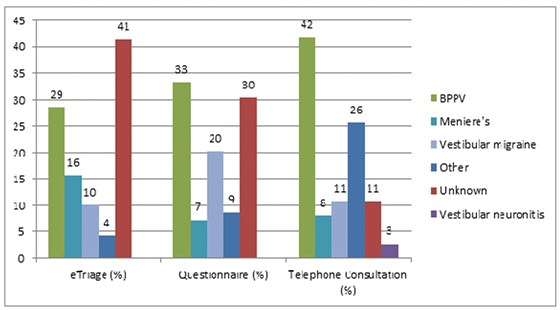
Figure 3. Percentage of diagnoses (labelled) at each checkpoint).
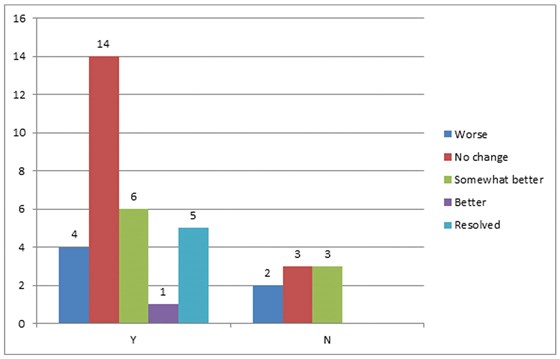
Figure 4. Outcome of telephone survey (label denotes number of patients). Y = satisfied, N = not satisfied.
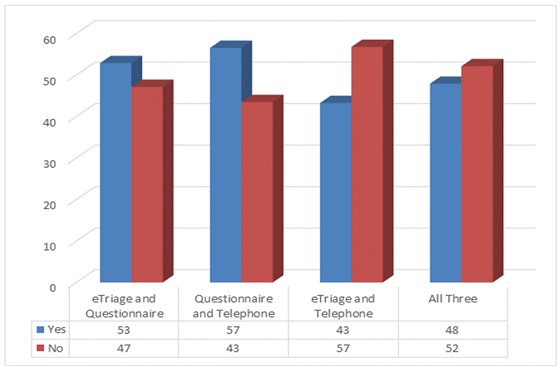
Figure 5. Bar chart as a visual representation of the concordance in diagnoses between two checkpoints.
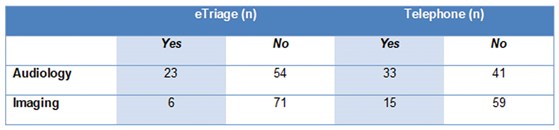
Figure 6. Investigations deemed required at e-triage and telephone consultation.
Investigations deemed required at e-triage and telephone consultation.
Case study
A patient was referred with short episodes of positional vertigo, unilateral pulsatile tinnitus and normal ear examination. Provisional diagnosis of BPPV was made following TF but an MRI was done as pulsatile tinnitus is not characteristic of BPPV.
Bilateral tympanic retractions were found at f2f. Audiogram showed right-sided mild conductive loss at high frequencies and imaging showed right-sided cholesteatoma eroding lateral semicircular canal. The patient underwent combined approach tympanoplasty and vestibular rehabilitation with subsequent improvement of vertigo.
Discussion
The fact that none of the patients were re-referred with worsening symptoms, presented to emergency department, or were admitted to hospital for dizzy symptoms, suggests that this is a safe short-term approach. Our approach demonstrated a correlation with a previous study where there were f2f consultations conducted on the same geographical area of GP referrals [2]. The ratio of diagnoses was similar, with 42% of our patients diagnosed with BPPV vs. 44% in the previous study (Fisher’s exact test, p = 0.85); we found 11% of vestibular migraine versus 10% (p = 1.00).
As concordance between questionnaire and TF was found to be highest, we have changed the referral pathway to mandate elements of the questionnaire in every GP referral letter before offering an appointment. It also means preliminary diagnosis can be made to start treatment while the patient is awaiting an appointment.
Patients who were either dissatisfied (8/38) or worse (6/38) contained a high proportion of BPPV diagnosis. This is not surprising as the gold standard treatment is particle repositioning manoeuvre rather than habituation exercises. Some way of performing Epley manoeuvres in the midst of a pandemic should be sought.
The majority of the TF took between 15 and 30 minutes but in f2f appointments, clinicians would be able to perform physical examination within 30 minutes. This means that f2f is favoured whenever possible.
The case study illustrates the inherent risk in situations where f2f consultation is not possible. However, the symptom of pulsatile tinnitus picked up on e-triage, questionnaire and telephone consultation did not fit with BPPV, which prompted further assessment.
Conclusion
Our experience demonstrated that this system appears diagnostically accurate and safe in the short term when f2f consultations are not possible. With this method, BPPV has the lowest rate of satisfaction and successful treatment. In the future we will be using questionnaires in all our balance patients to aid triage, diagnosis and to begin treatment before appointment. F2f is still favoured whenever possible, as examination can be performed within the same time frame.
References
1. Roland L, Kallogjeri D, Sinks B, et al. Utility of an Abbreviated Dizziness Questionnaire to Differentiate between Causes of Vertigo and Guide Appropriate Referral: A Multicenter Prospective Blinded Study. Otol Neurotol 2015;36(10):1687-94.
2. Bennett A, Yeo JCL, Rao A. The effectiveness of a questionnaire in the triage and diagnosis of balance disorders. The Otorhinolaryngologist 2015;8(3):130-3.







