In this article, the authors describe a simple and effective technique for extracting an aspirated voice prosthesis from within the tracheobronchial tree in the awake laryngectomised patient using the Ambu® aScopeTM 4 Broncho endoscope.
Surgical voice restoration remains the dominant mode of speech rehabilitation in patients who have undergone total laryngectomy. This is facilitated by the formation of a tracheo-oesophageal puncture and the placement of an indwelling voice prosthesis [1].
Dislodgement of the prosthesis can lead to aspiration into the airway which may result in significant morbidity [2]. We describe our favoured approach to the safe retrieval of an aspirated voice prosthesis using a flexible video bronchoscope under local anaesthesia.
Technical description
The procedure requires a minimum of one main operator and one assistant. It is recommended that this is performed in a monitored clinical environment. Figure 1 illustrates the equipment needed to perform the procedure.
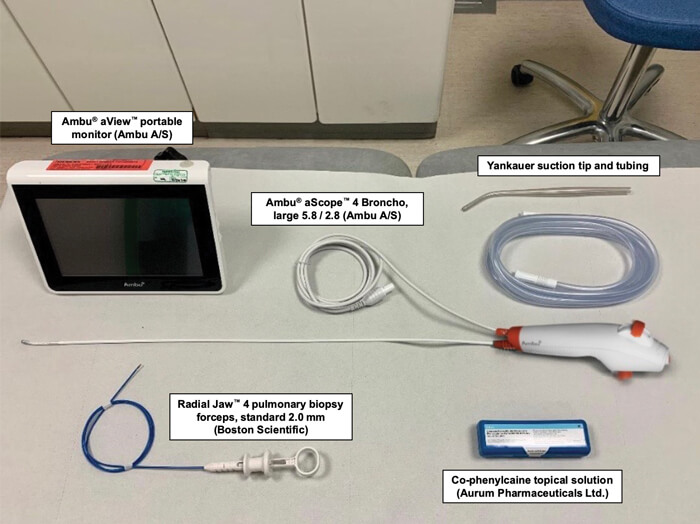
Figure 1. Equipment required for the procedure.
The Ambu® aScopeTM 4 Broncho flexible endoscope is connected to the Ambu® aViewTM portable monitor (Ambu A/S, Ballerup, Denmark). The patient is positioned on an examination couch in a semi-recumbent position. The laryngectomy stoma is inspected, and excess secretions are suctioned using a Yankauer sucker. Co-phenylcaine local anaesthetic spray (lidocaine hydrochloride 5% w/v and phenylephrine hydrochloride 0.5% w/v topical solution) (Aurum Pharmaceuticals Limited, Romford, UK) is administered to the laryngectomy stoma and proximal trachea. After a few minutes, the bronchoscope is introduced via the laryngectomy stoma and the airway is examined. The location of the aspirated voice prosthesis is confirmed within the tracheobronchial tree (Figure 2).

Figure 2. Endoscopic view of an aspirated Blom-Singer® ClassicTM indwelling voice prosthesis
(InHealth Technologies, Carpinteria, CA, USA) within the right main bronchus.
The Radial JawTM 4 pulmonary biopsy forceps (Boston Scientific, Marlborough, MA, USA) are inserted via the working channel of the bronchoscope and advanced until the jaws come into view on the monitor just beyond the tip of the bronchoscope. The forceps are controlled by the assistant henceforth while the main operator focuses on navigating the bronchoscope. The bronchoscope and forceps are advanced further until the location of the voice prosthesis is reached. The jaws of the forceps are opened by the assistant. The voice prosthesis is carefully grasped. Atraumatic retrieval of the prosthesis is ensured by withdrawing the forceps and bronchoscope under direct vision.
“The current technique can be performed safely under local anaesthesia thereby avoiding the burden and associated risks of a general anaesthetic”
Discussion
Total laryngectomy plays an important role in the treatment of locally advanced laryngeal cancer. It may constitute the primary treatment modality (primary total laryngectomy) or may be performed for recurrent disease following unsuccessful radiotherapy with or without chemotherapy (salvage total laryngectomy).
The impact of undergoing total laryngectomy on the quality of life of patients is significant. Laryngectomees face lifelong physical and psychosocial consequences as a result of substantial alterations to essential bodily functions, including respiration, swallowing and speech. Voice restoration, therefore, forms a cornerstone in the postoperative rehabilitation of these patients. Conventionally, this is achieved by one of three methods: oesophageal speech, tracheo-oesophageal speech or via the use of an electrolarynx.
Over the years, tracheo-oesophageal speech has emerged as the gold standard for achieving post-laryngectomy voice restoration. This method offers a relatively faster rate of speech acquisition, better intelligibility and an increased duration of phonation [3]. It is also associated with higher patient satisfaction compared to other forms of alaryngeal speech [4].
By occluding the laryngectomy stoma on expiration, air from the lungs is channelled through an indwelling one-way silicone speaking valve which sits in a surgically-created fistula between the trachea and the oesophagus. This air, in turn, causes mucosal vibrations in the pharyngo-oesophageal segment, thereby generating a voice.
“Single-use flexible videoscopes, such as the Ambu® aScopeTM 4 series, have the advantage of eliminating the potential risk of infection due to cross-contamination from inadequately reprocessed reusable equipment”
Pulmonary aspiration of the indwelling voice prosthesis is a relatively uncommon, albeit recognised, complication. This typically occurs when a loose-fitting prosthesis, due to an enlarged tracheo-oesophageal fistula, becomes dislodged [5]. Similarly, a cough stimulated during a prosthesis change can also result in aspiration of the device into the airway. Patients may subsequently present with moderate to severe dyspnoea although others may develop no overt symptoms at all. Timely management in this setting is crucial to prevent more serious sequelae.
The traditional use of rigid bronchoscopes in the extraction of tracheobronchial foreign bodies poses a technical challenge in the laryngectomised patient. Interference from the mandible may hinder the passage of the bronchoscope through the laryngectomy stoma despite hyperextension of the neck, thereby limiting the view. This can be particularly difficult in patients with a short neck and in those with fixed cervical flexion deformity. Flexible bronchoscopy provides relatively better access to and clearer visibility of the distal bronchial segments. This is particularly useful in the context of the aforementioned anatomical limitations in laryngectomees.
In our experience, the current technique can be performed safely under local anaesthesia thereby avoiding the burden and associated risks of a general anaesthetic. The brief nature of the procedure has the added benefit of immediate symptomatic relief and a shorter overall hospital stay for the patient. Furthermore, single-use flexible videoscopes, such as the Ambu® aScopeTM 4 series, have the advantage of eliminating the potential risk of infection due to cross-contamination from inadequately reprocessed reusable equipment. We therefore feel that the Ambu® aScopeTM 4 Broncho endoscope is a valuable addition to the armamentarium of the otolaryngologist in the acute care setting.
References
1. Owen S, Paleri V. Laryngectomy rehabilitation in the United Kingdom. Curr Opin Otolaryngol Head Neck Surg 2013;21(3):186-91.
2. Ostrovsky D, Netzer A, Goldenberg D, et al. Delayed diagnosis of tracheoesophageal prosthesis aspiration. Ann Otol Rhinol Laryngol 2004;113(10):828-9.
3. van Sluis KE, van der Molen L, van Son R, et al. Objective and subjective voice outcomes after total laryngectomy: a systematic review. Eur Arch Otorhinolaryngol 2018;275(1):11-26.
4. Galli A, Giordano L, Biafora M, et al. Voice prosthesis rehabilitation after total laryngectomy: are satisfaction and quality of life maintained over time? Acta Otorhinolaryngol Ital 2019;39(3):162-8.
5. Malik T, Bruce I, Cherry J. Surgical complications of tracheo-oesophageal puncture and speech valves. Current Opin Otolaryngol Head Neck Surg 2007;15(2):117-22.Figure 2. Endoscopic view of an aspirated Blom-Singer® ClassicTM indwelling voice prosthesis (InHealth Technologies, Carpinteria, CA, USA) within the right main bronchus.







