As unusual as it may sound, some people have great difficulty burping. We hear of one approach to tackling this problem.
Retrograde cricopharyngeal dysfunction (RCPD) is a condition presenting with inability to burp, resulting in gaseous distension of the digestive tract. These symptoms are commonly bloating, retrosternal pressure discomfort and excessive flatulence.
The symptoms are often aggravated by fizzy/carbonated drinks but can also be aggravated by normal meals and drinks. The patients don’t normally experience anterograde symptoms such dysphagia, hence the term retrograde cricopharyngeal dysfunction which was first coined by Robert Bastian [1].
The majority of people that present with RCPD reported that they have never been able to burp since birth, and this has been confirmed by their parents. This suggests that some people are born with the condition. There are also people who reported family members, either siblings or parents, having the same problem of not being able to burp.
The treatment is with botulinum toxin A (Botox) injection into the cricopharyngeal muscle, either under a general anaesthetic by suspension pharyngoscopy or transcutaneously guided by electromyography awake. Remarkably, a single injection seems to restore burping in 80-90% of people, even after the Botox has worn off after three months.

Figure 1. Weerda diverticuloscope.
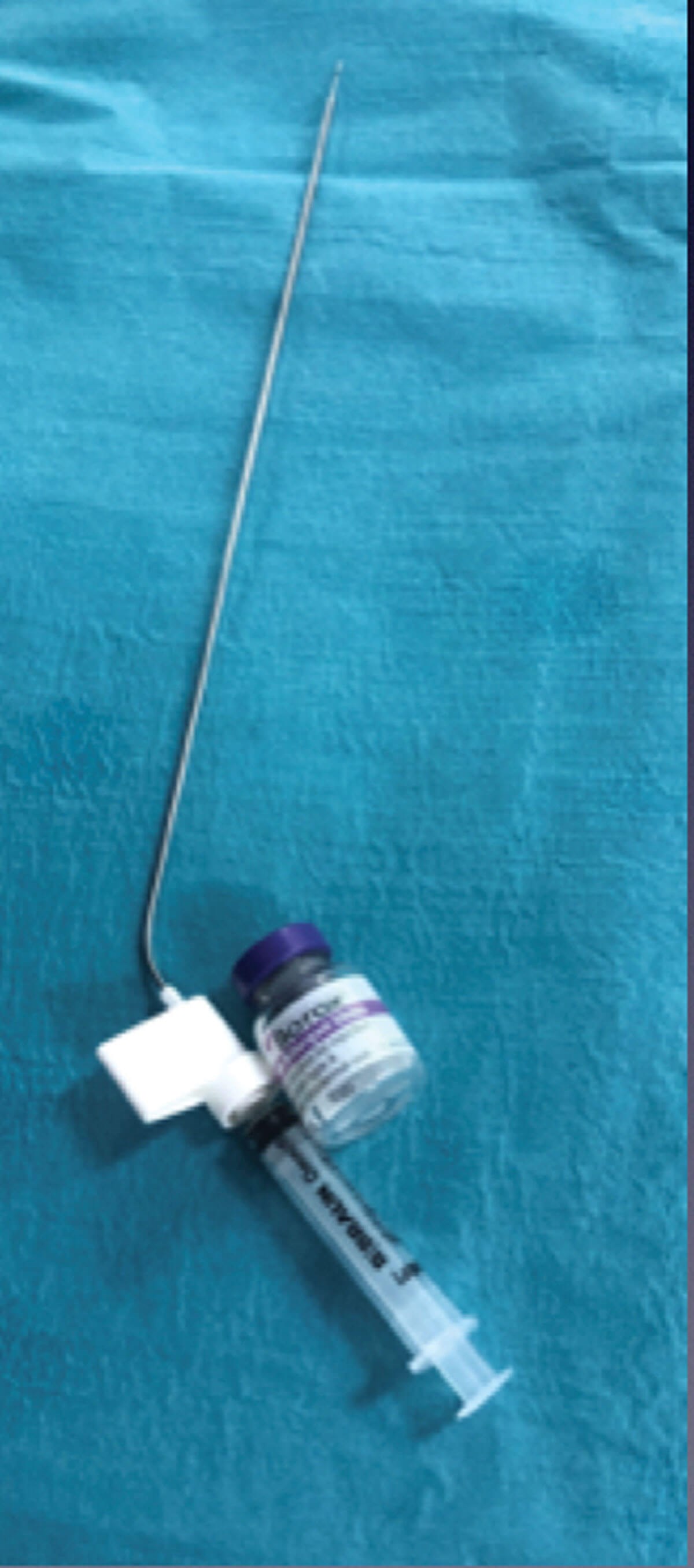
Figure 2. Botox diluted in normal saline
and attached to laryngeal needle.
Method
Equipment
- Weerda diverticuloscope (Figure 1)
- Botox 100 IU + 2ml normal saline + laryngeal injection needle (Figure 2)
Technique
Botox 100 IU is mixed with 2ml or 3ml of normal saline and drawn into a 2ml syringe.
The syringe filled with Botox diluent is attached to a long Renú laryngeal needle and primed. Suspension pharyngoscope using either a Weerda diverticuloscope or Benjamin oesophageal speculum, both made by Storz (Figure 3).

Figure 3. Suspension pharyngoscopy.
The diverticuloscope is introduced carefully into the cricopharyngeal inlet and the cricopharyngeal muscle CP is identified. A Hopkin rod laryngeal telescope is used to visualise the CP muscle during the injection.
Alternatively, a microscope may be used but the telescope gives a better sense of depth of the tip of the needle during injection.
"There is often submucosal venous plexus over the CP muscle and an attempt should be made to avoid injecting directly into this as it does bleed"
The author injects the Botox diluent in three points in the CP muscle: 50 IU in the posterior belly, 25 IU in the right posterior lateral belly, and 25 IU in the left posterior lateral (Figure 4).
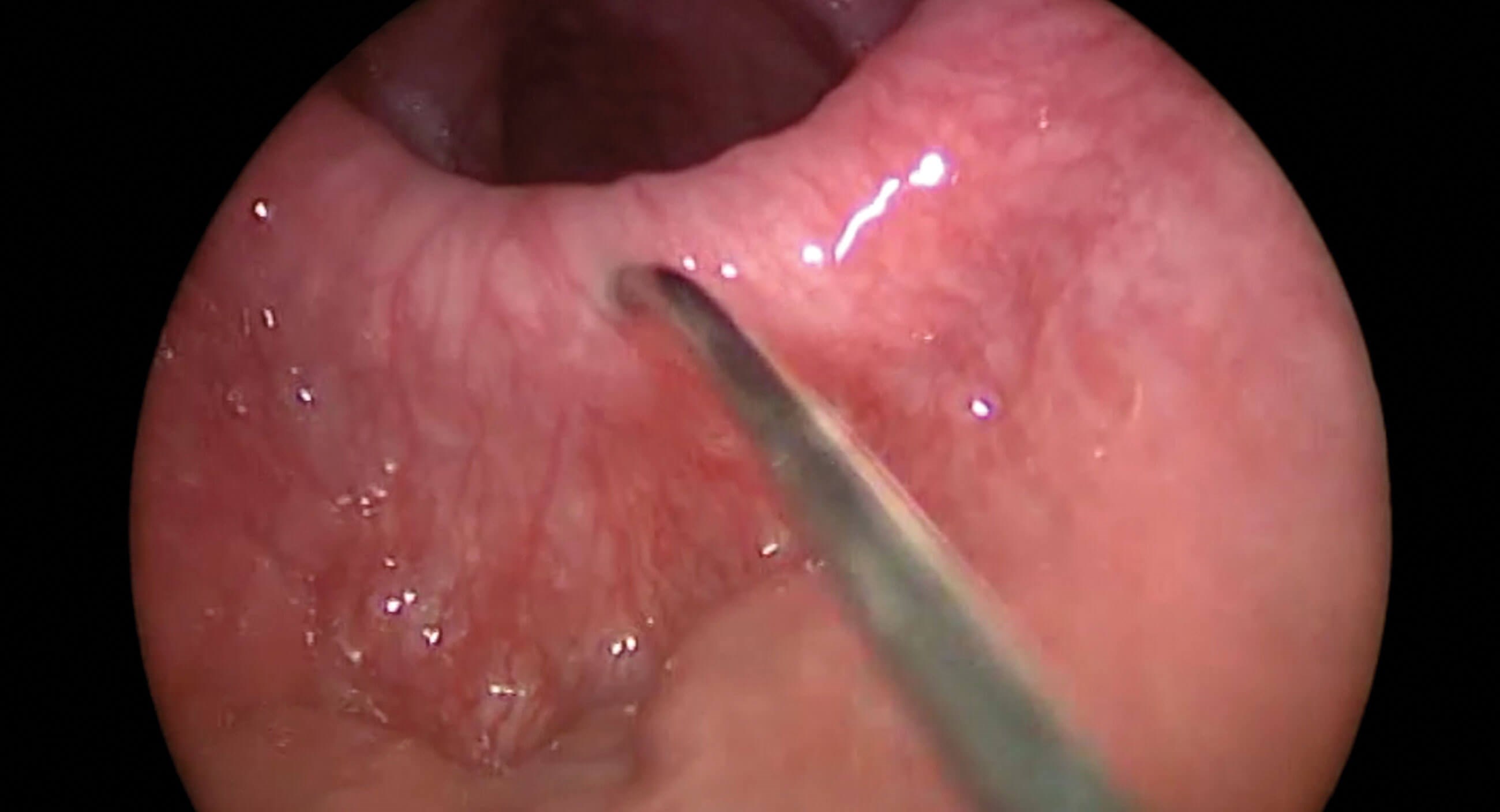
Figure 4. Botox injection into the cricpharyngeal muscle.
There may be some mucosal bleeding immediately on removal of the needle from the CP muscle after the injection. This is easily stopped with adrenaline 1:1000 soaked in a neurosurgical patty.
Complications
Immediate
Damage to teeth, torn or bruised lips, tongue, oropharynx and/or oesophagus, bleeding and anaesthetic complications.
Intermediate
Dysphagia, regurgitation, stridor, hoarseness and weak voice.
Long term
This is rare and the author has not experienced any long-term complications yet, after injection over 200 cases.
Tips and tricks
- Anatomical variations in patients meant that some patients are better with Benjamin oesophageal speculum and others Weerda diverticuloscope.
- The Renú long laryngeal needle has a dead space of 0.5ml so this needs to be borne in mind.
- There is often submucosal venous plexus over the CP muscle and an attempt should be made to avoid injecting directly into this as it does bleed.
Discussion
RCPD is fairly rare and not well known. It is frequently misdiagnosed, and patients can go on for several years having inappropriate treatment.
The diagnosis of this dysfunction is by history. Often, transnasal endoscopic examination of the pharynx, mainly to exclude any pharyngeal pathologies such as oesophageal inlet patch, polyps, cyst etc, may be useful.
Oesophageal impedance and manometry may or may not show high upper oesophageal sphincter pressure and does not exclude or confirm the diagnosis. Barium swallow may only show gaseous distension of the oesophagus or stomach (Figure 5). Imaging such as USS, CT scan and MRI scan are not necessary as it will often be reported normal but may show gaseous distension of the digestive tract.
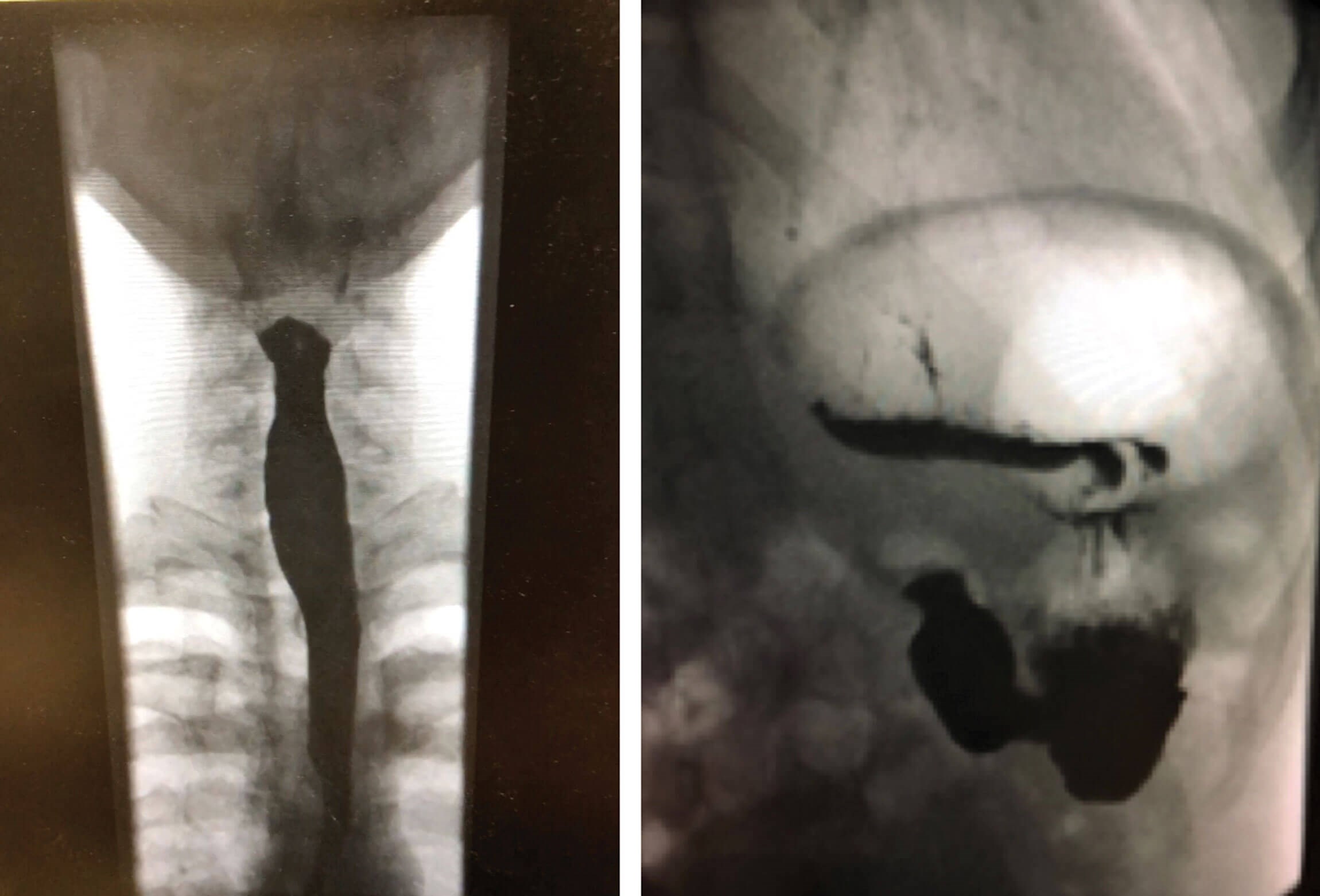
Figure 5. Barium swallow showing gaseous distension
of oesophagus (left) and stomach (right).
Oesophago-duodeno-gastroscopy (OGD) provides little information about the diagnosis of this condition but may exclude other oesophageal and gastric conditions.
Conclusion
Retrograde cricopharyngeal dysfunction is still poorly understood and patients can go on for years without diagnosis and treatment. The success rate for treatment with botulinum toxin A injection is very high, with a reported success rate of over 80% with a single injection [1,2]. About 20% will need a second injection within 12 months after the first wears off, and another 5% will need a third injection. No patient has returned for a fourth injection so far in the author’s practice.
References
1. Bastian RW, Smithson ML, Inability to Belch and Associated Symptoms Due to Retrograde Cricopharyngeus Dysfunction: Diagnosis and Treatment. OTO Open 2019;3(1):2473974X19834553.
2. Karagama Y. Inability to belch/burp- a new disorder? Retrograde cricopharyngeal dysfunction (RCPD). Eur Arch Otorhinolaryngol 2021;278(12):5087-91.





