Chronic ear disease can be challenging to manage and difficult for patients to live with. In this article, the authors describe their technique for otomastoid obliteration and blind sac closure of the external canal allowing for a more tolerable situation for the patient.
In selected cases of recalcitrant chronic ear disease, middle ear obliteration with blind sac closure of the external auditory canal can result in an improvement in patient quality of life [1]. There are several materials used to obliterate the mastoid cavity following subtotal petrosectomy, most commonly abdominal fat.
Although this is easy to harvest and insert, fat is avascular, and is quickly broken down and resorbed by the body so the authors prefer a vascularised temporoparietal flap (TPF). This makes use of the temporoparietal fascia which is supplied by a branch of the superficial temporal artery (STA) through its pedicle.
Method
A Doppler probe is used preoperatively to assess for the presence and position of the STA. The artery runs cephalad over the root of the zygoma in the preauricular region before bifurcating into its frontal and parietal branches; roughly 75% of the time this occurs above the zygomatic arch [2].

Figure 1: Picture showing preoperative markings. H – hairline, representing the anterior limit of the dissection; P – postauricular incision situated 1-2cm behind the ear; T – point at which the superficial temporal artery was located using a Doppler probe; Y – Y-shaped incision arising from the superficial temporal artery point, and curved to facilitate superior healing.
Following infiltration with a mixture of 2% lidocaine with 1:80,000 adrenaline, a typical postauricular incision is made, extended cranially into the temporoparietal region of the scalp and bifurcated into a ‘Y’ shape (Figure 1). A line demarcating the hairline is drawn on the skin and represents the anterior limit of dissection to safely avoid injury to the temporal branch of the facial nerve. This runs in the SMAS plane and is at risk during dissection, potentially resulting in ipsilateral brow ptosis and forehead paralysis [3].
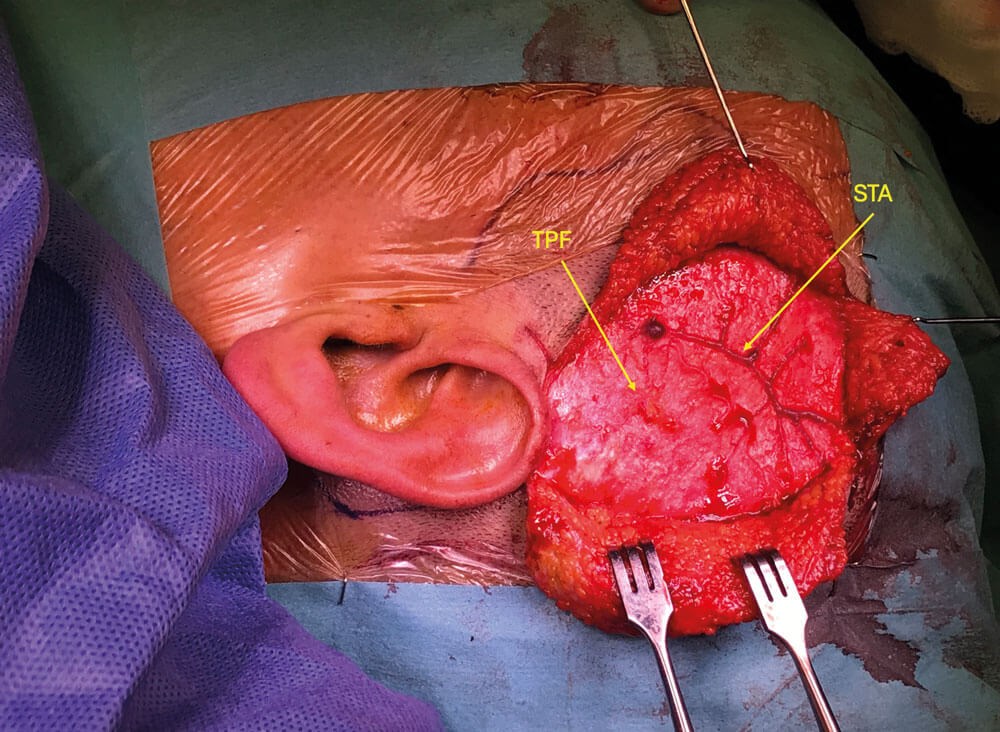
Figure 2: Picture showing scalp flaps raised. The temporoparietal fascia (TPF) has been
exposed and a branch of the superficial temporal artery (STA) is demonstrated.
Skin flaps are raised anteriorly and posteriorly to expose a large area of the temporoparietal fascia (Figure 2). This is performed in a sub-dermal plane immediately beneath the hair follicles, using sharp dissection to reduce the risk of alopecia through hair follicle injury. This is facilitated with traction and counter-traction between skin hooks on the skin edge and a swab gently tensing the fascia. Bipolar haemostasis should be used very sparingly to control bleeding; otherwise, patties soaked in 1:10,000 adrenaline are used for haemostasis. Where possible, care should be taken to stay superficial to any vessels encountered. Once an adequate amount of fascia has been exposed, it is dissected off the underlying temporalis muscle and kept pedicled on the STA (Figure 3). It is placed back down, saline-soaked gauze is used to keep it moist and the skin flaps are returned over the flap. The edges are loosely approximated with skin staples while attention is turned to the ear.
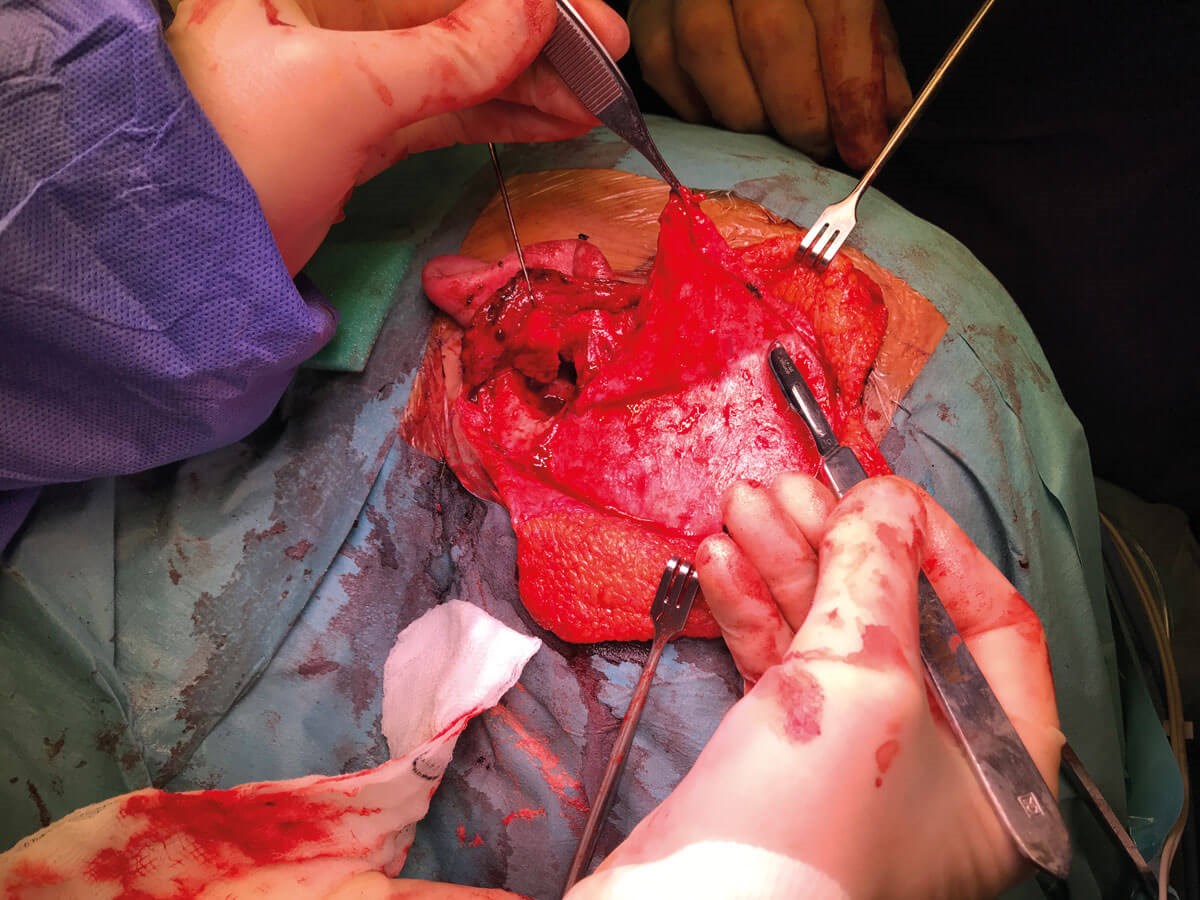
Figure 3: Picture showing the temporoparietal fascia being carefully dissected
off the underlying temporalis muscle and pedicled on the STA.
A Palva flap is raised, and posterior re-entry incision is made into the posterior canal wall skin as medially as possible to preserve maximal canal skin laterally. This will facilitate closing off the external auditory canal later. A subtotal petrosectomy, with removal of the tympanic membrane, malleus and incus (if present) is performed. The middle ear mucosa is stripped and as smooth a cavity as possible is created, which usually requires drilling the bony annulus flush with the surrounding bone. The mucosa should also be stripped from the opening to the bony portion of the eustachian tube, which opens at the anterior (or ‘carotid’) wall of the tympanic cavity around the level of the petrotympanic (Glaserian) fissure.
Where necessary, the orifice is widened with the drill to improve surgical access. Dissection in this area is performed cautiously with a fine diamond burr or curette and with the proximity of the internal carotid artery in mind. The bony canal through which the tensor tympani muscle runs is drilled away to reveal the muscle, which can then be elevated out and inverted to plug the eustachian tube orifice. Temporalis fascia or muscle can be used to supplement this if the bulk of the muscle is insufficient. Bone chips harvested from the mastoid bone are further introduced and the entire plug is then sealed with bone wax (Figure 4).
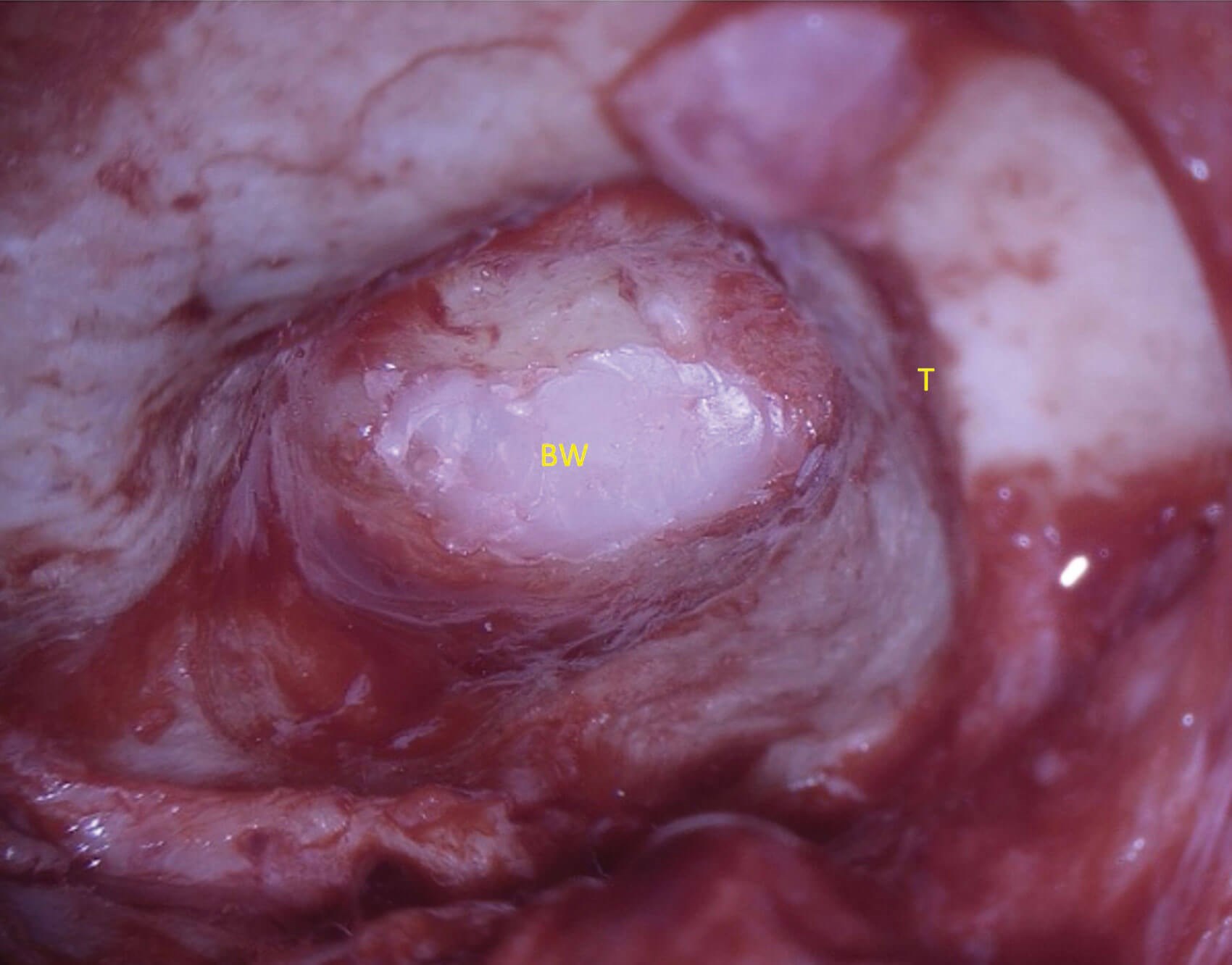
Figure 4: Picture showing a completed subtotal petrosectomy. T – the tegmen labelled for orientation; BW – bone wax used as the final material to obliterate the eustachian tube after the inverted tensor tympani muscle and bone chips.
The final step is closing off the external auditory canal, which involves everting the skin laterally before suturing it closed. The posterior re-entry incision is extended to form a complete circumferential incision. All skin medial to this incision is elevated and removed if still present. The skin must now be raised off the anterior canal wall and under-surface of the tragus (which may require sharp dissection). A circumferential rim of at least 1cm is ideal to provide enough laxity and length for sufficient closure, which is performed with interrupted everting 5-0 Vicryl Rapide sutures.
Once the external auditory canal skin has been sutured closed, the temporoparietal flap is mobilised. A large paddle-shaped area of fascia is raised from the underlying temporalis muscle with care taken to preserve the pedicle. Distal branches of the superficial temporal artery are ligated as necessary.
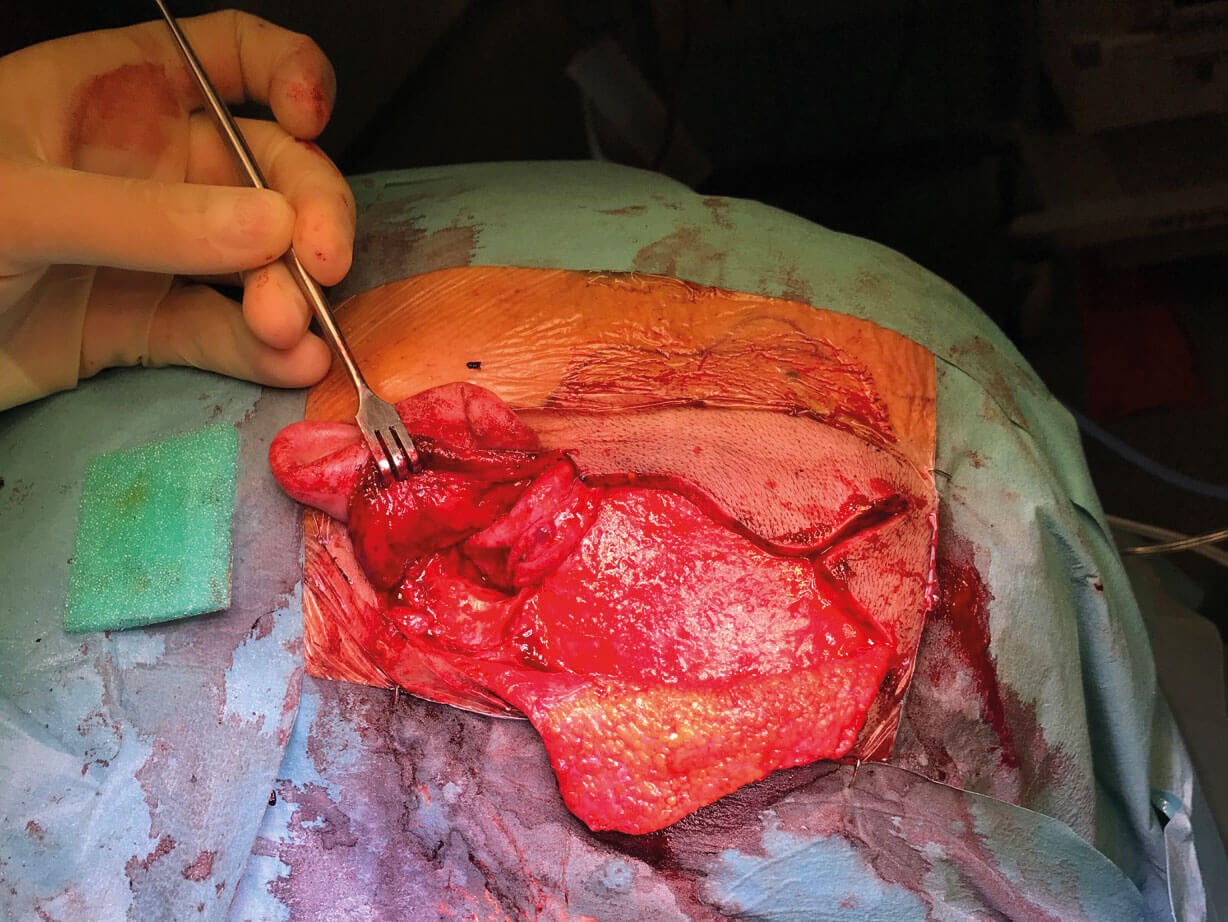
Figure 5: Picture showing the completed obliteration of the subtotal
petrosectomy with the vascularised temporoparietal pedicled flap.
The flap is then placed within the mastoid cavity to obliterate it (Figure 5). The skin is closed with staples and a corrugated drain is left for a minimum of four hours, but usually overnight, along with a pressure head bandage.
Key points
-
Blind sac closure is an effective treatment option to consider in a select number of complex chronic ears.
-
The vascularised TPF flap provides a durable and robust middle ear obliteration.
-
In-clinic/pre-op doppler probing of the STA allows for optimal surgical planning.
-
Limiting anterior dissection to the hairline is a good rule of thumb for avoiding injury to temporal branch of the facial nerve.
-
Obliteration is aided by creating as smooth a middle ear cavity as possible when drilling.
References
1. Sanna M, Dispenza F, Flanagan S, et al. Management of chronic otitis by middle ear obliteration with blind sac closure of the external auditory canal. Otology & Neurotology 2008;29(1):19-22.
2. Koziej M, Wnuk J, Polak J, et al. The superficial temporal artery: A meta-analysis of its prevalence and morphology. Clinical Anatomy 2020;33(8):1130–7.
3. Jawad BA, Raggio BS. Temporoparietal Fascia Flaps. StatPearls. Treasure Island, Florida, USA; StatPearls Publishing; 2023.
www.ncbi.nlm.nih.gov/books/NBK555905/
Last accessed January 2024.
Declaration of competing interests: None declared.







