Many of us are becoming more and more familiar with the use of transnasal oesophagoscopy. It has a number of well-described uses in the outpatient setting and is well tolerated by our patients. Yakubu Karagama describes taking this technique a step further and using it for balloon dilatation of lesions in the pharynx and upper oesophagus under local anaesthesia and in the outpatient clinic.
Transnasal oesophagoscopy guided balloon dilatation is not an entirely new invention [1,2,3,4]. This technique has been widely practised in the US, and perhaps other countries, for a number of years but it has only been in the last five years that its use is beginning to be widely appreciated among UK otolaryngologists.
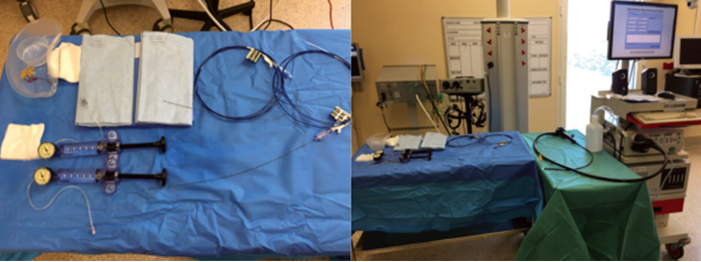
The reasons for the slow take for TNO is not known but there are suggestions that it may be due to doubts about the ability to examine the post-cricoid area fully, the cost of setting up such service and the relevant experience required. The features of the TNO – like the instrument channel, suction and insufflation buttons – the length of the TNO and the HD picture quality, has made it possible to perform a number of diagnostic and therapeutic procedures under local anaesthesia and in the outpatient set-up (see Figure 1).
Figure 1a. TNO suction & insufflation buttons.
Figure 1b. TNO 60 cm long.
Figure 1c. TNO Channel 2mm.
Indications for TNO
There are several indications for TNO. One of these is balloon dilatation. Balloon dilatation may be indicated in the management of dysphagia caused by cricopharyngeal spasm or hypertonicity, web or stricture or oesophageal ring.
Other indications for TNO are video panendoscopy (VIP), examination of the aerodigestive track, lbiopsy, insertion of nasogastric tube, tracheo-oesophageal puncture and placement of speech valve, placement of bravo capsule for PH monitoring, fibre KTP or fibre CO2 laser.
TNO guided balloon dilatation
Preoperative preparations: Full clinical history and examination is essential. The importance of patient selection based on symptoms, examination findings and diagnosis from Barium swallow (see Figure 2) and TNO findings cannot be overemphasised.
Figure 2. Barium swallow showing a thick cricopharyngeal bar as the cause of patient’s dysphagia.
Materials (see Figure 3)
- We use the Cook Medical balloon. There are different sizes of the balloon but most patients will require a 20mm size. There are other manufacturers, like Boston balloons that are suitable too.
- Cook Medical pressure pump syringe, size 60ml
- Transnasal oesophagoscope and a Videostack system (Pentax Medical). Other manufacturers like Olympus, Karl Storz and DP Medical can be use too.
- 2.5ml lidocaine HCL 5% w/v and phenylephrine HCL 0.5% w/v topical nasal spray
- 2mls of 4% lidocaine nebuliser
Figure 3. Equipment set up for TNO and balloon dilatation.
Procedure
This procedure can be performed either in the operating room or outpatient set-up with the patient sitting up at 60 degrees approximately. A good topical anaesthesia of the nasal cavities and pharynx is essential in order to complete the whole procedure successfully. This can be achieved with 2.5ml lidocaine HCL 5% w/v and phenylephrine HCL 0.5% w/v topical nasal spray into both nasal cavities and 4% lidocaine nebuliser 2mls. A mild sedation may be required in anxious and nervous patients.
A transnasal oesophagoscopy is performed to examine the larynx and pharynx. The TNO is advanced into the upper oesophagus transnasally via the most patent of the two nasal cavities. A full oesophagoscopy down to the gastro-oesophageal junction and into the stomach may be performed at this stage if necessary.
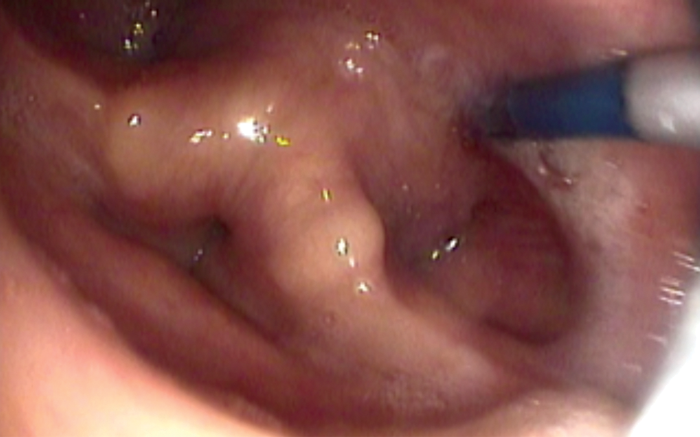
Once the TNO is placed past the cricopahrynx, a guide wire is introduced through the TNO channel until the tip of the guide wire emerges at the distal end of the TNO channel. The TNO is then withdrawn out of the patient completely while the guide wire remains in the oesophagus (see Figure 4). It is not always possible to pass the TNO through the cricopharynx especially in a very tight stricture. In such cases the TNO is placed over the piriform fossa and the guide wire introduced into the cricopharyngeal inlet under direct view. The guide wire is only about 1.5mm in diameter so it can usually be introduced through the smallest stricture unless there is a complete blockage of the stricture. In such cases, a retrograde dilatation may be necessary by introducing the guide wire and the balloon via an existing percutaneous gastrostomy (PEG) tube.
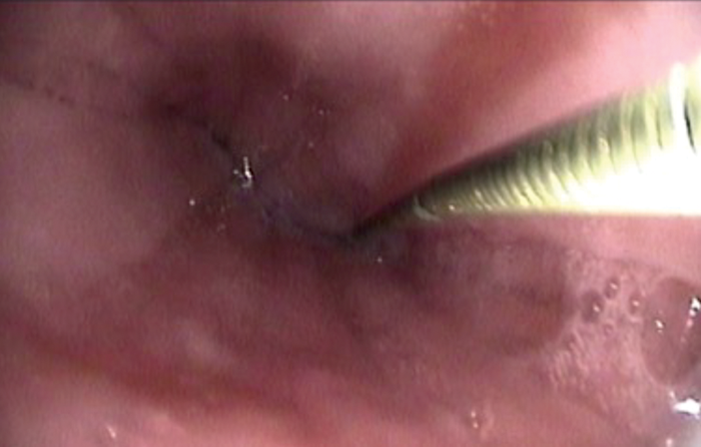
Figure 4. A guide wire inserted into oesophagus prior to balloon dilatation.
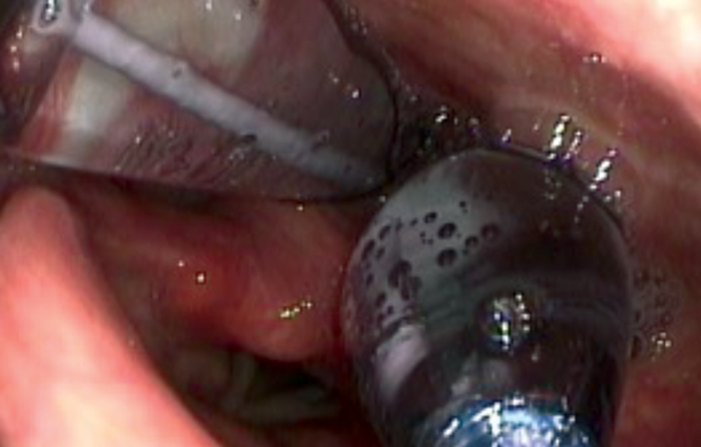
Once the tip of the guide wire is placed beyond the stricture, the TNO is reintroduced nasally via the most patent nasal cavity to visualise the pharynx during the dilatation. The uninflated balloon is then passed over the guide wire nasally until it passes through the area to be dilated. Both TNO and the balloon cables may be passed via same nostril if the other nostril is too narrow. The balloon is positioned with the proximal metallic silver marker visible just above the level to be dilated (see Figure 5). The balloon is then inflated using the pressure pump syringe until 20mm full dilatation (see Figure 6). This is then deflated after one minute and the balloon is removed with the guide wire. In some cases of webbing or cricopharyngeal bar, two 20mm balloons (40mm maximum) may be used simultaneously (see Figure 7). However, this carries a higher risk of perforation and it is more painful and, therefore, will need sedation in addition to the local anaesthesia.
Figure 5. Balloon being positioned in the cricopharynx.
Figure 6. Single balloon dilatation of a cricopharyngeal web.
Figure 7. Double balloon dilatation of a cricopharyngeal bar.
Postoperative instruction
Nil by mouth for an hour. Patient goes home same day, unless there are any complications like oesophageal tear. If such unfortunate complications occur, the patient will be managed nil by mouth until a contrast swallow test is performed to check for any of perforation.
Complications
The main significant complication is oesophageal perforation but this is rare with this technique. The reported incidence is 1-3 percent risk. Other possible complications are minor nose bleeding, throat pain, and failure of procedure to improve symptoms.
Discussion
Transnasal oesophagoscopy and balloon dilatation is now an established practice in the UK, most commonly by otolaryngologists. The use of this technique will continue to increase in the foreseeable future as the TNO equipment continues to improve in picture quality and the balloon dilatation continues to improve patient swallow. There is a need to attain certain level of training before starting this procedure to avoid failures and complications. Otolaryngologists, gastroenterologists and upper gastrointestinal surgeons with appropriate training may perform the procedure.
Conclusion
Balloon dilatation may provide a temporary or permanent cure for dysphagia, depending on the cause. Hence, it is important to warn the patient that the procedure may need to be repeated once or twice a year.
Training
A TNO Training workshop can be booked at www.phonosurgerycourse.com. It is also recommended to visit an expert to watch a live procedure. Furthermore, it is essential to visit your local endoscopy suite and to liaise closely with the radiologist, gastroenterologist and upper GI surgeons.
References
1. Howell RJ, Pate MB, Ishman SL, et al. Prospective multi-institutional transnasal esophagoscopy: Predictors of a change in management. Laryngoscope 2016;126(12):2667-71.
2. Sanyaolu LN, Jemah A, Stew B, Ingrams DR. The role of transversal oesophagoscopy in the management of globus pharyngeus and non-progressive dysphagia. Ann R Coll Surg Engl 2016;98(1): 49-52.
3. Abu-Nader L, Wilson JA, Paleri V. Transnasal oesophagoscopy: Diagnostic and management outcomes in a prospective cohort of 257 consecutive cases and practice implications. Clin Otolaryngol 2015;40(2):167.
4. Gollu G, Ates U, Can OS, Dindar H. Balloon dilatation in esophageal strictures in epidermolysis bullosa and the role of anesthesia. Dis Esophagus 2016.