In this How I Do It, Professor Sergei Karpischenko introduces a gentle method of reduction of mobilised frontal sinus osteoma which has been successfully used in five patients in his university clinic using a diode laser in contact mode.
Osteoma is a benign bone lesion which commonly occurs in the upper and lower extremities, flat and tubular bones, jaw and paranasal sinuses. It usually originates from the frontal (80%) and ethmoid (15%) sinuses. This tumour is rarely found in the maxillary (5%) and sphenoid (1%) sinuses [1].
Osteoma can be classified as single or multiple. Bone masses over 30mm in diameter or weighing more than 110g are regarded as giant (or large). Osteoma is divided into the following histological types: compact (ivory), mature (spongeous) and mixed, which includes features of both the former types [2]. Rarely, bone marrow can be found inside the osteoma, and such tumours are known as medullary. Aetiology of such tumours is unknown, however there are several theories of their origin, including trauma, infection, embryologic, etc.
Osteoma is a slow-growing encapsulated tumour, which is usually asymptomatic [3]. When the bone tumour begins to grow above the ranges of the sinus into the adjacent structures, it compresses soft tissue and damages surrounding anatomical structures. Depending on osteoma location, the patient’s symptoms include facial pain or deformity, diplopia, vision deterioration and other ophthalmological and neurological disorders. The most common symptom of osteoma is a headache. Bone tumour may be accompanied by polyposis and other rhinosinusitis.
Small tumours are usually accidental findings when CT or MRI scans are performed for other pathologies [4]. The bone mass of a very intense, uniform density with distinct contours is determined in CT or MRI scans. Such osteomas can be observed for the follow-up period, if there are no symptoms and they are not located in a sinus ostiae.
“Small tumours are usually accidental findings when CT or MRI scans are performed for other pathologies. The bone mass of a very intense, uniform density with distinct contours is determined in CT or MRI scans. Such osteomas can be observed for the follow-up period, if there are no symptoms and they are not located in a sinus ostiae.“
Only surgical treatment is indicated. The type of surgery depends on the size, anatomic localisation and dimension of the mass and includes three approaches: open, endoscopic and combined. In case of osteoma growing on the roof agger nasi or frontal bulla, the frontal sinus cannot be opened endoscopically without osteoma mobilisation. Mobilised osteoma can be removed only after endoscopical wide sinus opening, with Draf III procedure or with the open approach. In both cases non-pathological bone tissues should be removed. Another possibility for successful resolution of this difficult situation is to destroy mobile bone tumour inside the sinus. Motor systems or forceps cannot be applied, because of osteoma ‘run-away’ from the instrument. We successfully used diode laser for osteoma size reduction in the nose, as described in this article.
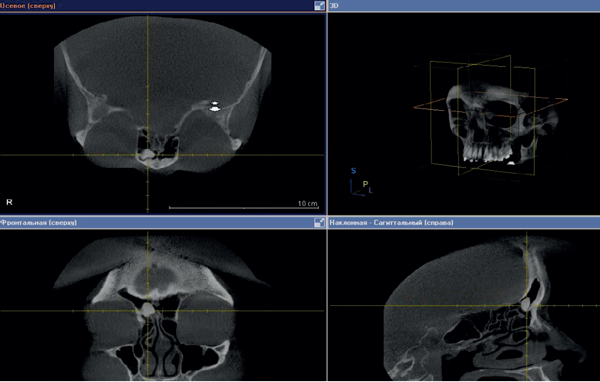
Figure 1: CT scan before surgery – right frontal sinus osteoma.
In January 2013, a 56-year-old woman presented at the ENT Department of First Pavlov State Medical University of St Petersburg, with discomfort in the right eye and right frontal sinus. These symptoms had occurred since 2011. The patient had been diagnosed with arterial hypertension. She had normal clinical analysis of blood and urine. Examination of the nose and nasopharynx with different endoscopes (0°, 30°, 45°) showed pink and moderate swelling nasal mucosa, nasal septum on midline. There was no pathological content on both sides of the nasal passages. CT scan of the paranasal sinuses revealed bone density tumours (1.0*1.5*1.0 cm) in the right frontal sinus with clear contours (Figure 1). The patient was advised to undergo surgical treatment.
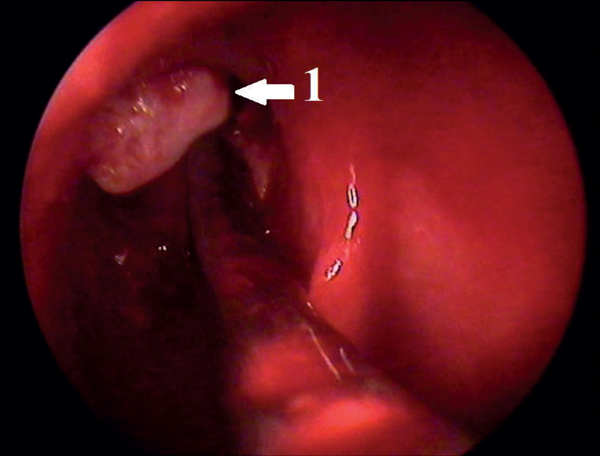
Figure 2: Endoscopic view: 1 – mobilised frontal osteoma.
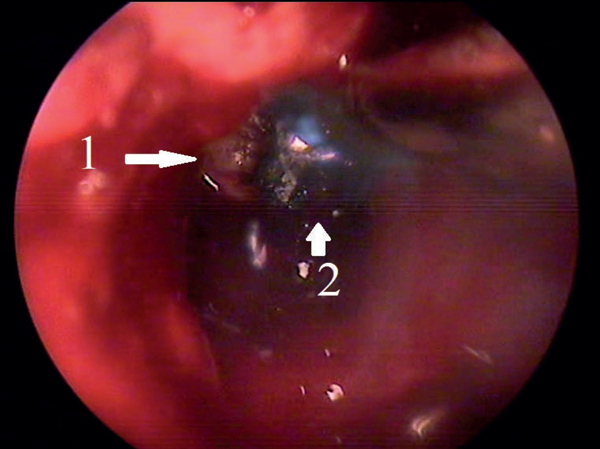
Figure 3: Endoscopic view: 1 – frontal osteoma; 2 – diode laser.
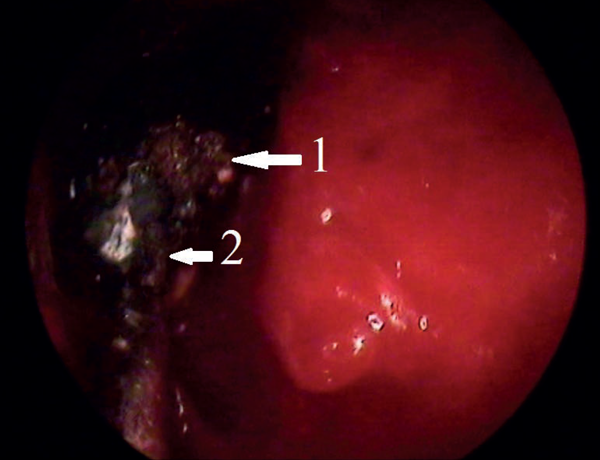
Figure 4: Endoscopic view: 1 – reduced frontal osteoma; 2 – aspirator.
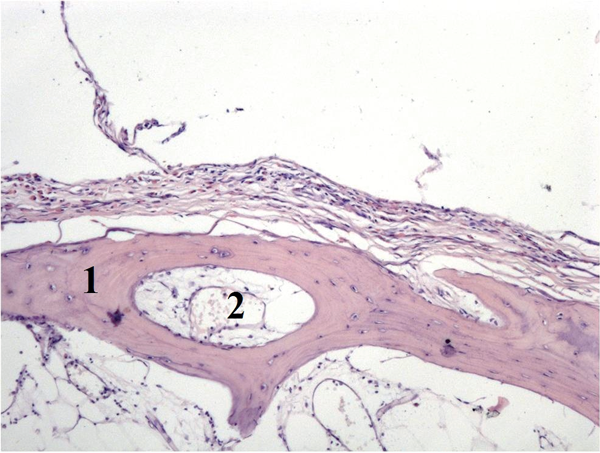
Figure 5: Histological examination: mixed osteoma (1 – trabeculae; 2 – fibrous tissue, collagen fibres).
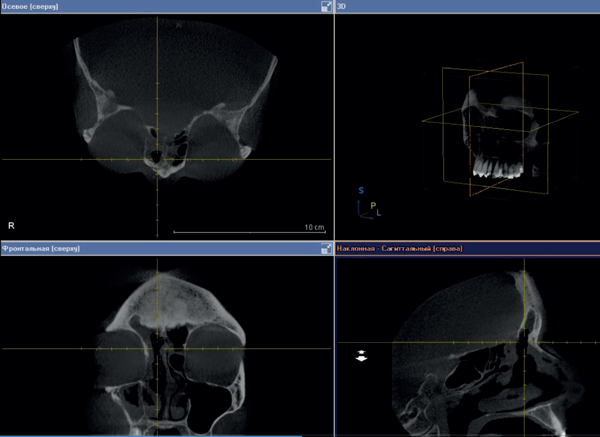
Figure 6: CT scan of paranasal sinuses three days after surgery.
She was informed beforehand that in case of failure of the endoscopic surgery the tumour would be removed by an open coronal approach. In January 2013 the osteoma was removed under general anaesthesia and controlled hypotension with endoscopic control using a 3D electromagnetic navigation system via endonasal approach. After the tumour was mobilised into the sinus cavity (Figure 2), reduction of its size was necessary to release it from the sinus. Mobilised osteoma was reduced by diode laser applied in contact mode (power 10 W) (Figure 3) and then removed through the nasal cavity (Figure 4). Vaporisation of mobilised bone tumour was held around its circumference with exposure time of 8-10 seconds. When it reached a sufficient size for removing through the expanded frontonasal ostiae, it was extracted by an aspirator. Histological examination showed a mixed osteoma, containing dense and mature bones, fibrous tissue and collagen fibres (Figure 5). A right eyelid oedema was in the early postoperative period. This situation was not accompanied by damage of the optic nerve and violations of the mobility of the eyeball. Systemic antibiotic therapy, glucocorticoids and diuretics were initiated immediately and eyelid oedema passed off within two days. The control CT scan on the third day after surgery showed complete removal of tumours (Figure 6). The patient was transferred to out-patient treatment on the seventh day after surgery. We recommended the use of topical steroids and ENT and ophthalmology dynamic observation.
The endoscopic approach has some limitations and difficulties. Contraindications for endonasal removal reduce from year to year. The first limitation is insufficient surgical experience of the operating surgeon. Endoscopic frontal sinus osteoma removal is one of the most difficult procedures in FESS. Other limitations include lateral osteoma position and huge size of the tumour (giant osteoma). Evolution of methods and instruments can also reduce these limitations. Some difficulties can be detected intraoperatively, which is why the patient must be informed about the possibility of external approach in case the endoscopic procedure is not effective.
In summary, we would like to discuss technical difficulties during osteoma removal, such as extraction of the mobilised tumour inside the sinus cavity. In order to remove such a mobile osteoma the surgeon needs to perform a wide window, destruct the tumour inside the sinus or apply an external approach. Intranasal laser-assisted osteoma destruction prevents soft tissues and bony structures from damage. Endoscopic tumour removal is preferable due to minimal trauma and the absence of cosmetic defects. Timely surgical treatment with endoscopic approach allows removal of the bone tumour completely, preventing the occurrence of adverse consequences. Our experience shows the perspectives of laser application in endoscopic endonasal osteoma removal.
References
1. Torun MT, Turan F, Tuncel Ü. Giant ethmoid osteoma originated from the lamina papyracea. Medical Archives 2014;3:209-11.
2. Satyarthee GD, Suri A, Mahapatra AK. Giant spheno-ethmoidal osteoma in a 14-year boy presenting with visual impairment and facial deformity: short review. Journal of Pediatric Neurosciences 2015;10:48-50.
3. Batra N, Batra R, Singh G, Gaur A. Peripheral osteoma of maxilla: a case report. National Journal of Maxillofacial Surgery 2014;5:240-2.
4. Gotlib T, Held-Ziółkowska M, Niemczyk K. Frontal sinus and recess osteomas: an endonasal endoscopic approach.
B-ENT 2014;2:141-7.
Declaration of competing interests: None declared.




