Dr Georgiou’s summary of the 2020 update to the 2017 Lancet Commission underscores the importance of medical and hearing healthcare professionals working together to tackle the modifiable risk factors that affect individuals throughout their lives, to help delay or even prevent the onset of dementia.
The 2020 Lancet Commission on dementia prevention, intervention and care identified 12 potentially modifiable risk factors for dementia. The risk factors include: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, low social contact, excessive alcohol consumption, traumatic brain injury and air pollution. The report estimates that modifying these risk factors might prevent or delay 40% of dementia cases worldwide [1] (Figure 1).
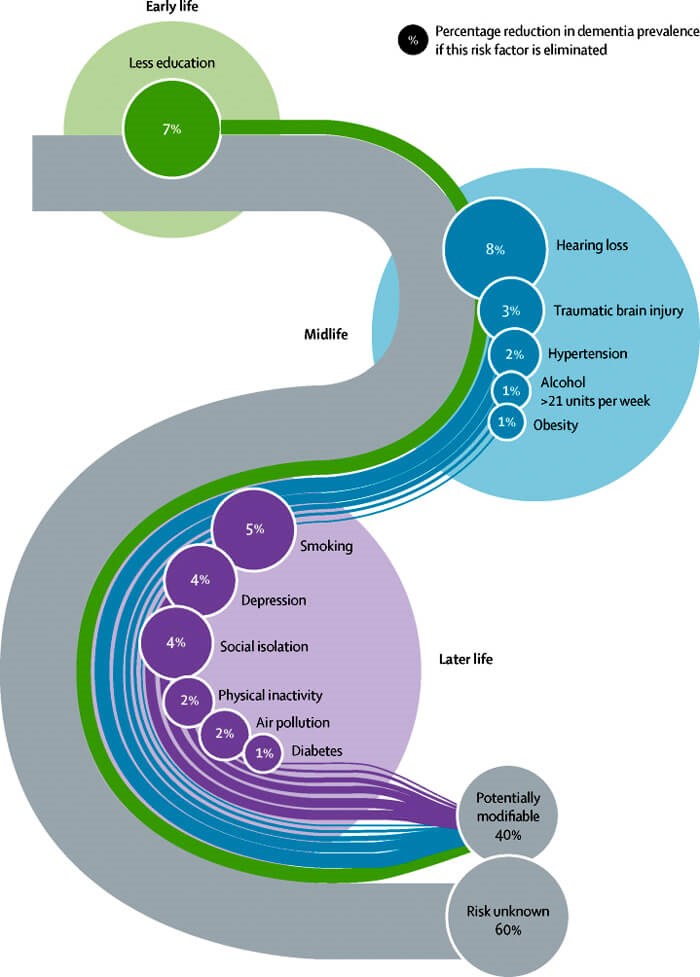
Figure 1. Population attributable fraction of potentially modifiable risk factors for dementia.
Reprinted from the Lancet Commission on Dementia with permission from Elsevier [1].
Hearing impairment is the largest contributor to the Commission’s risk reduction model and represents 20.5% (8.2 points) of the modifiable opportunity. While sensory deprivation is believed to be one of the mediating pathways between hearing loss and cognitive impairment, neither causality nor reversality have been definitively established. However, as a strategy to advance policies and practices that support risk factor reduction, the Commission boldly used high-quality evidence to implicate a causal relationship and explicitly recommends using hearing aids to prevent, slow down the progression, or reverse cognitive decline.
“Hearing impairment is the largest contributor to the Commission’s risk reduction model and represents 20.5% (8.2 points) of the modifiable opportunity”
Besides identifying hearing loss as an important modifiable risk factor for dementia, the Commission’s model reinforces the importance of a coordinated approach to patient care. At least four other risk factors in the report are strongly associated with hearing loss and potentially mediated by sensory deprivation.
These include:
- Depression: Deal, et al used administrative claims data to show that hearing loss was independently associated with a 3.2 times greater risk of depression in adults 50 years or older, over 10 years [2].
- Low social contact: a systematic review of five cross-sectional studies of social isolation found that older adults with hearing loss were more likely to be socially isolated [3] with women ages 60-69 years having 3.5 times higher risk [4].
- Traumatic brain injury (TBI): falls are the leading cause of traumatic brain injury and cause 81% of TBI-related emergency room visits in adults 65 years or older. Lin, et al found that people with a 25-decibel hearing loss were nearly three times more likely to have a history of falling, and every additional 10-decibels of hearing loss increased the chances of falling by 1.4-fold [5].
- Physical inactivity: compared to those with normal hearing, individuals with moderate or greater hearing impairment had a 59% increased odds of having lower levels of self-reported physical activity and a 70% increased odds of having lower levels of accelerometer-measured physical activity [6].
Collectively, these four risk factors account for 31% (12.4 points) of the modifiable risk, and at least a portion of this additional opportunity is captured when hearing loss is treated (Figure 2).
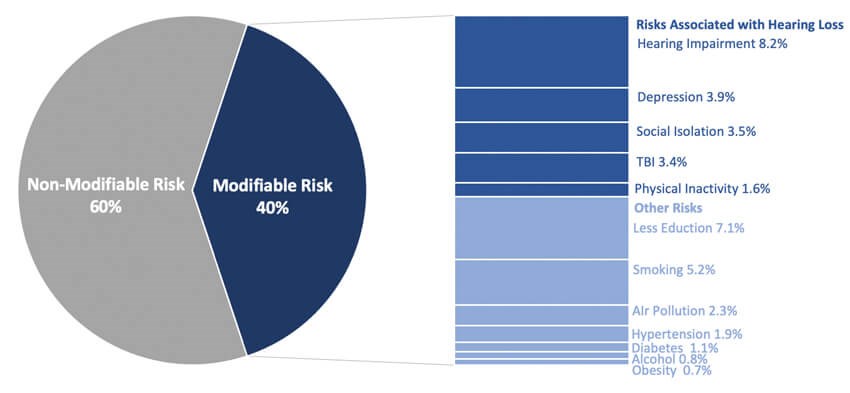
Figure 2. Modifiable risk factors associated with hearing impairment.
Adapted from the Lancet Commission on Dementia [1].
While primary care providers typically have the earliest insight to patients with mental health and social issues, gait instability, fall risk, physical inactivity and other symptoms and risk factors, they infrequently suspect hearing loss. Conversely, audiologists may have insights regarding patients’ early challenges with cognition, communication and engagement and balance but infrequently take action to coordinate follow-up medical evaluation with the primary care provider. The 2020 Lancet Commission is a call to action for medical and hearing professionals to design and implement integrated and bi-directional referral and care processes to decrease the risk of dementia.
“The Commission boldly used high-quality evidence to implicate a causal relationship and explicitly recommends using hearing aids to prevent, slow down the progression, or reverse cognitive decline”
References
1. Livingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020;396(10248):413-46.
2. Deal JA, Reed NS, Kravetz AD, et al. Incident Hearing Loss and Comorbidity: A Longitudinal Administrative Claims Study. JAMA Otolaryngol Head Neck Surg 2019;145(1):36-43.
3. Shukla A, Harper M, Pedersen E. Hearing Loss, Loneliness, and Social Isolation: A Systematic Review. Otolaryngology–Head and Neck Surgery 2020;162(5):622-33.
4. Mick P, Kawachi I, Lin F. The Association between Hearing Loss and Social Isolation in Older Adults. Otolaryngology–Head and Neck Surgery 2014;150(3):378-84.
5. Lin F, Ferrucci L. Hearing loss and falls among older adults in the United States. Arch Intern Med 2012;172(4):369-71.
6. Gispen F, Chen D, Genther D, Lin F. Association between hearing impairment and lower levels of physical activity in older adults. J Am Geriatr Soc 2014;62(8):1427-33.
Declaration of Competing Interests: Archelle Georgiou is employed by Starkey.





