Rilana Cima and Haúla Haider introduce an ambitious pan-European collaboration that seeks to establish guidelines for achieving best clinical practice for managing, assessing and treating patients with different tinnitus profiles.
Tinnitus heterogeneity is the major reason for inconsistent results in tinnitus studies and is the major barrier in developing innovative and more efficient treatments for tinnitus. The main objectives of WG1 are to develop harmonised and adaptive clinical guidelines for the management, assessment and treatment tinnitus patients and to develop guidelines for detailed clinical definition and characterisation of tinnitus.
Tinnitus is a widespread auditory symptom [1]. It is a highly complex condition with a multifactorial origin, and therefore heterogeneous patient-profiles, standard treatment, assessment and referral-trajectories are rare, inflexible and often insufficient. There is increasing need for European harmonised guidelines for demographic and clinical assessment of tinnitus sufferers, since a lack of standard guidelines, leads to untreated, under-, as well as over-treated patients. This leads to increasing complaints, prolonged suffering, loss of societal participation, health care overuse and endless referral trajectories, resulting in enormous psychological, societal and economic burden in Europe [2].
“There is a need for European harmonised guidelines for demographic and clinical assessment of tinnitus.”
Through development and implementation of European guidelines, we anticipate that management, assessment and treatment of tinnitus will be significantly more effective, leading to reduced suffering and frustration for patients, their families and clinicians alike.
The main goal of this working group is to establish uniformity with regards to management, assessment and treatment of patients with different tinnitus profiles. In addition, we aim to establish consistency in policy regarding referral trajectories, thereby decreasing the need for multiple second opinions, and over- and under-diagnostics and treatment. Guidelines for detailed clinical definition and characterisation of cases will also be developed. Experts from different disciplines across Europe have joined forces to further develop standardisation procedures for easy, practicable and meaningful patient-profiling.
“A set of guidelines will establish uniformity with regards to management, assessment and treatment of patients with different tinnitus profiles.”
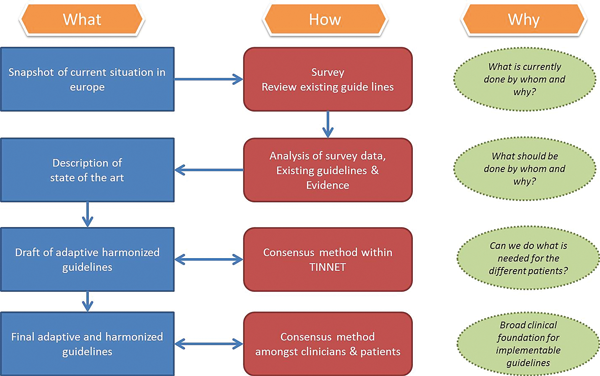
Figure 1: The RoadMap describing activities planned within WG1 to develop clinical guidelines.
A RoadMap describing our activities is shown in Figure 1. The first step towards the development of meaningful and actionable guidelines for the assessment and treatment of tinnitus patients will involve a pan-European survey amongst experts, clinicians and policy makers to investigate current standards in tinnitus care. This will lead to an updated description of ‘best practice’ in standard care in Europe [3]. The second step is to review existing guidelines internationally, including but not limited to Europe alone. Thirdly, best practice in clinical assessment of tinnitus (meaningful patient characterisation) and treatment options will be described. Results from the survey, as well as the review of existing guidelines and best practice in assessment and treatment, will be used to develop an initial draft description of a set of European guidelines. Finally, using Delphi consensus methodology, we aim to achieve harmonised and adaptive clinical European guidelines for the management, assessment and treatment of tinnitus patients.
References
1. Martinez C, Wallenhorst C, McFerran D, et al. Incidence rates of clinically significant tinnitus: 10-year trend from a cohort study in England. Ear and Hearing 2015;36(3):e69-e75.
2. Maes IH, Cima RF, Vlaeyen JW, et al. Tinnitus: a cost study. Ear and Hearing 2013;34(4):508-14.
3. Langguth B, Goodey R, Azevedo A, et al. Consensus for tinnitus patient assessment and treatment outcome measurement: Tinnitus Research Initiative meeting, Regensburg, July 2006. Progress in Brain Research 2007;166:525-36.
ABOUT THE AUTHORS
During the past 10 years, Rilana has specialised in the measurement, diagnostics, treatment and cognitive-behavioural mechanisms of tinnitus. National challenges in policy and legislation in tinnitus-healthcare within the Netherlands have called for active discussion between disciplines, legislators, policymakers and insurance companies about the diagnostics, treatments and non-existing standards in tinnitus healthcare and research. Rilana represents the Netherlands on the TINNET Management Committee and is chair of WG1. Haúla completed her internship in otolaryngology (ENT) at the Hospital Pulido Valente in 1999 and she has been a consultant specialising in tinnitus since 2002 at the Hospital Cuf Infante Santo. She represents Portugal on the TINNET Management Committee and is co-chair of WG1.
Declaration of competing interests: None declared.





