The words ‘choice and competition’, ‘any qualified provider (AQP)’ and ‘accreditation’ have irrevocably become part of audiology jargon in the last two years in England. Commissioners who chose ‘Adult Hearing Aid Services for age-related hearing loss’ have begun the process of driving competition between private and National Health Service (NHS) providers [1-3].
Until recently, the NHS has traditionally been the sole provider of free hearing aids to patients, but the introduction of AQP has forced a new pace of change requiring patients to be assessed within 21 days and fitted rapidly with digital aids.
In an era of quality performance targets, the role of leaders to lead effectively, efficiently and drive change has never been more important to meet new demands [4-6] and offer a new perspective that we now face more unpredictable circumstances this century, suggesting that it is even more essential to recognise changing trends and for managers to develop resilience to change.
Understanding the framework of IQIPS and accreditation
Accreditation of AQP was proposed to be the quality improvement and assurance measure to ensure adherence to national standards of practice, but to date (July 2014) only 16 services have been accredited in England. In my role as Deputy Head of audiology, I was assigned as project lead for accreditation at The Shrewsbury and Telford Hospitals NHS Trust.
It was a huge task, resulting in many hours of work, requiring determination and drive, attention to detail, a team effort and a full systems analysis. However, once we got the accreditation certificate there was a sense of pride and achievement.
The first part of the Improving Quality In Physiological Service (IQIPS) Programme is the self-assessment online tool (SAIT), which requires the service to answer a series of key statements with yes / no / not applicable and to address any identified weaknesses. Level B needs to be achieved before proceeding to the United Kingdom Accreditation Service (UKAS) accreditation process [7, 8]. Self assessment is only the start of the accreditation journey, together with the different costings for each element of self assessment, then accreditation web-based assessment and visit, which is sometimes a cause for confusion.
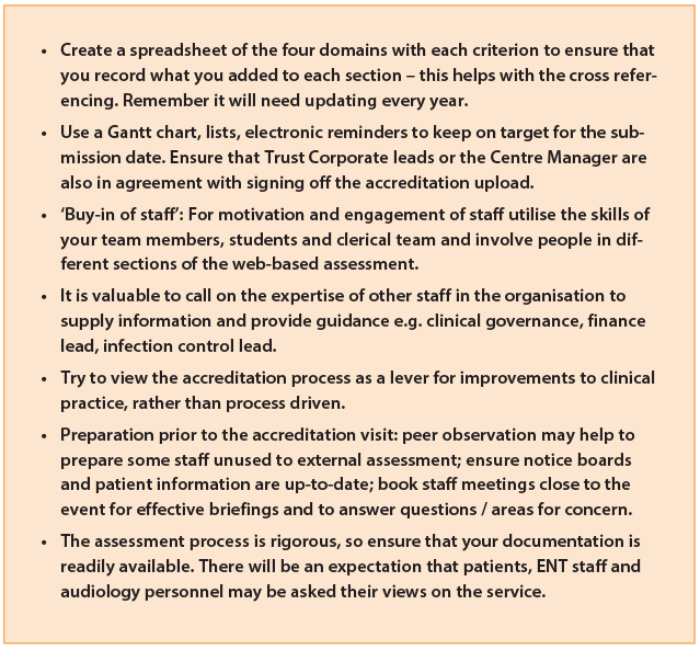
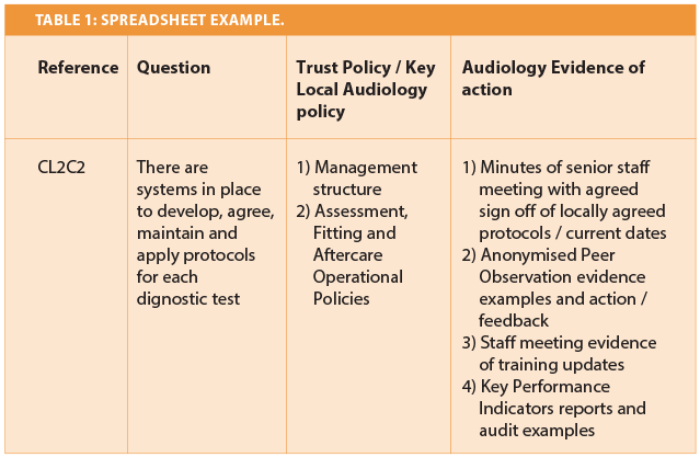
If you are starting on the accreditation process my top tip is: remember that for every yes answer, you will need to supply relevant evidence at the next stage of accreditation. Start collating electronic evidence early e.g. staff meeting minutes, learning outcomes from complaints and datix incidents, training and development plans, risk assessments, peer competency observations, photos of facilities, scanned signatures of key policy documents. Keep your personal files according to your trust policy. Finding implementation examples and monitoring mechanisms across a 150 quality criteria, together with ensuring careful cross referencing was a daunting task.
There are four domains, which cover every aspect of a department’s functioning:
- Patient Experience e.g. dignity and respect, patient information and feedback, complaints system
- Facilities and workforce e.g. budgeting, capacity and demand planning, business planning, procurement, quality of the testing environment
- Patient Safety e.g. local governance arrangements, risk and Control of Substances Hazardous to Health (COSHH) assessments, infection control, lone working procedures
- Clinical Section e.g. referral processes, audit evidence, peer observation, key performance measures, local operational policies based on national recommended procedures, referral monitoring.
NHS providers can also get accredited for complex work including tinnitus, vestibular and paediatric services. Clear standards and specific examples of what evidence the assessors expected were useful within the web-based tool, but can only be viewed once payment and access to the website has been approved. Preparing for accreditation was a source of stress, whilst trying to balance the day job and the usual clinical demands.
Once I entered the accreditation website, the size of the task became apparent. It needs a designated person to lead the project, time away from clinical work and a team of people to source relevant evidence. Trust policies and departmental procedures need uploading with the correct review dates, but what is important is how you evidence that all your staff follow the policies to provide a good quality patient service.
Figure 1: Top tips for the accreditation leader.
Motivation, engagement and teamwork
A positive outcome of accreditation is that it has raised the profile of audiology within the Trust and was an effective lever for facilities improvements. It could be proposed that external assessment drove the pace of change and drive for quality, which was a core objective of the accreditation process [7]. The domain on workforce highlighted the importance of investment in leadership skills requiring demonstration of business planning, effective people management, financial awareness, stock management mechanisms and clear processes for calibration.
At the heart of the matter is the key question of whether ‘choice and competition’ has achieved greater access, shorter waits and most importantly a quality hearing aid service to improve the lives of patients with a hearing loss. Accreditation provides one monitoring mechanism to evaluate the impact of AQP, but it is important to also consider patient groups and commissioners. Now the organisation ‘Monitor’ is currently collating opinion on the impact of AQP and evaluating the cost. In conclusion, it could be proposed that it is essential to develop new ways of thinking and empower line managers and frontline staff to sustain improvements to be better prepared for the future [9, 10]. Equally, it is important for audiology departments to be politically aware of commissioning intentions, technological advances making sure they utilise the expertise within trusts to work towards a cohesive strategy for change and improvement.
References
1. Cavanagh, C. 2012. Any Qualified Provider: Where are we now?
http://www.baaudiology.org/files /8813/5898/
2762/BAA-AQP-Info-Day-CC-and-AD-Slides-v3.pdf
Last accessed July 2014.
2. Department of Health (2010). Impact assessment : Extension of Any Qualified Provider. IA No. 2026. https://www.gov.uk/government/publications/
extension-of-any-qualified-provider-impact-assessment
Last accessed July 2014.
3. Action on Hearing Loss (2013). Extending Patient Choice to Any Qualified Provider.
http://www.actiononhearingloss.org.uk/
supporting-you/policy-research-and-influencing/
policy/ policy-statements/health-and-social-care.aspx
Last accessed July 2014.
4. Marr B, Creelman J. More with Less: Maximising Value in the Public Sector. Basingstoke, UK; Palgrave Macmillan; 2011.
5. NHS Change Model (2013). NHS Change Model: Everything we know about delivering change in the NHS, all in one place. http://www.changemodel.nhs.uk/
pg/dashboard
Last accessed July 2014.
6. Eoyang G, Holladay R. Adaptive Action: Leveraging Uncertainty in your Organisation. California, USA; Stanford University Press; 2013.
7. IQIPS (2013).
https://www.iqips.org.uk/documents/new/
IQIPS%20Standards%20and%20Criteria.pdf
Last accessed July 2014.
8. United Kingdom Accreditation Service (2014). IQIPS Standards - Accredited Services.
http://www.ukas.com/about-accreditation/
accredited-bodies/IQIPS_Schedules.asp
Last accessed July 2014.
9. The King’s Fund (2012). Leadership and Engagement for Improvement in the NHS: Together We Can. http://www.kingsfund.org.uk/publications/
leadership-engagement-for-improvement-nhs
Last accessed July 2014.
10. Lewis S. Positive psychology at work: how positive leadership and appreciative inquire create inspiring organisations. Chichester, UK; Wiley-Blackwell; 2011.
Declaration of Competing Interests: None declared.