Abi Asher, Clinical Lead for the IAD programme in Cambridge describes how hearing care professionals work together to make the best recommendation for the patient, in turn helping navigate through the various devices now on offer.
Multidisciplinary teams (MDTs) are a familiar concept within many medical fields, including hearing implants. Implantable acoustic devices (IADs) include passive and active bone conduction hearing devices (BCHDs), and middle ear implants (MEIs), and are manufactured by the same companies that also provide cochlear implants (CI).
BCHD professionals have a history of multidisciplinary consensus statements that set out future plans and have impacted on the course of NHS England Commissioning guidelines [1], but a shorter history of offering an MDT assessment. The 20 centres that offer CI in the UK, some of which offer IADs, have a long history of MDT working and typically have representation from ENT surgeons, nurses, speech and language therapists, audiologists, teachers of the deaf, psychologists and hearing therapists. By contrast, audiology departments, some of whom offer IADs, are not funded to provide the same breadth of multidisciplinary assessment of hearing. They do, however, show a range of interdisciplinary working with ENT services, paediatrician aetiological investigations, local speech therapy and education services, cleft and oncology teams, and newborn hearing screening, depending on the services they provide.
“The MDT approach is considered a gold standard of care”
The MDT approach is considered a gold standard of care. Literature from MDT in ENT settings appears sparse but in other fields, MDT working is documented to be associated with changes to diagnosis, management plans and adherence to clinical guidelines [2].
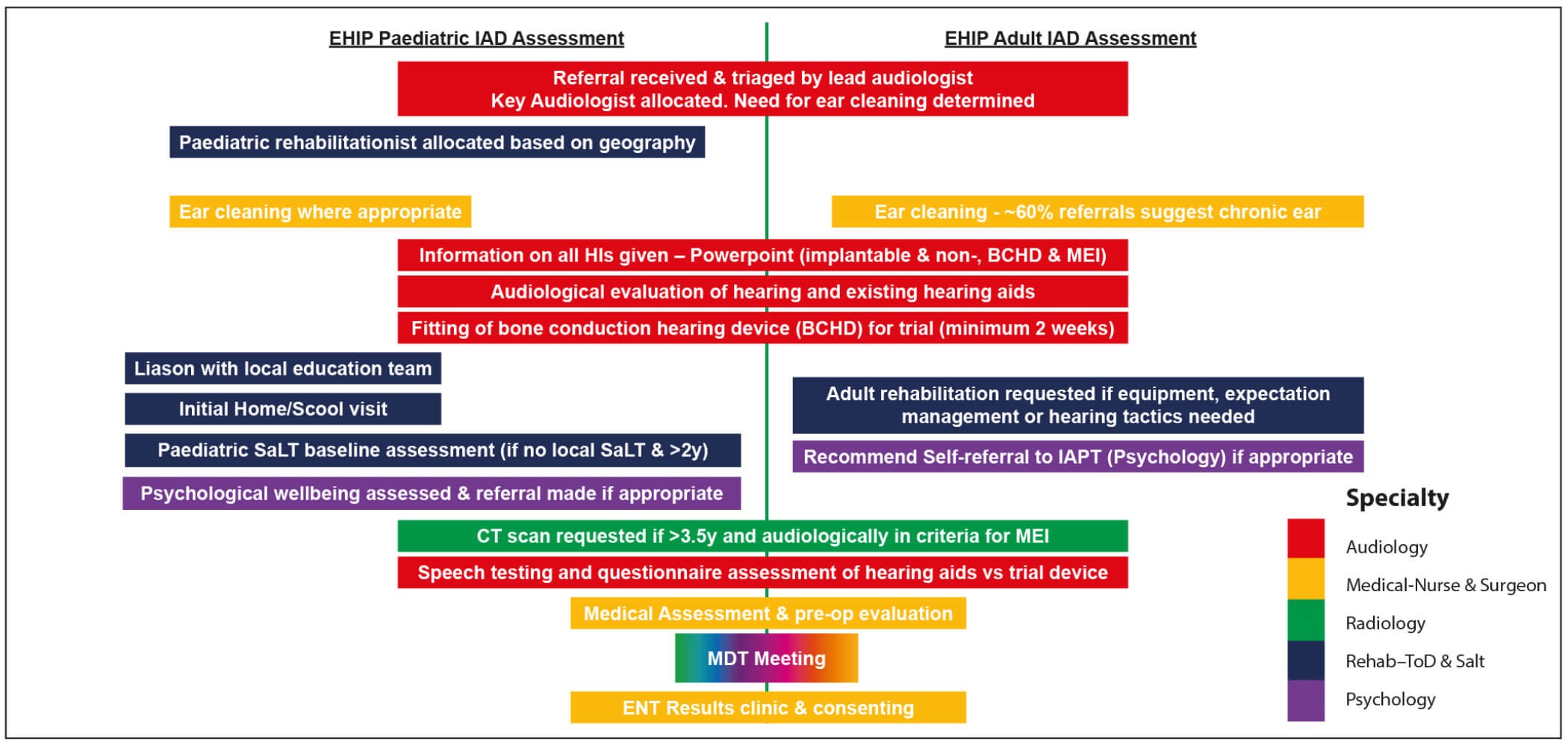
Figure 1: EHIP MDT Assessment process.
Since 2013, the 110+ hearing implant and audiology teams who provide implantable acoustic devices have also been required by NHS England to offer a ‘comprehensive assessment by a specialist multi-disciplinary team’ [3]. The revised NHS commissioning policy from 2016 continued to specify this MDT approach [4]. Neither commissioning guideline specifies the makeup of an MDT, and so many are comprised of only audiological and medical specialties.
At the Emmeline Hearing Implant Programme (EHIP) in Cambridge, patients referred for IADs have undergone a multidisciplinary approach since the 1990s. Initially this involved medical and audiological assessment but, over time, the benefits of broader MDT expertise has led to inclusion into the MDT meeting (previously purely CI), routine paediatric rehabilitationist intervention, radiology for consideration of MEI, and case-by case addition of psychology and adult rehabilitation input. IAD assessments are undertaken by the same MDT that undertakes CI assessments, so there is a broad range of knowledge, skills and experience to draw upon.
Since an MEI programme was added to the bone conduction programme in 2010, all referrals received from ENTs, audiologists, GPs, paediatricians or Teachers of the Deaf have been assessed by the MDT for all IAD types, regardless of request on the referral.
“IAD assessments are undertaken by the same MDT that undertakes CI assessments, so there is a broad range of knowledge, skills and experience to draw upon”
We consider that MDT assessment combines expertise and experience in a range of fields, giving a holistic patient approach that is most likely to give the correct decision. Benefits include:
- Combining previous professional experience in each specialty.
- Complementing experience of hearing implants between specialties (objective audiological tests + outcome measures + functional performance outside clinic + psychological ability to make best use of an implant).
- MDT assessment is less likely to miss the needs of the patient as there is continuous assessment flowing between the different specialties.
- Paediatric support from implant experts when local funding is tight and tends to be directed towards the CIs.
- Efficient within-specialty communication, training and support for local professionals (e.g. implant SaLT to local SaLT).
MDT meeting
EHIP runs a fortnightly MDT meeting attended by all clinical members of the team except psychology and radiology, for whom reports are available at the meeting. Each patient case is added to the MDT agenda at the request of clinicians. There are a variety of weekly review meetings designed to allow case discussions between members of the MDT. The patient specifics are verbally presented by the key audiologist who prepares a written template on our electronic medical record system, which is projected for the whole team. The MDT template includes information about aetiology, ear health, hearing tests, speech results, known medical conditions and a list of implants that the patient meets criteria for, with preference given depending on patient-specific factors. The scans are pre-reviewed by a member of the surgical team, and the nurse and rehab teams review their visit notes, ready to add to the discussion. All members of the team, regardless of whether they are the ‘key’ clinicians, contribute to the discussion about each patient and come to an MDT consensus about which device should be offered. The patient is offered this device by the consultant ENT surgeon at a clinic within three weeks.
“Consistency might be best achieved by having a standard of care for makeup of the MDT”
Cases are split into those ready for implant decision, needing discussion (and therefore likely more assessment after MDT), and those being discharged. Cases for discharge, either by patient choice or being out of criteria, are brought to the MDT for transparency, learning and discussion as needed, and to initiate a discharge by letter if appropriate.
The MDT meeting benefits include:
- Encouraging routine peer review - multiple professionals from the same speciality give robust review of each element of the MDT assessment (audiologists from different backgrounds reviewing each other’s work).
- Unrecognised bias can be challenged (e.g. preference for one device).
- With a crossover in candidacy, MDT meetings allow open discussion of pros and cons of possible recommend devices.
- Giving consistency to a decision-making process where more than one implant is suitable.
Ongoing use of the MDT
In Cambridge, the MDT approach continues after implantation. Patients are made aware of their pathway and additional support is made available, so that they and local professionals can be empowered to request intervention if needed.
The future of MDT assessment for IADs is assured. Not least, it is an NHS requirement for teams providing IADs, but the benefits are well documented in the literature for other disciplines [2]. The methods of delivering MDT input postoperatively may change with remote care and resources available through electronic devices, but the principles of MDT working will be embedded.

The Hearing Implant MDT.
One future issue is providing equality of care across IAD teams. Consistency might be best achieved by having a standard of care for makeup of the MDT. The future of MDT meetings is moving towards a telemedicine approach [5]. Issues of IT and information governance within the NHS are significant but not insurmountable and might facilitate hub and spoke models of care.
There is also future scope for having an Audiology ‘IAD Champion’, akin to the current movement towards ‘CI Champions’, who could further increase awareness of an MDT assessment and reduce IAD postcode inequality.
References
1. Hill P, Norman G, Davison T, et al. Adult bone anchored hearing aid services in the United Kingdom: Building a consensus for development. Cochlear Implants International 2013;13(4):228-36.
2. Pillay B, Wootten A, Crowe H, et al. The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: A systematic review of the literature. Cancer Treat Rev 2016;42:56-72.
3. NHS Standard Contract (2013) For Implantable Hearing Aids for Microtia, Bone Anchored Hearing Aids and Middle Ear Implants (all ages). NHS England/ D09/S/b.
4. Clinical Commissioning Policy (2016): Bone conducting hearing implants (BCHIs) for hearing loss (all ages). NHS England: 16041/P.
5. Aghdam M, Vodovnik A, Hameed R. Role of Telemedicine in Multidisciplinary Team Meetings. J Pathol Inform 2019;18(10):35.
Declaration of Competing Interests: None declared.




